Abstract
Angiogenesis, the process of new blood vessel formation, is a complex phenomenon that plays a crucial role in various physiological and pathological processes, including embryonic development, tissue repair, vascular homeostasis, and tumor microenvironments. The utilization of human in vitro and ex vivo models to study angiogenesis is an actively investigated area that holds great promise for offering novel insights and prospects for developing methods to treat angiogenesis-related diseases, such as cancer and cardiovascular disorders. Combining in vitro and ex vivo models using human samples can enhance the understanding of the complex process of angiogenesis in the human body. This integrative strategy facilitates a holistic exploration of angiogenesis, bridging the gap between simplified in vitro systems and the complexities inherent in in vivo settings, thereby augmenting the translational prospects of research outcomes for clinical applications. However, ethical constraints, inherent individual variability in human samples, challenges in obtaining tissue samples, technical issues in tissue handling, and the high cost involved are key limitations to consider.
Introduction
Angiogenesis is the process of forming new capillaries from pre-existing blood vessels and plays a pivotal role in various normal physiological processes, including embryonic growth, tissue repair, and the maintenance of vascular homeostasis1. While pathological angiogenesis has traditionally been associated with oncology, recent advancements in angiogenesis research have also influenced the treatment of non-malignant conditions in fields such as ophthalmology, cardiology, and gynecology2. The historical development of angiogenesis research gained interest in the 1970s, primarily due to the pioneering work of Judah Folkman. The study stated that tumors could be inhibited by targeting their blood supply, leading to the hypothesis that angiogenesis was a crucial factor in tumor growth. His early experiments laid the groundwork for the development of various angiogenesis assays that were essential for understanding the mechanisms of blood vessel formation in both health and disease3. Understanding the mechanisms that control angiogenesis and its regulation is crucial for developing successful therapeutic interventions and evaluating potential drug candidates.
Angiogenesis assays can be used to assess the pro- or anti-angiogenic effects of endogenous or exogenous stimuli by measuring their effects in in vitro, in vivo, and ex vivo methods using samples from either animals or humans4. Generally, in vitro techniques focus on different phases of the angiogenesis process and are utilized for initial evaluations, while in vivo techniques more closely replicate natural conditions to provide more relevant data4. Ex vivo models of angiogenesis, including vascular explant cultures, are becoming more prominent because they overcome limitations encountered by in vitro techniques and simplify the complexity found in in vivo models5. Recent advancements in human model systems, including organ-on-a-chip technologies and 3D bioprinting, have significantly enhanced the study of angiogenesis. These models allow for a more accurate representation of human physiology, addressing some limitations of conventional animal models. For instance, human endothelial cells can be cultured in 3D matrices that mimic the extracellular environment, thereby facilitating a better understanding of angiogenesis mechanisms in human tissues6.
Therefore, this review article focuses on the use of human samples that are currently most often employed to study angiogenesis through in vitro and ex vivo methods. The information gathered aims to provide deeper insights into the use of humanized models in improving the translational potential of angiogenesis research, allowing researchers to study the effects of angiogenic factors in a context that closely resembles human biology. The shift toward human-centric models has been pivotal in identifying novel therapeutic targets and enhancing the efficacy of antiangiogenic therapies.
Angiogenesis Assay
Angiogenesis assays are experimental techniques designed to evaluate various aspects of blood vessel formation and serve as essential tools in angiogenesis research4. These assays provide critical insights into the complex mechanisms underlying angiogenesis, enabling researchers to investigate the effects of different chemicals, growth factors, and genetic alterations on blood vessel development4. Below is an overview of in vitro and ex vivo methodologies employed in previous studies related to angiogenic diseases.
In Vitro Angiogenesis Assay
In vitro models involve cultivating isolated tissue components of an organ while maintaining certain features of the in vivo environment. The primary goal of in vitro models in research and medicine is to reduce experimental variables by isolating various organ components or structures for study in regulated, reproducible, and easily evaluated circumstances7. In vitro models of angiogenesis mainly focus on endothelial cell proliferation, migration, and tube formation in response to angiogenic stimuli. Table 1 shows the comparison of the method and provides a summary for better understanding.
| Type of in vitro assays | Methods | References |
|---|---|---|
| Endothelial cell proliferation assay | The effects of pro-angiogenic and anti-angiogenic substances on proliferation can be evaluated using direct cell counts, DNA synthesis, or metabolic activities. Cell proliferation is commonly assessed by a colorimetric technique. MTT : - Seed the cells in 96-well plates for 24 hours and treat with test compound. - Change the medium for the next day and add 10 µL of MTT reagent. Incubate the plates for 3-5 hours at 37 o C. - Remove media and add 100 µl of DMSO. Incubate for 15 minutes and then read absorbance at 570 nm. - Mitochondrial enzymes convert MTT into the formazan dye in correlation with the number of cells. MTT is a yellow tetrazole compound that is transformed into purple formazan in living cells, and its colour absorbance may be measured using a spectrophotometer. Other than MTT, BrdU also can be utilized for DNA cell labelling, followed by cell analysis employing colorimetry, chemiluminescence, or fluorescence detection | 8 , 9 |
| Endothelial cell migration assay | Cell migration is the movement of cells in response to external biochemical cues. One way to detect the migration process is the scratch wound assay. - Seed the cell in the well plate and incubate until confluency reached 90%. - Scrap the cells by using 200 µl pipettes tip or cell scrapper. Wash the cell-plate with PBS to remove the floating cells. - Add the media with treatment and observe the wound area using inverted microscope. This approach is used to measure fundamental cell migration properties in terms of speed, persistence, and polarity. | 8 , 10 |
| Tube formation assay | Commonly used in vitro to assess angiogenic characteristics by observing the creation of tubular structures from endothelial cells A common method for studying tube formation is to culture HUVECs on Matrigel and observe the branching structures within 12 to 24 hours. | 11 |
| Spheroid-based assay | Enable to investigate the effects of drug or genetic manipulations on sprouting angiogenesis in a fast and robust manner. Cells will be harvested and seed cells in ultra-low-attachment plate to promote spheroid formation as shown in Figure 1 . After checking the assay uniformity and reproducibility, downstream application could be proceeded. This assay better reflects in vivo angiogenesis than other well-known in vitro angiogenesis assays, such as the 2D tube formation on Matrigel, due to the formation of complex cell-cell interactions and gradients that are crucial for studying angiogenesis. | 12 , 13 , 14 |
| Organ-On-A-Chip Models | The organ on a chip (OOAC) is a cutting-edge in vitro microscale biomimetic platform capable of recreating the physiological environments of human organs. OOAC is a novel in-vitro micro-scale biomimetic platform that helps in reproducing physiological environment of human organs. This technology involves cell biology, engineering and material sciences to simulate in-vivo tissues. The initial stage of this process involves designing and creating the microfluidic chip of organ on a chip models ( Figure 2 ) to mimic the cellular structure and surroundings of the desired organ or tissue. The chip used for researching angiogenesis may have endothelial cell-lined channels that imitate blood arteries, along with other cell types such pericytes, smooth muscle cells, and extracellular matrix components. There are several micro-fabrication methods that had been introduced such as photolithography, soft lithography, 3D printing and computer numerical code micro milling. Type of microarchitectures that can be used in micro engineered chips such as single layer microfluids device, 3D compartmentalization, microfluidic vascular networks. | 6 , 15 |
Ex Vivo Angiogenesis Assay
Ex vivo refers to experiments performed on tissue or organs extracted from a living organism and conducted outside the original biological context16. In scientific research, ex vivo methodologies allow for experimentation in a controlled laboratory environment while maintaining conditions that closely mimic those found within organisms. Tissues may be removed in various ways, including whole organs or parts of tissue16. Unlike in vitro, which typically involves isolated cells or tissues cultured in controlled environments, ex vivo studies utilize living cells or tissues taken directly from an organism. This distinction allows ex vivo experiments to retain more of the natural architecture and metabolic processes of the tissue, making them more representative of in vivo conditions17. Ex vivo models have become increasingly important in various fields, including disease modeling, drug discovery, and regenerative medicine, as they bridge the gap between simpler in vitro assays and more complex in vivo studies. Table 2 shows the list of ex vivo angiogenesis assays that have been conducted in previous studies.
| Types of ex vivo angiogenesis assay | Methods | References |
| Aortic ring assay | This assay facilitates the growth of angiogenic vessels originating from a section of the aorta when cultured within a three-dimensional matrix, such as collagen or fibrin gels. Figure 3 shown the overview of the aortic ring assay method. | 5 |
| Tissue explant assay | A technique involving the isolation and ex vivo cultivation of tissue fragments while maintaining their native cellular architecture and interactions. Upon isolation, the explants are embedded in extracellular matrix gels to maintain their three-dimensional structure and support the angiogenic processes. | 18 |
Human models in angiogenesis assays
In vitro
In vitro angiogenesis models are essential tools for studying the intricate processes of blood vessel creation in a controlled laboratory environment19. By using human endothelial cells and other relevant supporting cell types, these models enable researchers to investigate the spatial and temporal aspects of angiogenesis, understand the signaling pathways in vascular development, and test substances that could promote or inhibit angiogenesis20. Endothelial cells, once considered merely a basic blood vessel lining, are now acknowledged as a highly dynamic tissue that significantly contributes to various physiological and pathological processes21. Below are several types of human endothelial cell samples that have been utilized in angiogenesis research.
Human Umbilical Vein Endothelial Cells (HUVECs)
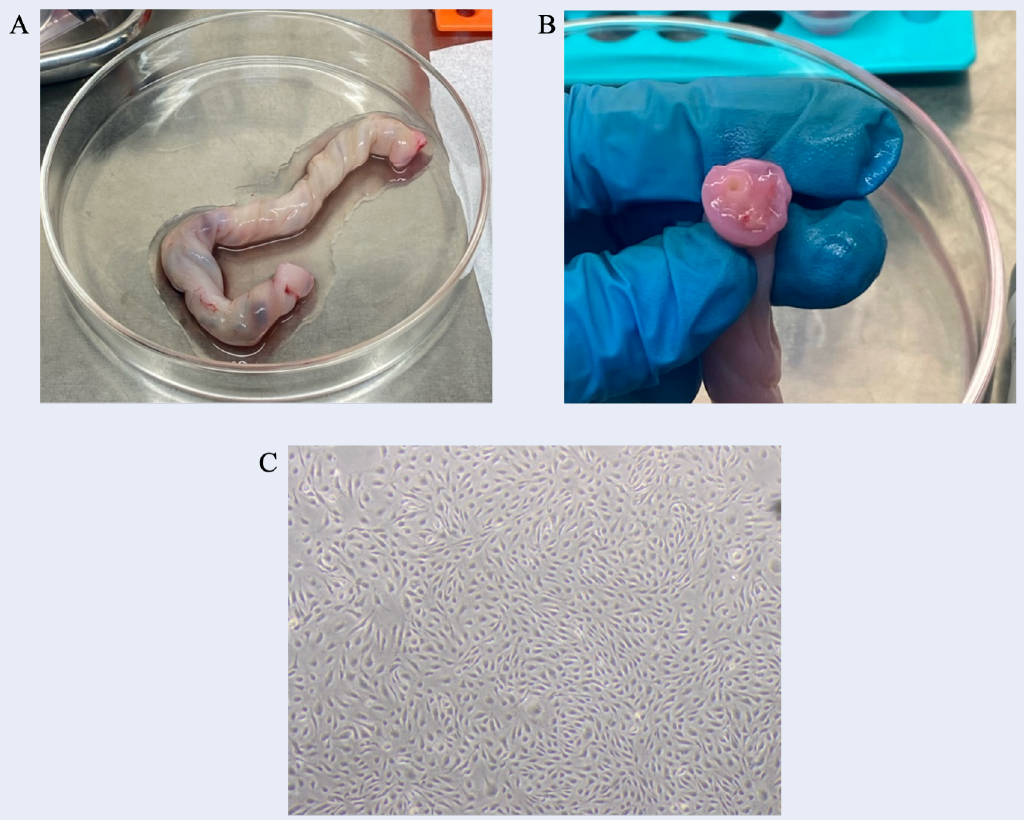
HUVECs serve as a valuable model for researching vascular endothelium features and key biological pathways related to endothelial function22. They are frequently utilized in in vitro research because they are easily isolated from the human umbilical cord, readily available, and their behavior is well-documented 22. Figure 4 shows an example of the morphology of HUVECs and the umbilical cord that was dissected to isolate HUVECs. In addition, HUVECs have the capacity to accurately represent the human vascular endothelium. This is consistent with the results of Lau et al.23, who evaluated HUVECs and human umbilical artery endothelial cells (HUAEC) as in vitro models for cardiovascular research. Their study showed that both cell types displayed comparable features in terms of cell viability, metabolic activity, and membrane integrity, indicating that both cell types are equally appropriate for cardiovascular research. HUVECs are commonly used to investigate angiogenesis in vitro and its associated disorders24. Many studies have utilized HUVECs to explore the molecular processes related to blood vessel formation, such as endothelial cell migration, growth, and branching25.
Moreover, HUVECs are a useful model for researching vascular illnesses such as atherosclerosis, thrombosis, and endothelial dysfunction26. In earlier studies, they were utilized to replicate disease conditions in a laboratory setting to explore the fundamental mechanisms involved in vascular pathology. The HUVEC model is valuable for studying how hemodynamic forces affect the endothelium and the development of atherosclerotic plaques. This model enables researchers to subject endothelial cells to shear stress under controlled flow conditions, replicating blood flow conditions in living organisms22. The HUVEC model has proven valuable for investigating various biological processes and disorders, including inflammation, apoptosis, preeclampsia, cardiovascular diseases, and regenerative medicine22, 27.
Nevertheless, one of the primary limitations of HUVECs is their unsuitability for long-term investigations22. HUVECs typically have a lifespan of around 10 passages, although some researchers suggest that these cells may lose their original features and responsiveness to stimuli after passage 622. HUVECs may not be suitable for vascularizing specific tissues, such as neurological tissue, which requires a tightly sealed endothelium and an effective blood-brain barrier28, 29. Furthermore, as the human umbilical cord is fetal rather than maternal tissue, the fetal gender must be considered, as it might yield different results in metabolite levels and oxidative stress29. While HUVECs are commonly used in vascular biology research due to their ease of isolation and culture, they may not fully represent the phenotypic response of adult-derived endothelial cells30. This is because HUVECs are fetal cells and may not accurately reflect the characteristics and behavior of endothelial cells found in adult tissues. These limitations highlight the need to consider the specific requirements of each application when choosing endothelial cell types for research.
Human Aortic Endothelial Cells (HAECs)
HAECs are commonly derived from the inner lining of the aorta, a major artery responsible for transporting oxygen-rich blood from the heart to the body. These cells can be sourced from various segments of the aorta, such as the ascending aorta (proximal to the heart) or the descending aorta (distal from the heart)31. The specific site of HAEC isolation may vary based on the research methodology or experimental design. HAECs are typically procured from explants of healthy human heart donors through surgical procedures or post-mortem tissue donations32. Samples containing the aortic endothelial layer are harvested, and endothelial cells are extracted and cultured in laboratory settings for further analysis and experimentation32. The collection and utilization of human tissue samples for research purposes are governed by ethical guidelines and regulatory approvals33.
HAECs offer an excellent model system for investigating various aspects of cardiovascular function and disease, such as atherosclerosis and endothelial dysfunction caused by different stressors34, 35. HAECs can be employed to evaluate changes in the vascular endothelium and its function at a preclinical stage, which holds potential for refining therapeutic strategies. In addition, HAECs have been found to exhibit robust angiogenic potential in 3D microfluidic angiogenesis systems, which is critical for investigating vessel formation and regeneration36. It was also reported that HAECs exhibit similar cellular characteristics to HUVECs in a 2D culture system37. The study of HAECs in laboratory settings has significantly contributed to our understanding of endothelial physiology and the pathogenesis of vascular diseases.
While in vitro cell cultures provide insight into the interactions of endothelial cells with diverse mediators, it is essential to acknowledge their inherent limitations, particularly regarding the uncertainty of translatability to human physiological contexts. Like other endothelial cell types, HAECs may undergo alterations upon extraction from their native human environments. This is primarily due to the absence of the intricate intercellular communications observed within the living organism, which cannot be fully captured via in vitro assays38. Furthermore, HAECs demonstrate variability according to factors such as donor age, health status, and genetic background, which could influence the consistency and reliability of research outcomes32. In contrast to utilizing immortalized endothelial cell lines or cells from more accessible sources like the human umbilical vein, isolating, culturing, and maintaining primary HAECs necessitate a more complicated and expensive process involving the acquisition of human heart donors through surgical procedures or post-mortem tissue donations32.
Human Coronary Artery Endothelial Cells (HCAECs)
HCAECs are considered a dynamic organ exhibiting secretory, metabolic, and immune functions beyond their main role in modulating nutrient translocation across the vascular wall. HCAECs are specifically involved in the secretion of various vasoactive substances that regulate vascular smooth muscle tone and blood flow within the coronary arteries39. HCAECs originate from the coronary arteries of the human heart40, and they can be obtained from individuals undergoing percutaneous coronary interventions (PCI)41. Notably, most studies employ commercially available HCAECs purchased from authorized companies, such as Promocell (Germany) or Lonza (USA)42, 43. As indicated by these providers, primary HCAECs can be isolated not only from the main coronary arteries but also from their respective branches, including the right and left coronary artery, anterior descending, and circumflex branches, from a single donor. As these cells originate from human coronary arteries, they play a pivotal role in supplying oxygenated blood to the heart muscle and therefore are ideally suited for investigating the pathogenesis of coronary heart disease and developing innovative therapies39. Moreover, according to Lakota et al.43, HCAECs exhibit unique sensitivities and responses compared to endothelial cells derived from other vascular beds, as HCAECs were shown to have sensitivity to tumor necrosis factor alpha (TNFα)-induced expression of adhesion molecules compared to HUVECs and human dermal microvascular endothelial cells (HMVECs).
However, the considerable heterogeneity and organ-specific characteristics of HCAECs pose challenges in result interpretation and study reproducibility. This means that HCAECs might not be fully representative of the behavior of endothelial cells from other vascular beds, potentially resulting in inconclusive or inaccurate findings44. A study by Wagner et al.45 also emphasized that HCAECs were the only cells expressing spike protein post-SARS-CoV-2 infection, indicating distinct responses compared to other endothelial cells, such as HUVECs, HMECs, and human pulmonary arterial cells. This suggests that observations in HCAECs may not fully capture the responses of endothelial cells from diverse vascular beds or under varying pathological conditions. Besides that, the variability among donors can also affect the behavior and reactivity of HCAECs in vitro. Donor-related factors, such as age, sex, genetic background, and health status, may influence angiogenic responses, contributing to variability in experimental results46, 47. Obtaining HCAEC samples can be intricate, involving procurement from patient donors or acquisition from authorized companies with legal consent, potentially incurring higher costs41, 43.
Ex vivo
Isolating human endothelial cells from the primary organ and culturing the cells in vitro might cause the loss of complexity of the organ structure48. Thus, ex vivo angiogenesis assays play a key role in exploring the complex interaction between molecular and cellular elements in angiogenic processes under controlled experimental settings49. Among the various ex vivo assays available, human sample models hold particular importance due to their direct relevance to human physiology and disease. By utilizing human tissues and cells, these models provide a more accurate representation of the physiological conditions and responses to human angiogenesis50. Below are several types of human samples that have been utilized in ex vivo angiogenesis research.
Human Saphenous Vein (HSV)
HSV have been previously utilized in ex vivo assays. These veins are located beneath the skin and contain valves that prevent blood backflow, playing a crucial role in transporting deoxygenated blood from the leg to the heart51. Interestingly, HSVs are widely employed as a conduit for coronary artery bypass grafting52. According to the literature, HSVs have been extensively utilized in ex vivo tissue culture investigations, particularly for modeling intimal hyperplasia and exploring the causes of vein graft failure in coronary artery bypass grafting (CABG)53. In the context of angiogenesis research, as indicated in Table 3, most researchers have cultured saphenous veins by embedding them in a gel to observe sprouting formation. Conversely, there is limited specific mention of ex vivo tissue cultures in previous angiogenesis studies that used other veins, including the human umbilical vein.
| Related Angiogenesis Study | Methods | References |
| Su-PAR trigger endothelial cell signaling leading to new vessel formation through its chemotactic Ser 88 -Arg-Ser-Arg-Tyr 92 sequence | - 48-well plates were covered with 200 µl of Matrigel. - 2-3 mm of the long cross section was placed on the gel after the gel has polymerized and another 200 µl of Matrigel was added to cover the tissue. - The ring was cultured with 1 ml of complete media growth (EBM) | 54 |
| Effect of thalidomide in antiangiogenic activity | - The vein was cut into 2 mm long cross sections. - A 12-well plate was covered with 250 µl of Matrigel and then the tissue was placed onto the polymerized gel. Another 250 µl of Matrigel was used to cover the tissue. - The tissue was cultured in 2 ml (endothelial cell growth media) EGM-2 medium for 24 hours before treatment. - The media was removed after 24 hr and replaced with 1 ml endothelial basal media (EBM) with 2% FBS and 10 ug/mL gentamicin. - Photographed on day 5. | 55 |
| Diminished venous endothelial Eph-B4 expression is associated with an angiogenic and mitogenic phenotype | - A segment of adult human saphenous vein was used in the flow model. - Veins were inspected for feasibility of incorporation into the bioreactor, and structural parameters were measured. | 56 |
| Function of PDE10A in SMC proliferation and intimal hyperplasia | - The vein was cut into 0.5 cm lengths. - Cultured with luminal surface in a 12-well plate with RPMI 1640 medium containing 15% of FBS. | 52 |
| Vinpocetine suppress pathological vascular remodeling | - The vein was cut into 0.5 cm sections. - The segments were pinned onto a Mersilene mesh with luminal surface in 12-well plates in RPMI 1640 medium with 30% FBS and other supplements including antibiotics. The tissue was cultured for 7 days | 57 |
Human artery
The human arterial ring assay is an innovative system for the 3D study of angiogenesis. Arterial explants for ex vivo angiogenesis studies can be obtained from various sources, such as aortic tissue, choroid, epididymis, and skeletal muscle. Aortic explants are able to form branching microvessels when embedded in an extracellular matrix58. Table 4 shows a list of previous reports that utilized human artery explants in ex vivo angiogenesis studies.
| Artery explants | Angiogenesis-related study | Methods | References |
| Umbilical cord | Human tumor angiogenesis | - Human arterial rings assay. - Arterial rings were placed on 48-well cell culture dishes pre-coated with 100 µl of basement membrane extract (BME) and overlaid with 100 µl of BME. - Maximum growth velocity achieved at 14 days. | 59 |
| Umbilical cord | Kisspeptin-10 roles inhibiting angiogenesis in human blood vessels | - Vessels were cut into 1 mm sections. - The vessel ring was embedded in Matrigel (200 µl) and were cultured for 2-3 days with media consisting of 10% FBS. | 60 |
| Temporal artery biopsy | Giant cell arteritis | - Cultured in Matrigel for 5 days in 96 well plate. | 61 |
| Human umbilical cord | Identification of new genes regulating sprouting, screening pro and anti-angiogenic drugs, biomarkers and analysis of tumor microenvironmental effects on vessel formation | - Artery was cut into 30 1-2 mm sections and placed inside a 48-well plate that was precoated with 100 µl of BME gel. - Cultured for 18 days with media consisting of 5% FBS. | 62 |
| Human Mesenteric arteries | Age-associated deterioration in angiogenesis, blood flow and glucose homeostasis by therapeutically targeting CD47 | - Arterial ring assay by cutting the vessel into 1 mm sections. - Embedded with Matrigel with cell media. - Incubated the tissue for 15 days. | 63 |
Human Retinal Explant
Excess angiogenesis also contributes to the pathogenesis of various ocular illnesses, including diabetic retinopathy, age-related macular degeneration (AMD), and retinopathy of prematurity64. Table 5 shows the usage of human retinal tissues used to investigate retina-related angiogenesis illnesses. Based on our literature search, there are only a small number of previous reports that used human retinal explants in angiogenesis studies. This might be due to the difficulty in obtaining donor eyes and the high level of competence required for retina manipulation, which may not be feasible with small samples65.
| Retina explant | Methods | References |
| Choroidal tissues | - Human choroidal explants were cultured in normal medium for 5 days for neovessel growth and undergo treatment. | 64 |
| Human iris | - Whole iris fragments were cut into 3 mm diameter segments and embedded with Matrigel in a 24-well plate. - The tissue explants were cultured with ECGM for 48 hours. | 66 |
| Choroidal explant | - Choroidal sprouting assay was conducted by embedding the samples with Matrigel in 24 well plate. - The samples were incubated for 1 day and continued with treatment. - The sprout image was captured at day 5. | 67 |
| Human retinal explants | - Each of the tissue explant was cut in to 4 mm diameter segments. - Then, the tissues were placed on top of a gel matrix. - The tissues were observed from day 2 to day 15. | 68 |
Clinical Research in Angiogenic Therapies
Clinical trials and research have led to the development of various effective anti-angiogenic treatments, such as bevacizumab, tyrosine kinase inhibitors like sorafenib, and human recombinant endostatin. These advancements indicate the potential of targeting angiogenesis for therapeutic purposes, particularly in the context of cancer diseases69. In addition, numerous clinical trials have assessed the safety and efficacy of VEGF therapy for ischemic coronary and peripheral arterial disease (Table 6), which showed potential therapeutic benefits despite the low significance. The findings from human models in angiogenesis assays have significant implications for clinical practice, particularly in the development of therapeutic strategies for various diseases. By utilizing human-derived models, researchers can gain insights that are more directly applicable to patient care.
Angiogenesis assays have become significant tools in the discovery of anti-angiogenic drugs for cancer treatment. Identification of vascular endothelial growth factor (VEGF) as an important regulator of angiogenesis led to the development of bevacizumab (Avastin), which is a monoclonal antibody that suppresses VEGF70. Preclinical studies of angiogenesis with human endothelial cells revealed that bevacizumab was capable of inhibiting tumor angiogenesis, thereby supporting its clinical use. Clinical trials have shown that bevacizumab, when used together with chemotherapy, enhances outcomes for several malignancies, including osteosarcoma70. The successful translation of angiogenesis testing results into the clinic underlines the value of these models in developing effective therapies for cancer patients. Aside from cancer treatment, angiogenic therapies have also been used in clinical trials for retinal and ischemic diseases. Table 6 shows previous studies that conducted clinical trials associated with angiogenic agent targets.
| Angiogenic therapy target | Study design (Disease; Time; Drugs; Dose; Number of patients; Phase) | Outcomes | References |
| VEGFR inhibitor | Advanced renal cell cancer; Axitinib + pembrolizumab; 5mg + 2 mg/kg; 6 weeks; n = 52; Phase 1b | The treatment combination of axitinib + pembrolizumab is tolerable and shows promising antitumour activity in patients with treatment-naive advanced renal cell carcinoma No unexpected toxicities were observed 94% of patients experienced some degree of tumour shrinkage. | 71 |
| VEGF | Osteosarcoma; 29 weeks; Bevacizumab + MAP; 15 mg/kg; n = 3; Phase II | 4-year EFS rate: 57.5% ± 10.0% Overall survival rate: 83.4% ± 7.8% 28%evaluable patients had good histologic response (<5% viable tumor) to preoperative chemotherapy. | 70 |
| VEGF inhibitor | Branch retinal vein occlusion; 12 months; dexamethasone & ranibizumab; 0.7 mg (dexamethasone) & 0.5 mg (ranibizumab); n = 307 | Dexamethasone and ranibizumab improved best-corrected visual acuity and anatomical outcomes. Dexamethasone did not show non-interiority to ranibizumab Dexamethasone associated with increased risk of intraocular pressure elevation and cataract pressure | 72 |
| VEGF | Angina; 0,3 and 12 months; AdVEGF-DΔNΔC (AdVEGF-D) or placebo (control) groups; 200 µL at 10 sites; n = 30 | Shown significant increase in myocardial perfusion at 3 months and 12 months compared to baseline. | 73 |
| VEGFR inhibitor | Hepatocellular carcinoma; 4 weeks; oral dovitinib; 500 mg (5 days on & 2 days off); n = 24; phase II | Overall response rate was 48%, including 13% complete remission Time to progression: 16.8 months Overall survival: 34.8 months | 74 |
| BMSC | Critical limb ischemia; over 12 months; stempeucel®; 2 million cells/kg body weigh; n = 24; Phase III | Showed statistically significant reduction in rest pain and ulcer size (healing of ulcer) as compared to baseline. Increased the blood flow to the ischemic limbs as ABPI and ASP increased. | 75 |
Limitations of Using Human Models in Angiogenesis Assays
Angiogenesis denotes the intricate process of forming new blood vessels, a pivotal aspect of human physiological functions. Utilizing human models in studying angiogenesis yields significant outcomes for diseases associated with this process. Nonetheless, the study of angiogenesis through human models is not devoid of limitations due to various factors. Firstly, ethical constraints emerge as a prominent issue. The ethical framework governing research involving human subjects underscores fundamental principles, including respect for individuals and associated responsibilities mandated by justice, whereas regulations concerning research involving animal subjects primarily focus on limited considerations of welfare76. Other than that, human samples can show inherent individual variability in terms of genetic differences, health conditions, and age-related factors. These factors might add complexity and variability to the study outcomes65. Obtaining human tissue samples for angiogenesis assays can also pose challenges, particularly when considering specific tissues or disease conditions, resulting in limitations in sample size and study replication65. Working with human samples also involves high costs due to various factors, including sample collection, processing, and storage77. Due to the limited availability of human samples from donors, most researchers are forced to purchase samples from a small number of established companies, such as Promocell (Germany) or Lonza (USA)42. All these limitations and issues must be carefully considered by researchers before embarking on their angiogenesis-related research.
Future Direction of Using Human Models in Angiogenesis Assay
Currently, the development of human model technologies in the angiogenesis research field has shown potential for enhancing our understanding and for developing new therapeutics. Models such as organ-on-a-chip systems, 3D bioprinted tissues, and ex vivo culture have the potential to overcome the limitations of conventional in vitro and in vivo assays by offering more accurate and physiologically relevant platforms for studying angiogenesis. As these technologies evolve, they can enhance the precision of drug testing. For example, organ-on-a-chip systems allow for the precise control of the cellular microenvironment6. By incorporating human endothelial cells and other supporting cell types, organ-on-a-chip devices can be used to study angiogenesis in the context of specific organ systems, such as the brain, heart, or kidney6. These models can provide valuable insights into the role of angiogenesis in organ development, homeostasis, and disease pathogenesis. 3D bioprinting technology also allows for the precise deposition of cells, biomaterials, and growth factors to create complex, tissue-like structures. By incorporating human endothelial cells and supporting cell types into 3D bioprinted constructs, researchers can develop highly customizable angiogenesis assays that mimic the native extracellular matrix and cellular microenvironment78. Additionally, CRISPR can be used to create patient-derived induced pluripotent stem cells (iPSCs) with disease-relevant genetic mutations, which can then be differentiated into endothelial cells and used to develop personalized angiogenesis assays24. As these emerging technologies continue to advance, they will likely play an increasingly important role in angiogenesis research. By providing more accurate and physiologically relevant human models, researchers will be better equipped to study the complex mechanisms of angiogenesis, identify novel therapeutic targets, and develop more effective treatments for angiogenesis-related diseases.
Conclusion
It is important to understand the development of the vascular system and the mechanisms that lead to vascular diseases in order to discover new, effective treatments. Combining in vitro and ex vivo models using human samples offers a comprehensive approach to studying angiogenesis. This integrative strategy bridges the gap between simplified in vitro systems and the complex realities of in vivo conditions, enhancing the translational potential of research findings. However, key challenges remain, including ethical considerations, variability in human samples, difficulties in tissue sample acquisition, and the cost of obtaining samples. Addressing these challenges is critical for advancing the field. Therefore, collaboration with ethical boards and regulatory agencies to establish clear, standardized guidelines for the use of human tissues in angiogenesis research can help streamline the approval process and ensure that research is conducted in a manner that respects donor rights. By utilizing large-scale biobanks that store a wide variety of human tissue samples, researchers can select samples that best match their study criteria and reduce variability65. In addition, establishing collaborative networks between research institutions, hospitals, and biobanks can improve access to human tissue samples and facilitate the sharing of resources and information. Additionally, funding from government agencies, non-profit organizations, or private-sector partnerships can encourage sharing of expensive resources, such as specialized equipment or reagents, through collaborative agreements or shared facilities. All these measures might help reduce the overall cost burden for individual research groups. By addressing these limitations through strategic collaboration, future researchers can enhance the effectiveness of human models in angiogenesis assays, ultimately leading to more accurate and clinically relevant findings.
Abbreviations
ABPI: Ankle-brachial pressure index; AKT: Ak strain transforming (Protein kinase B); ASP: Ankle systolic pressure; ATP: Adenosine triphosphate; BMSC: Bone marrow-derived stem cell; BrdU: Bromodeoxyuridine; CABG: Coronary artery bypass grafting; CAD: Coronary artery disease; ECM: Extracellular matrix; EFS: Event free survival; ETT: Exercise treadmill tests; FGFs: Fibroblast growth factors; HAECs: Human aortic endothelial cells; HCAECs: Human Coronary Artery Endothelial Cells; HMVEC: Human Microvascular Endothelial cells; HSV: Human saphenous veins; HUVECs: Human umbilical cord vein endothelial cells; MMPs: Matrix metalloproteinases; MTT: 3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide; NCD: Non-communicable diseases; OOAC: The organ-on-a-chip; PDGF: Platelet-derived growth factor; PFS: Progression-free survival; PI3K: Phosphoinositide 3-kinases; TGFβ: Transforming growth factor beta; VEGF: Vascular Endothelial Growth Factor
Acknowledgments
We would like to appreciation to the financial support provided by the Ministry of Higher Education (MOHE), Malaysia through the Fundamental Research Grand Scheme (FRGS), under grant number FRGS/1/2023/SKK06/UKM/02/16.
Author’s contributions
Maisarah was the primary author and was responsible for drafting and editing the manuscript. Nur Najmi, Azizah, and Nadiah provided supervision, critical review, and contributed to manuscript revisions. Mohd Faizal, Safa, and Ishamuddin participated in the review process and provided feedback on the manuscript. All authors read and approved the final version of the manuscript.
Funding
Fundamental Research Grand Scheme (FRGS), under grant number FRGS/1/2023/SKK06/UKM/02/16.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Elebiyo
T.C.,
Rotimi
D.,
Evbuomwan
I.O.,
Maimako
R.F.,
Iyobhebhe
M.,
Ojo
O.A.,
Reassessing vascular endothelial growth factor (VEGF) in anti-angiogenic cancer therapy. Cancer treatment and research communications.
2022;
32
:
100620
.
View Article Google Scholar -
Griffioen
A.W.,
Dudley
A.C.,
The rising impact of angiogenesis research. Angiogenesis.
2022;
25
(4)
:
435-7
.
View Article PubMed Google Scholar -
Ribatti
D.,
Judah Folkman, a pioneer in the study of angiogenesis. Angiogenesis.
2008;
11
(1)
:
3-10
.
View Article Google Scholar -
Stryker
Z.I.,
Rajabi
M.,
Davis
P.J.,
Mousa
S.A.,
Evaluation of Angiogenesis Assays. Biomedicines.
2019;
7
(2)
:
37
.
View Article PubMed Google Scholar -
Kapoor
A.,
Chen
C.G.,
Iozzo
R. V.,
A simplified aortic ring assay: a useful ex vivo method to assess biochemical and functional parameters of angiogenesis. Matrix biology plus.
2020;
6
:
100025
.
View Article Google Scholar -
Singh
D.,
Mathur
A.,
Arora
S.,
Roy
S.,
Mahindroo
N.,
Journey of organ on a chip technology and its role in future healthcare scenario. Applied Surface Science Advances.
2022;
9
:
100246
.
View Article Google Scholar -
Collins
S.D.,
Yuen
G.,
Tu
T.,
Budzinska
M.A.,
Spring
K.,
Bryant
K.,
In vitro models of the liver: disease modeling, drug discovery and clinical applications. Exon Publications.
2019;
9
:
47-67
.
View Article Google Scholar -
Roper
S.J.,
Coyle
B.,
Establishing an in vitro 3d spheroid model to study medulloblastoma drug response and tumor dissemination. Current Protocols.
2022;
2
(1)
:
e357
.
View Article PubMed Google Scholar -
Kannan
P.,
Schain
M.,
Lane
D.P.,
An automated quantification tool for angiogenic sprouting from endothelial spheroids. Frontiers in Pharmacology.
2022;
13
:
883083
.
View Article PubMed Google Scholar -
Merck. Tumor spheroid formation assay [Internet]. 2024 [cited 2024 Aug 15]. Available from: https://www.sigmaaldrich.com/MY/en/technical-documents/protocol/cell-culture-and-cell-culture-analysis/3d-cell-culture/tumor-spheroid-formation-assay. 2024
.
-
Hisam
N.S. Nor,
Ugusman
A.,
Rajab
N.F.,
Gregoli
K. Di,
Ahmad
M.F.,
Anuar
N.N. Mohamad,
In vitro cell migration, invasion, and adhesion assays: from cell imaging to data analysis. Frontiers in cell and developmental biology.
2023;
14
:
107
.
View Article Google Scholar -
Evyapan
G.,
Senturk
N.C.,
Celik
I.S.,
Ornidazole Inhibits the Angiogenesis and Migration Abilities of Non-small Cell Lung Cancer (NSCLC) via Downregulation of VEGFA/VEGFR2/NRP-1 and PI3K/AKT/mTOR Pathways. Cell biochemistry and biophysics.
2024;
82
(4)
:
3277-85
.
View Article Google Scholar -
Pijuan
J.,
Barceló
C.,
Moreno
D.F.,
Maiques
O.,
Sisó
P.,
Marti
R.M.,
In vitro cell migration, invasion, and adhesion assays: from cell imaging to data analysis. Frontiers in Cell and Developmental Biology.
2019;
7
:
107
.
View Article PubMed Google Scholar -
Martí-Clúa
J.,
Methods for inferring cell cycle parameters using thymidine analogues. Biology (Basel).
2023;
12
(6)
:
885-5
.
View Article PubMed Google Scholar -
Joseph
X.,
Akhil
V.,
Arathi
A.,
Mohanan
P.V.,
Comprehensive development in organ-on-a-chip technology. Journal of Pharmaceutical Sciences.
2022;
111
(1)
:
18-31
.
View Article PubMed Google Scholar -
Hughes
D.L.,
Hughes
A.,
Soonawalla
Z.,
Mukherjee
S.,
O'neill
E.,
Dynamic physiological culture of ex vivo human tissue: a systematic review. Cancers.
2021;
13
(12)
:
2870
.
View Article Google Scholar -
Hemmilä
S.,
Ruponen
M.,
Toropainen
E.,
Tengvall-Unadike
U.,
Urtti
A.,
Kallio
P.,
Microflow-based device for in vitro and ex vivo drug permeability studies. SLAS Technology.
2020;
25
(5)
:
455-62
.
View Article PubMed Google Scholar -
Carranza-Rosales
P.,
Valencia-Mercado
D.,
Esquivel-Hernández
O.,
González-Geroniz
M.I.,
Bañuelos-García
J.I.,
Castruita-Ávila
A.L.,
Breast cancer tissue explants: an approach to develop personalized therapy in public health services. Journal of Personalized Medicine.
2023;
13
(10)
:
1521
.
View Article PubMed Google Scholar -
Kim
S.J.,
Kim
M.G.,
Kim
J.,
Jeon
J.S.,
Park
J.,
Yi
H.G.,
Bioprinting methods for fabricating in vitro tubular blood vessel models. Cyborg and Bionic Systems (Washington, D.C.).
2023;
4
:
0043
.
View Article PubMed Google Scholar -
Maurya
M.R.,
Gupta
S.,
Li
J.Y.,
Ajami
N.E.,
Chen
Z.B.,
Shyy
J.Y.,
Longitudinal shear stress response in human endothelial cells to atheroprone and atheroprotective conditions. Proceedings of the National Academy of Sciences of the United States of America.
2021;
118
(4)
:
e2023236118
.
View Article PubMed Google Scholar -
Zhou
H.L.,
Jiang
X.Z.,
Ventikos
Y.,
Role of blood flow in endothelial functionality: a review. Frontiers in Cell and Developmental Biology.
2023;
11
:
1259280
.
View Article PubMed Google Scholar -
Medina-Leyte
D.J.,
Domínguez-Pérez
M.,
Mercado
I.,
Villarreal-Molina
M.T.,
Jacobo-Albavera
L.,
Use of human umbilical vein endothelial cells (huvec) as a model to study cardiovascular disease: a review. Applied Sciences (Basel, Switzerland).
2020;
10
(3)
:
938
.
View Article Google Scholar -
Lau
S.,
Gossen
M.,
Lendlein
A.,
Jung
F.,
Venous and arterial endothelial cells from human umbilical cords: potential cell sources for cardiovascular research. International Journal of Molecular Sciences.
2021;
22
(2)
:
978
.
View Article PubMed Google Scholar -
Rahman
H.S.,
Tan
B.L.,
Othman
H.H.,
Chartrand
M.S.,
Pathak
Y.,
Mohan
S.,
An Overview of in vitro, in vivo, and computational techniques for cancer-associated angiogenesis studies. BioMed Research International.
2020;
2020
(1)
:
2020:8857428
.
View Article PubMed Google Scholar -
Gentile
M.T.,
Pastorino
O.,
Bifulco
M.,
Colucci-D'Amato
L.,
HUVEC tube-formation assay to evaluate the impact of natural products on angiogenesis. Journal of Visualized Experiments.
2019;
2019
(148)
:
58591
.
View Article PubMed Google Scholar -
He
S.,
Wu
C.,
Xiao
J.,
Li
D.,
Sun
Z.,
Li
M.,
Endothelial extracellular vesicles modulate the macrophage phenotype: potential implications in atherosclerosis. Scandinavian Journal of Immunology.
2018;
87
(4)
:
e12648
.
View Article PubMed Google Scholar -
Lu
F.,
Gong
H.,
Lei
H.,
Li
J.,
Downregulation of cathepsin C alleviates endothelial cell dysfunction by suppressing p38 MAPK/NF-κB pathway in preeclampsia. Bioengineered.
2022;
13
(2)
:
3019-28
.
View Article PubMed Google Scholar -
Kocherova
I.,
Bryja
A.,
Mozdziak
P.,
Angelova Volponi
A.,
Dyszkiewicz-Konwińska
M.,
Piotrowska-Kempisty
H.,
Human umbilical vein endothelial cells (HUVECs) co-culture with osteogenic cells: from molecular communication to engineering prevascularised bone grafts. Journal of Clinical Medicine.
2019;
8
(10)
:
1602
.
View Article PubMed Google Scholar -
Campesi
I.,
Franconi
F.,
Montella
A.,
Dessole
S.,
Capobianco
G.,
Human umbilical cord: information mine in sex-specific medicine. Life (Basel, Switzerland).
2021;
11
(1)
:
52
.
View Article PubMed Google Scholar -
Moccia
C.,
Cherubini
M.,
Fortea
M.,
Akinbote
A.,
Padmanaban
P.,
Beltran-Sastre
V.,
Mammary microvessels are sensitive to menstrual cycle sex hormones. Advanced Science.
2023;
10
(35)
:
e2302561
.
View Article PubMed Google Scholar -
Donnini
D.,
Perrella
G.,
Stel
G.,
Ambesi-Impiombato
F.S.,
Curcio
F.,
A new model of human aortic endothelial cells in vitro. Biochimie.
2000;
82
(12)
:
1107-14
.
View Article PubMed Google Scholar -
Adelus
M.L.,
Ding
J.,
Tran
B.T.,
Conklin
A.C.,
Golebiewski
A.K.,
Stolze
L.K.,
Single-cell: omic profiles of human aortic endothelial cells in vitro and human atherosclerotic lesions ex vivo reveal heterogeneity of endothelial subtype and response to activating perturbations. eLife.
2024;
12
.
View Article PubMed Google Scholar -
Grizzle
W.E.,
Issues in the use of human tissues to support precision medicine. Journal of Health Care for the Poor and Underserved.
2019;
30
:
66-78
.
View Article PubMed Google Scholar -
Lippi
M.,
Stadiotti
I.,
Pompilio
G.,
Sommariva
E.,
Human cell modeling for cardiovascular diseases. International Journal of Molecular Sciences.
2020;
21
(17)
:
6388
.
View Article PubMed Google Scholar -
Lee
S.H.,
Jeong
Y.J.,
Park
J.,
Kim
H.Y.,
Son
Y.,
Kim
K.S.,
Low-dose radiation affects cardiovascular disease risk in human aortic endothelial cells by altering gene expression under normal and diabetic conditions. International Journal of Molecular Sciences.
2022;
23
(15)
:
8577
.
View Article PubMed Google Scholar -
Seo
H.R.,
Jeong
H.E.,
Joo
H.J.,
Choi
S.C.,
Park
C.Y.,
Kim
J.H.,
Intrinsic FGF2 and FGF5 promotes angiogenesis of human aortic endothelial cells in 3D microfluidic angiogenesis system. Scientific reports.
2016;
6
(1)
:
28832
.
View Article Google Scholar -
Poursaleh
A.,
Beigee
F.S.,
Esfandiari
G.,
Najafi
M.,
Adhesion of monocytes and endothelial cells isolated from the human aorta suppresses by miRNA-PEI particles. BMC Cardiovascular Disorders.
2021;
21
(1)
:
395
.
View Article PubMed Google Scholar -
Ghallab
A.,
In vitro test systems and their limitations. EXCLI Journal.
2013;
12
:
1024-6
.
PubMed Google Scholar -
Krüger-Genge
A.,
Blocki
A.,
Franke
R.P.,
Jung
F.,
Vascular endothelial cell biology: an update. International Journal of Molecular Sciences.
2019;
20
(18)
:
4411
.
View Article PubMed Google Scholar -
Shishkova
D.,
Markova
V.,
Sinitsky
M.,
Tsepokina
A.,
Frolov
A.,
Zagorodnikov
N.,
Co-culture of primary human coronary artery and internal thoracic artery endothelial cells results in mutually beneficial paracrine interactions. International Journal of Molecular Sciences.
2020;
21
(21)
:
8032
.
View Article PubMed Google Scholar -
Yu
S.Y.,
Song
Y.M.,
Li
A.M.,
Yu
X.J.,
Zhao
G.,
Song
M.B.,
Isolation and characterization of human coronary artery-derived endothelial cells in vivo from patients undergoing percutaneous coronary interventions. Journal of vascular research.
2009;
46
(5)
:
487-94
.
View Article Google Scholar -
Pandian
K.,
Huang
L.,
Junaid
A.,
Harms
A.,
Zonneveld
A.J. van,
Hankemeier
T.,
Tracer-based metabolomics for profiling nitric oxide metabolites in a 3D microvessels-on-chip model. FASEB Journal : Official Publication of the Federation of American Societies for Experimental Biology.
2024;
38
(16)
:
e70005
.
View Article PubMed Google Scholar -
Vozzi
F.,
Cecchettini
A.,
Cabiati
M.,
Mg
F.,
Aretini
P.,
Ry
S. Del,
Modulated molecular markers of restenosis and thrombosis byin-vitrovascular cells exposed to bioresorbable scaffolds. Biomedical Materials.
2021;
16
(4)
:
ac0401
.
View Article PubMed Google Scholar -
Lakota
K.,
Mrak-Poljsak
K.,
Rozman
B.,
Sodin-Semrl
S.,
Increased responsiveness of human coronary artery endothelial cells in inflammation and coagulation. Mediators of inflammation.
2009;
2009
(1)
:
146872
.
View Article Google Scholar -
Majewska
A.,
Wilkus
K.,
Brodaczewska
K.,
Kieda
C.,
Endothelial cells as tools to model tissue microenvironment in hypoxia-dependent pathologies. International Journal of Molecular Sciences.
2021;
22
(2)
:
520
.
View Article PubMed Google Scholar -
Wagner
J.U.,
Bojkova
D.,
Shumliakivska
M.,
Luxán
G.,
Nicin
L.,
Aslan
G.S.,
Increased susceptibility of human endothelial cells to infections by SARS-CoV-2 variants. Basic Research in Cardiology.
2021;
116
(1)
:
42
.
View Article PubMed Google Scholar -
Wu
H.,
Yao
Q.,
Lumsden
A.,
Chen
C.,
Characterization of two populations of human coronary artery endothelial cells(1). The Journal of Surgical Research.
2004;
118
(1)
:
38-44
.
View Article PubMed Google Scholar -
Staton
C.A.,
Reed
M.W.,
Brown
N.J.,
A critical analysis of current in vitro and in vivo angiogenesis assays. International Journal of Experimental Pathology.
2009;
90
(3)
:
195-221
.
View Article PubMed Google Scholar -
Smith
L.R.,
Meyer
G.A.,
Skeletal muscle explants: ex-vivo models to study cellular behavior in a complex tissue environment. Connective Tissue Research.
2020;
61
(3-4)
:
248-61
.
View Article PubMed Google Scholar -
Loewa
A.,
Feng
J.J.,
Hedtrich
S.,
Human disease models in drug development. Nature Reviews Bioengineering.
2023;
1
(8)
:
1-15
.
View Article PubMed Google Scholar -
Zeybek
A.,
Ozkan
M.,
Alpay
M.,
Bilateral variations of the great saphenous vein. Marmara Medical Journal.
2021;
34
(2)
:
219-21
.
View Article Google Scholar -
Luo
L.,
Cai
Y.,
Zhang
Y.,
Hsu
C.G.,
Korshunov
V.A.,
Long
X.,
Role of PDE10A in vascular smooth muscle cell hyperplasia and pathological vascular remodelling. Cardiovascular Research.
2022;
118
(12)
:
2703-17
.
View Article PubMed Google Scholar -
Prim
D.A.,
Menon
V.,
Hasanian
S.,
Carter
L.,
Shazly
T.,
Potts
J.D.,
Perfusion tissue culture initiates differential remodeling of internal thoracic arteries, radial arteries, and saphenous veins. Journal of Vascular Research.
2018;
55
(5)
:
255-67
.
View Article PubMed Google Scholar -
Bifulco
K.,
Longanesi-Cattani
I.,
Gala
M.,
Carluccio
G. DI,
Masucci
M.T.,
Pavone
V.,
The soluble form of urokinase receptor promotes angiogenesis through its Ser88‐Arg‐Ser‐Arg‐Tyr92 chemotactic sequence. Journal of Thrombosis and Haemostasis.
2010;
8
(12)
:
2789-99
.
View Article PubMed Google Scholar -
Model
L.S.,
Hall
M.R.,
Wong
D.J.,
Muto
A.,
Kondo
Y.,
Ziegler
K.R.,
Arterial shear stress reduces eph-b4 expression in adult human veins. The Yale journal of biology and medicine.
2014;
87
(3)
:
359
.
PubMed Google Scholar -
Cai
Y.,
Knight
W.E.,
Guo
S.,
Li
J.D.,
Knight
P.A.,
Yan
C.,
Vinpocetine suppresses pathological vascular remodeling by inhibiting vascular smooth muscle cell proliferation and migration. The Journal of Pharmacology and Experimental Therapeutics.
2012;
343
(2)
:
479-88
.
View Article PubMed Google Scholar -
Price
D.K.,
Ando
Y.,
Kruger
E.A.,
Weiss
M.,
Figg
W.D.,
5'-OH-thalidomide, a metabolite of thalidomide, inhibits angiogenesis. Therapeutic Drug Monitoring.
2002;
24
(1)
:
104-10
.
View Article PubMed Google Scholar -
Pereira
M.M.,
Equine Endothelial Colony-Forming Cells: Phenotypic Enhancement and Ex vivo Angiogenesis Studies. International Journal of Molecular Sciences.
2024;
25
(11)
:
6017
.
PubMed Google Scholar -
Ramaesh
T.,
Logie
J.J.,
Roseweir
A.K.,
Millar
R.P.,
Walker
B.R.,
Hadoke
P.W.F.,
Kisspeptin-10 inhibits angiogenesis in human placental vessels ex vivo and endothelial cells in vitro. Endocrinology.
2010;
151
(12)
:
5927-34
.
View Article Google Scholar -
Seano
G.,
Primo
L.,
Human arterial ring angiogenesis assay. Methods in Molecular Biology (Clifton, N.J.).
2016;
1430
:
191-203
.
View Article PubMed Google Scholar -
Ghimire
K.,
Li
Y.,
Chiba
T.,
Julovi
S.M.,
Li
J.,
Ross
M.A.,
CD47 promotes age-associated deterioration in angiogenesis, blood flow and glucose homeostasis. Cells.
2020;
9
(7)
:
1695
.
View Article PubMed Google Scholar -
Seano
G.,
Chiaverina
G.,
Gagliardi
P.A.,
Blasio
L. Di,
Sessa
R.,
Bussolino
F.,
Modeling human tumor angiogenesis in a three-dimensional culture system. Blood, The Journal of the American Society of Hematology.
2013;
121
(21)
:
e129-37
.
View Article Google Scholar -
O'Neill
L.,
Rooney
P.,
Molloy
D.,
Connolly
M.,
McCormick
J.,
McCarthy
G.,
Regulation of inflammation and angiogenesis in giant cell arteritis by acute-phase serum amyloid A. Arthritis {&}amp; Rheumatology (Hoboken, N.J.).
2015;
67
(9)
:
2447-56
.
View Article PubMed Google Scholar -
Yang
C.,
Tahiri
H.,
Cai
C.,
Gu
M.,
Gagnon
C.,
Hardy
P.,
microRNA-181a inhibits ocular neovascularization by interfering with vascular endothelial growth factor expression. Cardiovascular Therapeutics.
2018;
36
(3)
:
e12329
.
View Article PubMed Google Scholar -
Moleiro
A.F.,
Conceição
G.,
Leite-Moreira
A.F.,
Rocha-Sousa
A.,
A critical analysis of the available in vitro and ex vivo methods to study retinal angiogenesis. Journal of Ophthalmology.
2017;
2017
:
3034953
.
View Article PubMed Google Scholar -
Pesce
N.A.,
Plastino
F.,
Reyes-Goya
C.,
Bernd
J.,
Pavone
V.,
Monte
M. Dal,
Mitigation of human iris angiogenesis through uPAR/LRP-1 interaction antagonism in an organotypic ex vivo model. FASEB Journal : Official Publication of the Federation of American Societies for Experimental Biology.
2024;
38
(5)
:
e23533
.
View Article PubMed Google Scholar -
Popovic
N.,
Hooker
E.,
Barabino
A.,
Flamier
A.,
Provost
F.,
Buscarlet
M.,
COCO/DAND5 inhibits developmental and pathological ocular angiogenesis. EMBO Molecular Medicine.
2021;
13
(3)
:
e12005
.
View Article PubMed Google Scholar -
Knott
R.M.,
Robertson
M.,
Muckersie
E.,
Folefac
V.A.,
Fairhurst
F.E.,
Wileman
S.M.,
A model system for the study of human retinal angiogenesis: activation of monocytes and endothelial cells and the association with the expression of the monocarboxylate transporter type 1 (MCT-1). Diabetologia.
1999;
42
(7)
:
870-7
.
View Article PubMed Google Scholar -
Liu
Y.,
Huang
N.,
Liao
S.,
Rothzerg
E.,
Yao
F.,
Li
Y.,
Current research progress in targeted anti‐angiogenesis therapy for osteosarcoma. Cell proliferation.
2021;
54
(9)
:
e13102
.
View Article Google Scholar -
Navid
F.,
Santana
V.M.,
Neel
M.,
McCarville
M.B.,
Shulkin
B.L.,
Wu
J.,
A phase II trial evaluating the feasibility of adding bevacizumab to standard osteosarcoma therapy. International journal of cancer.
2017;
141
(7)
:
1469-77
.
View Article Google Scholar -
Bandello
F.,
Augustin
A.,
Tufail
A.,
Leaback
R.,
A 12-month, multicenter, parallel group comparison of dexamethasone intravitreal implant versus ranibizumab in branch retinal vein occlusion. European Journal of Ophthalmology.
2018;
28
(6)
:
697-705
.
View Article PubMed Google Scholar -
Gupta
P.K.,
Shivashankar
P.,
Rajkumar
M.,
Mahapatra
S.S.,
Desai
S.C.,
Dhar
A.,
Label extension, single-arm, phase III study shows efficacy and safety of stempeucel\textregistered in patients with critical limb ischemia due to atherosclerotic peripheral arterial disease. Stem Cell Research {&}amp; Therapy.
2023;
14
(1)
:
60
.
View Article PubMed Google Scholar -
Atkins
M.B.,
Plimack
E.R.,
Puzanov
I.,
Fishman
M.N.,
McDermott
D.F.,
Cho
D.C.,
Axitinib in combination with pembrolizumab in patients with advanced renal cell cancer: a non-randomised, open-label, dose-finding, and dose-expansion phase 1b trial. The Lancet Oncology.
2018;
19
(3)
:
405-15
.
View Article Google Scholar -
Woei-A-Jin
F.J.S.H.,
Weijl
N.I.,
Burgmans
M.C.,
Sarasqueta
A. Fariña,
Wezel
J.T. van,
Wasser
M.N.J.M.,
Neoadjuvant treatment with angiogenesis-inhibitor dovitinib prior to local therapy in hepatocellular carcinoma: a phase II study. The Oncologist.
2021;
26
(10)
:
854-64
.
View Article Google Scholar -
Hartikainen
J.,
Hassinen
I.,
Hedman
A.,
Kivelä
A.,
Saraste
A.,
Knuuti
J.,
Adenoviral intramyocardial VEGF-DΔNΔC gene transfer increases myocardial perfusion reserve in refractory angina patients: a phase I/IIa study with 1-year follow-up. European Heart Journal.
2017;
38
(33)
:
2547-55
.
View Article PubMed Google Scholar -
Walker
R.L.,
Human and animal subjects of research: the moral significance of respect versus welfare. Theoretical Medicine and Bioethics.
2006;
27
(4)
:
305-31
.
View Article PubMed Google Scholar -
Grizzle
W.E.,
Bell
W.C.,
Sexton
K.C.,
Issues in collecting, processing and storing human tissues and associated information to support biomedical research. Cancer Biomarkers.
2010;
9
(1-6)
:
531-49
.
View Article Google Scholar -
Esparza
A.,
Jimenez
N.,
Borrego
E.A.,
Browne
S.,
Natividad-Diaz
S.L.,
Human stem cell-based 3D in vitro angiogenesis models for preclinical drug screening applications. Molecular Biology Reports. .
2024;
51
(1)
:
260
.
View Article Google Scholar
Comments
Article Details
Volume & Issue : Vol 12 No 4 (2025)
Page No.: 7304-7319
Published on: 2025-04-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 67 times
- PDF downloaded - 17 times
- XML downloaded - 11 times
 Biomedpress
Biomedpress






