Abstract
Introduction: Thyroid hormones are major contributors to numerous physiological processes in the body. Thyroid disorders are frequently associated with an imbalance in the homeostasis of calcium and phosphorus. The objective of this study is to evaluate and compare the mineral status of hypothyroid patients and euthyroid controls by determining the serum levels of calcium, magnesium, and phosphorus. The aim is to identify any significant differences in the concentrations of these minerals between hypothyroid individuals and healthy controls, thereby contributing to a better understanding of the potential metabolic disturbances associated with hypothyroidism.
Methods: A prospective case-control study was conducted at Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu. It involved 35 hypothyroidism cases and 35 euthyroid controls attending the outpatient department, aged 18-45 years. The control group had normal Thyroid-Stimulating Hormone (TSH) and Free Thyroxine (FT4) levels, while the case group had hypothyroidism, diagnosed by increased TSH levels and decreased FT4. Serum samples were evaluated for TSH, Free Triiodothyronine (FT3), FT4, calcium, magnesium, and phosphorus in both case and control groups.
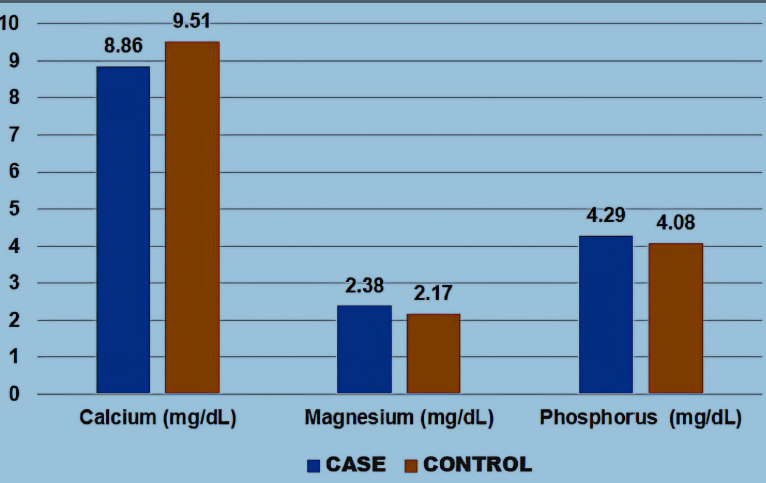
Results: Serum calcium levels were found to be significantly decreased (p<0.001) and serum magnesium and phosphorus were found to be slightly elevated (p>0.05) in the hypothyroid cases compared to euthyroid controls. Calcium positively correlated with FT3 and negatively correlated with FT4, while phosphorus levels positively correlated with TSH levels and negatively correlated with FT4, calcium, and magnesium levels.
Conclusion: Hypothyroid individuals have an altered mineral profile, necessitating comprehensive treatment procedures and monitoring of serum levels. Early assessment of mineral status in terms of calcium, magnesium, and phosphorus can aid in the treatment and management of hypothyroidism, preventing further complications.
Introduction
Thyroid function is crucial for regulating cellular activity and body metabolism, but dysfunction can lead to dyslipidemia and mineral metabolism issues. Hypothyroidism can cause hypercholesterolemia, elevated LDL levels, and hypertriglyceridemia, increasing the risk of cardiovascular diseases due to adverse lipid profiles and metabolic changes1. Thyroid hormones, triiodothyronine (T3) and tetraiodothyronine (T4), also known as thyroxine, are secreted by the thyroid gland and play a crucial role in regulating body temperature, metabolism, and hemodynamics. Thyroid Stimulating Hormone (TSH) and Thyrotropin Releasing Hormone (TRH) are released by the pituitary gland and hypothalamus, helping to regulate T3 and T4 levels2.
Hypothyroidism is a condition where thyroid hormones T3 and T4 are circulated at lower than normal levels, leading to increased TSH levels. Symptoms appear when TSH exceeds 10 mIU/L. In subclinical hypothyroidism, TSH levels are elevated to some extent, while T3 and T4 remain within their normal ranges in the serum. The frequency of hypothyroidism increases with age and is more prevalent among women3, 4.
Hypothyroidism, a prevalent endocrine disorder globally, affects 10-11% of Indians. It is caused by decreased thyroid hormone levels, leading to mental and physical slowdown5. In India, endocrine disorders affect 108 million people, with hypothyroidism being more common than hyperthyroidism6.
Thyroid hormones control various metabolic pathways that require calcium, phosphate, magnesium, and zinc. In hypothyroidism, decreased calcium release from bone cells results in lower blood calcium levels, which stimulates an increase in calcitonin. This increase, in turn, enhances phosphate reabsorption and leads to greater urinary excretion of calcium, often causing hyperphosphatemia alongside reduced calcium levels7. Zinc modulates thyroid hormone synthesis, secretion, bioavailability, and activity, while magnesium influences membrane permeability and thyroid hormone secretion. Their metabolism and clearance are influenced by thyroid hormones as well8, 9. Magnesium is vital for activating enzymes like adenyl cyclase and plays a role in the thyroid’s response to hormones through the cAMP pathway. It also contributes to antioxidant defense and is essential for mitochondrial function, especially in oxidative phosphorylation7.
Thyroid hormones stimulate bone turnover, leading to decreased bone mineral density, increased risk of osteoporotic fractures, and disturbed serum calcium and phosphate levels1, 10. Hypothyroidism, a biochemical condition resulting from thyroid hormone insufficiency, slows down metabolic processes, including water, salt, potassium, and chloride absorption, as well as renal blood flow. The effect of thyroid hormones on electrolyte balances is not fully elucidated9. The objective of this study is to evaluate and compare the mineral status of hypothyroid patients and euthyroid controls by determining the serum levels of calcium, magnesium, and phosphorus. The aim is to identify any significant differences in the concentrations of these minerals between hypothyroid individuals and healthy controls, thereby contributing to a better understanding of the potential metabolic disturbances associated with hypothyroidism.
Methods
Study Design
This prospective case-control study was conducted at Sri Ramachandra Institute of Higher Education and Research, Chennai, Tamil Nadu, India.
Sample Size
The sample size for this study was determined using a power analysis based on previous research on thyroid function and mineral status in hypothyroid patients. The study comprises a total of 70 patients attending the outpatient department, among them 35 were hypothyroid patients and 35 were euthyroid controls. The study evaluated thyroid status in patients aged 18-45, focusing on those with hypothyroidism.
Inclusion and Exclusion Criteria
Normal TSH (0.5–5 µIU/mL) and Free T4 (0.75–1.54 ng/dL) levels were measured, while hypothyroidism was diagnosed by increased TSH (> 5 µIU/mL) levels and decreased FT4 (< 0.75 ng/dL) levels. Patients diagnosed with hypothyroidism within a year were included in the case group, and hypothyroidism patients on treatment for a long period were excluded from the study. The study also excluded patients with hospital admission, diabetes mellitus, liver disease, chronic renal failure, diuretics, magnesium supplements, antacids, malabsorption, chronic diarrhea, and a history of epilepsy.
Sample Storage and Collection
Venous blood was collected using a disposable vacutainer system in a fasting state, ensuring aseptic precautions, and stored at -20 degrees Celsius for further analysis.
Analytical Methodology
Free T3, Free T4, TSH, calcium, magnesium, and phosphorus levels were assayed. Thyroid hormones were assayed using the ECLIA method in the Roche Cobas e602 analyzer; calcium using the Arsenazo III method in the Beckman Coulter AU 5800 analyzer; magnesium using the Xylidyl blue method in the Beckman Coulter AU 5800 analyzer, and phosphorus using the phosphomolybdate method in the Beckman Coulter AU 5800 analyzer.
Statistical Analysis
SPSS version 18.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis with a significance level set at p < 0.05. Independent sample T-tests and Karl Pearson's correlation coefficient were used to determine differences between case and control groups.
| Characteristics | Case (n = 35) | Control (n = 35) Mean ± Standard deviation | p-value | |
|---|---|---|---|---|
| Age (years) | 57 ± 17 | 50 ± 16 | >0.05 | Not significant |
| FT3 (pg/mL) | 2.17 ± 1.11 | 2.86 ± 0.64 | >0.05 | Significant |
| FT4 (ng/dL) | 0.88 ± 0.21 | 1.29 ± 0.18 | <0.001 | Highly significant |
| TSH (µIU/mL) | 17.93 ± 18.69 | 1.99 ± 0.85 | <0.001 | Highly significant |
| Calcium (mg/dL) | 8.86 ± 0.77 | 9.51± 0.74 | <0.001 | Highly significant |
| Magnesium (mg/dL) | 2.38 ±0.93 | 2.17 ± 0.72 | >0.05 | Not significant |
| Phosphorus (mg/dL) | 4.29 ± 1.77 | 4.08 ±1.00 | >0.05 | Not significant |
Results
Normality of the data distribution was investigated using the Shapiro-Wilk test. Mean and standard deviation were calculated for all parameters. An independent sample T-test was performed, and a two-tailed p-value of < 0.05 was considered statistically significant. A p-value < 0.05 was considered statistically significant, and a p-value < 0.001 was considered highly significant. Karl Pearson’s correlations were analyzed to determine the relationship between risk variables.
Population characteristics were calculated for both case and control groups and tabulated (Table 1 ). Thirty-five hypothyroid individuals formed the case group, and thirty-five euthyroid individuals formed the control group. A pie chart representing the gender percentage in both case and control groups is shown (Figure 1 ).
From Table 1, the control group of euthyroid subjects had an average age of 51, while the case group had an average age of 57. The mean value of TSH in the control group was 1.99 µIU/mL, and the FT4 values were 1.29 ng/dL. The case group, consisting of hypothyroid patients, had a TSH value of 22.58 µIU/mL and FT4 values of 0.88 ng/dL. The case group had average calcium, magnesium, and potassium levels of 8.86 mg/dL, 2.38 mg/dL, and 4.29 mg/dL, respectively, while the control group had average values of 9.51 mg/dL, 2.17 mg/dL, and 4.08 mg/dL, respectively.
A Raincloud Plot represents the distribution of data for all parameters, with the case group compared to the control group (Figure 2 ). The bar graph from Figure 3 represents the serum calcium, magnesium, and potassium levels in cases (hypothyroidism patients) and controls (euthyroid subjects). These results revealed a significant decrease in calcium levels in the hypothyroid case group compared to the healthy control group, and slightly increased levels of magnesium and potassium were observed in cases compared to healthy controls.
Discussion
Hypothyroidism, a condition characterized by disturbances in mineral metabolism, can lead to bone loss, osteoporosis, metabolic syndrome, and cardiovascular diseases7. Subclinical hypothyroidism, which is defined as elevated serum thyroid-stimulating hormone (TSH) levels with normal levels of free thyroxine (FT4), affects up to 10% of the adult population. Subclinical hypothyroidism, which involves mildly low thyroid function but elevated TSH levels, affects up to 18% of the elderly, with a higher prevalence in women compared to men5.
This study comprises predominantly women with hypothyroidism, accounting for 63%, and only 37% were male patients. A previous study states that the majority were women, with a higher prevalence of hypothyroidism in the 20-30 age group. Female hypothyroid patients accounted for 78.3% of the total, with 30% aged 20-30, 18% aged 30-40, 25% aged 40-50, and 27% aged 50-602. This reveals that female patients have a higher prevalence of hypothyroidism than males.
Hypothyroidism is a condition where thyroid hormones regulate calcium levels in the blood. Patients experience hypocalcemia, a decrease in calcium outflow due to lower thyroxine levels. This leads to increased calcitonin production, promoting calcium clearance and phosphate absorption. Hypothyroidism can also cause magnesium metabolism disturbances, leading to metabolic syndrome and cardiovascular diseases10, 11.
This study shows significantly decreased calcium levels in cases (8.86 ± 0.77 mg/dL) compared to controls (9.51 ± 0.74 mg/dL) (p < 0.001). Calcium positively correlated with FT3 and negatively correlated with TSH levels. A study by Padhiary et al. showed statistically significant elevated levels of phosphorus and magnesium and decreased calcium levels in hypothyroidism patients when compared to controls (p < 0.001)12.
A study by Bushra et al. found a significant decrease in serum calcium levels in hypothyroidism patients (8.06 ± 0.99 mg/dL) compared to healthy controls (9.1 ± 0.67 mg/dL), possibly due to a low level of thyroxine, a hormone that plays a crucial role in calcium homeostasis2. Our findings are similar to previous studies by Saxena S, et al. (case 8.0 ± 8.4 mg/dL vs. control 8.6 ± 9.6 mg/dL)8, and Sridevi D et al. (8.58 ± 0.46 mg/dL vs. 10.04 ± 0.56 mg/dL)13. These studies suggest that thyroid hormones significantly impact mineral levels in hypothyroid patients, and regular follow-ups in cases of thyroid hormone deficit may help manage it. However, Susanna TY, et al. (case 8.98 ± 0.61 mg/dL vs. controls 8.98 ± 0.49 mg/dL) found no change in serum calcium levels in hypothyroidism patients compared to healthy controls. A 2024 study by Turanjanin D et al. showed positive and similar results to this present study (8.86 ± 0.52 mg/dL vs. 9.50 ± 0.44 mg/dL)7. These findings highlight the importance of monitoring and managing thyroid hormone deficits in managing hypothyroidism14.
A study by Bushra et al. reveals that hypothyroid patients have significantly elevated levels of serum magnesium (2.63 ± 0.57 mg/dL) compared to controls (2.36 ± 0.65 mg/dL). This results in increased renal retention of up to 30% from the kidneys and can be attributed to the increased reabsorption of magnesium by thyroid hormones, which impacts renal tubules2. Similarly, our study showed slightly elevated magnesium levels in the case group (2.38 ± 0.93 mg/dL) compared to the control group (2.17 ± 0.72 mg/dL). A study by Saxena S, et al. also reveals increased levels of magnesium in hypothyroid patients than in healthy controls (median of 2.0 mg/dL vs. 1.8 mg/dL)8. Early detection and treatment can help prevent additional bone complications. However, a study by Abdel-Gayoum provides contradicting findings, showing that magnesium levels in subclinical hypothyroid patients (0.83 ± 0.08 mg/dL) are reduced compared to euthyroids (0.84 ± 0.06 mg/dL), and overt hypothyroid patients show a slight increase compared to euthyroids (0.85 ± 0.06 mg/dL)1. The results of our study show increased magnesium levels in hypothyroid patients compared to euthyroid controls, whereas a 2024 study by Turanjanin D et al. reports decreased levels of magnesium in hypothyroid patients (Case 1.58 ± 0.19 vs. Control 2.02 ± 0.1). This discrepancy may have occurred due to several factors, including differences in patient populations, dietary intake, and regional variations in mineral availability7. The study suggests that monitoring serum magnesium levels in hypothyroid patients can help reduce the adverse consequences of magnesium insufficiency in hypothyroid individuals.
Our study found slightly elevated levels of phosphorus in the hypothyroid case group (4.29 ± 1.77 mg/dL) compared to the euthyroid control group (4.08 ±1.00 mg/dL) and found a robust positive correlation with TSH and a negative correlation with FT4, calcium, and magnesium levels. Similarly, the Bushra et al. study found a significant increase in serum phosphorus levels in hypothyroid patients (6.79 ± 1.04 mg/dL) compared to controls (4.22 ± 1.23 mg/dL)2. Our finding is also similar to previous research by Susanna TY et al. (2016), which showed significantly higher (p < 0.001) levels of phosphorus in hypothyroid cases (5.56 ± 2.03 mg/dL) than in healthy individuals (3.10 ± 0.50 mg/dL)15. The study by Majid et al. also supports our study findings, showing higher levels of phosphorus in hypothyroid patients (3.25 ± 0.58 mg/dL) compared to controls (3.51 ± 0.51 mg/dL)14. A recent study by Turanjanin D et al. reported similar results to our study (Case 3.69 ± 0.37 mg/dL vs. Control 3.53 ± 0.12 mg/dL)7. The increase in serum phosphorus levels could be attributed to increased calcitonin synthesis, which leads to increased tubular phosphate reabsorption and excretion, resulting in hypocalcemia and hyperphosphatemia, as seen in hypothyroidism.
Conclusions
This study concludes that hypothyroid people have an altered mineral profile. Developing and framing comprehensive treatment procedures and emphasizing the necessity of monitoring these minerals' serum levels during follow-up are necessary. Hypocalcemia, hypermagnesemia, and hyperphosphatemia conditions were observed in hypothyroid patients. Early assessment of mineral status can aid in the treatment and management of hypothyroidism and can prevent further complications. If consistent mineral imbalances in hypothyroid patients are observed, it may necessitate updating clinical guidelines to include routine monitoring of mineral levels, potentially improving patient outcomes and offering personalized treatment strategies.
Future research should focus on long-term, longitudinal studies to monitor mineral levels in hypothyroid patients before, during, and after treatment. It should also explore the role of other trace elements, such as selenium, copper, and zinc, in hypothyroidism. Subgroup analysis should be considered, taking into account subclinical vs. overt hypothyroidism, age, gender, and comorbidities. Clinical trials should explore whether mineral supplementation can improve clinical outcomes in hypothyroidism. Studies should explore the biochemical pathways through which hypothyroidism impacts mineral metabolism.
The primarily small sample size poses a limitation of this study. Further studies may include a larger sample size, and additionally, minerals such as zinc, iron, and iodine can also be studied along with the electrolyte profile in hypothyroid patients.
Abbreviations
FT3: Free triiodothyronine, FT4: free thyroxine, mg/dL: milligrams Per Deciliter, ng/dL: nanograms per decilitre, pg/mL: picograms per millilitre, TRH: Thyrotropin Releasing Hormone, TSH: Thyroid stimulating hormone, µIU/mL: micro-international units per milliliter
Acknowledgments
None.
Author’s contributions
NR, DS, SS, SK and SK, equally contributed to the conception and design of the research. NR, DS and SS contributed to the acquisition and analysis of the data. NR, DS, SS, SK and SK contributed to the interpretation of the data. DS, SS SK and SK drafted the manuscript. All authors critically revised the manuscript, agreed to be fully accountable for ensuring the integrity and accuracy of the work, and read and approved the final manuscript. SS accepts full responsibility for the finished work and the conduct of the study, has access to the data, and controls the decision to publish. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Institutional Ethics Committee of Sri Ramachandra Institute of Higher Education and Research (Date: 2024-09-19, No: CSP/22/AUG/115/449) and written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Abdel-Gayoum
A.A.,
Dyslipidemia and serum mineral profiles in patients with thyroid disorders. Saudi Medical Journal.
2014;
35
(12)
:
1469-76
.
PubMed Google Scholar -
Bushra
S.K.,
Jamal
F.,
Study of mineral profile in patients with hypothyroidism. International Journal of Advanced Biochemistry Research.
2022;
6
(1)
:
55-60
.
View Article Google Scholar -
Vasanthan
M.,
Vinodhini
V.,
Bone Mineral Status in Sub-clinical Hypothyroidism: A Case-control Study. Journal of Clinical and Diagnostic Research : JCDR.
2021;
15
(2)
:
09
.
View Article Google Scholar -
Zahra
N.,
Ali
A.,
Kousar
S.,
Malik
A.,
Zaheer
A.,
Malik
I.R.,
Study on significant changes in calcium, phosphorus and thyroid hormones level in hypothyroidism patients. Advancements in Life Sciences.
2020;
8
(1)
:
85-8
.
-
Jat
R.K.,
Panwar
A.K.,
Agarwal
P.,
Sharma
C.,
Bansal
D.P.,
Pareek
A.,
Assessment of Serum Minerals in Subclinical Hypothyroid and Overt Hypothyroid Patients. Cureus.
2021;
13
(8)
:
e16944
.
View Article PubMed Google Scholar -
Vasanthan
M.,
A Study of Mineral Status in Hypothyroidism. Journal of Medical Science and Clinical Research.
2018;
6
(11)
:
66
.
View Article Google Scholar -
Turanjanin
D.,
Mijovic
R.,
Star\vcević
I.,
Tatalovic
V.,
Calcium and magnesium levels in patients with primary hypothyroidism. Medicinski Pregled.
2024;
77
(3-4)
:
106-12
.
View Article Google Scholar -
Saxena
S.,
Srivastava
P.C.,
Katyal
R.,
Das
B.,
Pannu
S.J.,
Evaluation of mineral status in hypothyroidism in a tertiary care centre. International Journal of Research in Medical Sciences.
2020;
8
(2)
:
667-71
.
View Article Google Scholar -
Sivakumar
S.,
Bhargavi
S.K.,
Naidu
M. Prasad,
Study of Serum Calcium, Magnesium and Phosphorous Levels in Hypothyroidism. Scholars International Journal of Biochemistry.
2020;
03
(02)
:
22-6
.
View Article Google Scholar -
Chatterjee
S.,
Chakrabarti
P.,
Lokanathan
V.,
Calcium and Magnesium Levels in Subclinical and Overt Hypothyroidism: A Cross-sectional Study. Journal of Clinical and Diagnostic Research : JCDR.
2023;
17
(9)
:
BC15 -BC17
.
View Article Google Scholar -
Pattanashetti
S.B.,
Krishnappa
P.,
Serum Electrolytes in Subclinical Hypothyroidism and Subclinical Hyperthyroidism. Indian Journal of Medical Biochemistry.
2021;
25
(1)
:
1-4
.
View Article Google Scholar -
Padhiary
M.,
Mishra
T.,
Mohanty
R.R.,
Mishra
S.,
Mishra
S. Kumar,
Study of serum electrolytes and minerals in hypothyroidism. International Journal of Medical Research and Review.
2016;
4
(7)
:
1189-93
.
View Article Google Scholar -
Sridevi
D.,
Dambal
A.A.,
Sidrah
undefined,
Challa
A.S.,
Padaki
S.K.,
A Study of Serum Magnesium, Calcium and Phosphorus in Hypothyroidism. https://doi.org/10.5958/2394-6377.2016.00045.9.
2016;
3
(2)
:
236-239
.
View Article Google Scholar -
Majid
W.,
Saeed
M.N.,
Hussein
M.A.,
A Case Control Study to Evaluate the Levels of Vitamin D, Calcium, Parathyroid Hormone, Phosphate, and Demographic Characteristics of Patients with Hypothyroidism. Annals of the Romanian Society for Cell Biology.
2021;
25
(6)
:
3143-52
.
-
Susanna
T.Y.,
Sagayaraj
A.,
Shashidhar
K.N.,
Gomathi
M.,
Mahesh
V.,
A correlative study of thyroid profile and mineral status in patients with hypothyroidism - A hospital-based case control study. Asian Journal of Pharmaceutical and Clinical Research.
2016;
9
(3)
:
292-4
.
Comments
Article Details
Volume & Issue : Vol 12 No 2 (2025)
Page No.: 7118-7124
Published on: 2025-02-28
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 1053 times
- PDF downloaded - 384 times
- XML downloaded - 88 times
 Biomedpress
Biomedpress





