Abstract
Background: Coronaviruses (CoVs) are members of the Nidovirales family, Coronaviridae. To date, seven human CoVs have been identified, some of which are known to circulate persistently in the human population, particularly among young infants. Among these CoV types, renal disease is a recognized complication associated with SARS-CoV-2. No cases of renal disease caused by HCoVNL63 have been reported.
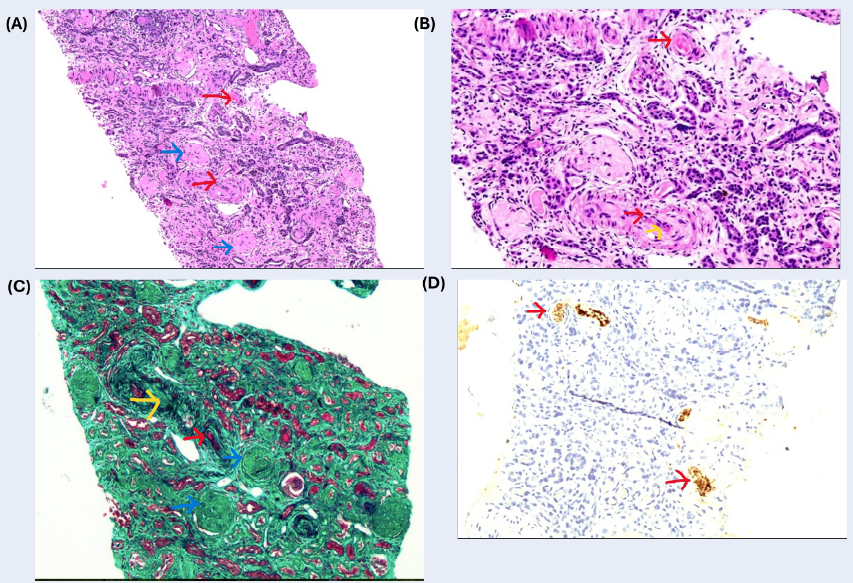
Case report: A 4-year-old girl presented with severe renal injury and cardiorespiratory collapse as a result of HCoV-NL63-associated glomerulonephritis. Histopathology from a renal biopsy revealed severe tubulointerstitial changes. She was subsequently placed on continuous ambulatory peritoneal dialysis (CAPD) with a Tenckhoff catheter as a long-term renal replacement therapy due to her incomplete recovery.
Conclusion: HCoV-NL63, previously identified as causing moderate respiratory symptoms in infants, is capable of inducing severe renal impairment in childhood. Histopathological findings in the renal area are critical in determining the pathology of this rare etiology that causes childhood glomerulonephritis. This report emphasizes the novelty and importance of this rare case in pediatric nephrology.
Introduction
Coronaviruses (CoVs) are members of the Nidovirales family, within the Coronaviridae subfamily. CoVs are positive-strand RNA viruses with large genomes ranging in size from 27 to 33 kb1. To date, seven human CoVs have been identified, some of which persistently circulate in the human population, particularly among young infants. Initially detected in the mid-1960s, HCoV-229E and HCoV-OC43 have been associated with the common cold and, in rare cases, with lower respiratory tract infections2. In 2003, a third human coronavirus (SARS-CoV) was identified as the causative agent of severe acute respiratory syndrome (SARS)1. HCoV-NL63 and HCoV-HKU1 were two additional human coronaviruses identified after 20031. The Middle East respiratory syndrome coronavirus (MERS-CoV) emerged in the Arabian Peninsula in 2012 as a highly lethal human pathogen2. The novel coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), was discovered in Wuhan, China, in 2019 and has since caused a global pandemic3. Among these CoV types, renal disease has been recognized as a complication associated with SARS-CoV-2, as previously reported by Lv W et al.2. Specific studies directly correlating HCoV-NL63 with renal impairment in pediatric patients are limited. While some children with HCoV-NL63 infections have underlying health issues, including renal problems, the majority of research focuses on respiratory outcomes, and the direct causative relationship remains to be established. We present the case of a 4-year-old girl who presented with severe renal injury and cardiorespiratory collapse as a result of HCoV-NL63-associated glomerulonephritis. We have reviewed the associated pathology of the underlying disease.
Methods
A 4-year-old girl presented with a sudden onset of cardiorespiratory collapse following a 2-day history of cough, coryza, loose stools, and vomiting. The patient exhibited severe acute renal injury (ARI) and hepatorenal syndrome, complicating her condition. She was ventilated due to respiratory failure and hemodynamic instability. She had anuric renal failure and received continuous veno-venous hemofiltration (CVVH) via a right internal jugular vein catheter for five days.rd percentile). She appeared sallow and was not edematous. She was afebrile and hypertensive, with a pulse rate of 100 beats per minute and a blood pressure of 160/100 mmHg. Her skin was dry, with scabs from a previous skin infection covering her body. Lung auscultation revealed diminished breath sounds bilaterally. The remaining systemic examinations were inconclusive.
| 27/5/23 | 10/6/23 | 13/6/23 | 15/6/23 | 23/6/23 | |
| WBC ꝉ (10 9 /L) | 16.4 | 30.28 | 15.5 | 10.28 | 20.8 |
| Haemoglobin (g/dL) | 5.4 | 12.8 | 9.9 | 9.7 | 9.1 |
| Haematocrit | 15.9 | 38.2 | 30.9 | 30.7 | 27.7 |
| Platelet (10 9 /L) | 250 | 1097 | 929 | 847 | 728 |
| Sodium | 137 | 140 | 142 | 142 | 138 |
| Potassium | 5.2 | 2.9 | 3.5 | 4.9 | 4.7 |
| Urea | 45.9 | 23 | 24.4 | 23 | 17.3 |
| Creatinine | 1467 | 800 | 715 | 496 | 446 |
| Calcium | 1.85 | 2.45 | 2.32 | 2.38 | 2.17 |
| Phosphate | 5.43 | 1.56 | 2.19 | 1.54 | 1.88 |
| ALP ‡ | 110 | 136 | 108 | 117 | 162 |
| Albumin | 20 | 41 | 32 | 38 | |
| CRP § | <5 | 27.7 | |||
| LDH ¶ | 1892 | 650 | |||
| INR ꝉ | 1.5 | 0.89 | |||
| APTT ‡ | 52.3 | 37.9 | |||
| PT § | 19.7 | 12.2 | |||
| C3 | 0.43 | ||||
| C4 | <0.08 | ||||
| ANA ¶ | Negative | ||||
| ASOT ꝉ | Negative |
Table 1 shows that a creatinine level of 1467 µmol/L and an estimated glomerular filtration rate (eGFR) of 2.5 ml/min/1.73 m² indicated renal impairment. Urine analysis revealed hematuria and proteinuria, with red blood cell (RBC) and protein levels of 3+, respectively. The peripheral blood film demonstrated a leukoerythroblastic pattern accompanied by neutrophilia and left-shifted red blood cell alterations, all indicative of infection. The results of all autoantibody assays were negative. HCoV-NL63 was identified as the respiratory pathogen by rapid molecular detection. A chest radiograph showed left pleural effusion and right loculated pneumothorax, for which a left-sided chest tube was inserted. Pleural fluid examination revealed an exudative type with no positive culture. Abdominal and kidney-ureter-bladder (KUB) ultrasounds indicated bilateral renal and liver parenchymal disease. Brain computed tomography (CT) revealed no abnormalities. Because of the lack of improvement in renal function despite consistent hemodialysis, a renal biopsy was performed on the patient's left kidney. Histopathological (HPE) analysis of the kidney biopsy indicated that, of the 60 glomeruli examined, 55 showed global sclerosis, and only five remained viable (Figure 1). Active lesions, including crescent formation, endocapillary hypercellularity, and necrotizing lesions, were not observed. Tubular atrophy and interstitial fibrosis, comprising moderate to severe chronic tubulointerstitial changes, were observed in over 50% of the biopsy with diffuse acute tubular injury changes. Moderate chronic vascular changes were noted in the vessels, manifesting as fibro-myxoid changes and thickened wall thickness. Immunohistochemistry stains for CD61 indicated the existence of fibrin thrombi within the vessels' lumen. She received 30 mg/kg body weight of intravenous (IV) methylprednisolone per day for three days. An angiotensin-converting enzyme inhibitor, a beta-blocker, and a calcium channel blocker were administered to regulate her blood pressure. In addition to packed cell transfusions administered during hemodialysis, the patient underwent intravenous infusions of iron sucrose to treat her anemia. The patient's renal function did not fully recover, necessitating renal replacement therapy (RRT). Given the challenges with accessing veins and the cost-effectiveness of the option, she was transitioned to continuous ambulatory peritoneal dialysis (CAPD) using a Tenckhoff catheter as her long-term RRT.
Discussion
HCoV-NL63 is the fifth discovered human coronavirus and, unlike SARS-CoV-2, it produces mild respiratory illnesses in infants1. Researchers in Amsterdam initially identified HCoV-NL63 in 2004 from a nasopharyngeal aspirate of a seven-month-old infant4. The existing literature provides limited information regarding its association with severe renal manifestations. In this case, the most plausible pathogenic etiology of the renal impairment was glomerulonephritis caused by HCoV-NL63. Given the patient's abrupt onset of acute kidney injury (AKI) and histopathological examination (HPE) analysis, the most plausible diagnosis is rapidly progressive glomerulonephritis (RPGN), potentially caused by HCoV-NL63. RPGN is marked by a sudden loss of renal function over days or weeks, evident in the urine (proteinuria, micro, or macroscopic hematuria, dysmorphic red blood cells (RBC), RBC casts), and also in the kidneys' histopathological features of crescentic glomeruli5. Without treatment, RPGN can advance to renal failure within weeks or months. Consequently, immediate treatment is essential, consisting of at least three doses of pulsed IV methylprednisolone and plasmapheresis5.
Three of these coronaviruses, namely COVID-19, SARS, and MERS, have spread and caused exceptionally hazardous diseases4. The remaining four, HCoV-229E, HCoV-OC43, HCoV-NL63, and HCoV-HKU1, are mildly pathogenic and induce just common cold symptoms in immunocompetent persons4. Patients infected with SARS-CoV, MERS-CoV, or SARS-CoV-2 may present with acute respiratory illness (ARI), although retrospective studies have not consistently reported the incidence of ARI. They hypothesize that a pro-inflammatory cytokine response or viral replication-mediated renal cytopathy could directly or indirectly induce ARI based on their analysis of ARI reports associated with SARS-CoV, MERS-CoV, and SARS-CoV-2 infections2. Lednicky et al. discovered HCoV-NL63 in commercially available primary human renal proximal tubule epithelial cells (RPTEC)6 and subsequently demonstrated that the virus replicates in primary human kidney cells at high titers6. Despite its classification as a respiratory virus with moderate virulence, HCoV-NL63 has not been associated with renal disease in humans6. SARS and MERS coronaviruses, on the other hand, are genetically related and are responsible for inducing severe respiratory and renal diseases3. This leads to an inquiry into whether HCoV-NL63 impacts the kidneys. Previous studies have linked SARS-CoV, which possesses the identical ACE2 receptor as HCoV-NL63, to kidney disease6. It is conceivable that HCoV-NL63 is also capable of inducing kidney disease, albeit with considerably less severity compared to SARS-CoV. HCoV-NL63 may contribute to renal impairment by causing direct viral effects on the renal epithelial cells, a systemic inflammatory response, and co-infection with other viruses or bacteria7. Given the potential for HCoV-NL63 to contribute to renal impairment, clinicians should be vigilant in monitoring renal function in pediatric patients diagnosed with HCoV-NL63 infections. Despite undergoing dialysis, this patient's kidney function has become irreversible, resulting in a poor prognosis. This patient may be a candidate for a renal transplant, which we need to discuss further with the parents.
CONCLUSION
The case of HCoV-NL63's potential renal impacts serves as a reminder of the need for ongoing research and the development of clinical guidelines that address the multifaceted effects of respiratory viruses in pediatric patients. By enhancing our understanding and management of these infections, we can improve outcomes and the quality of life for affected children.
Abbreviations
ACE2 - Angiotensin-Converting Enzyme 2, AKI - Acute Kidney Injury, ARI - Acute Renal Injury, CAPD - Continuous Ambulatory Peritoneal Dialysis, CoV - Coronavirus, CoVs - Coronaviruses, COVID-19 - Coronavirus Disease 2019, CT - Computed Tomography, CVVH - Continuous Veno-Venous Hemofiltratione, GFR - Estimated Glomerular Filtration Rate, HCoV-NL63 - Human Coronavirus NL63, HPE - Histopathological Examination, IV - Intravenous, KUB - Kidney-Ureter-Bladder, MERS-CoV - Middle East Respiratory Syndrome Coronavirus, µmol/L - Micromoles Per Liter, RBC - Red Blood Cells, RPTEC - Renal Proximal Tubule Epithelial Cells, RPGN - Rapidly Progressive Glomerulonephritis, RRT - Renal Replacement Therapy, SARS-CoV - Severe Acute Respiratory Syndrome Coronavirus, SARS-CoV-2 - Severe Acute Respiratory Syndrome Coronavirus 2
Acknowledgments
None.
Author’s contributions
AMMK and MII participate in drafting the case report. KI and NACJ creating the outline of the case. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the parents of the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Li
X.,
Luk
H.K.,
Lau
S.K.,
Woo
P.C.,
Human Coronaviruses: General Features. Reference Module in Biomedical Sciences.
2019;
2019
:
B978-0-12-801238-3.95704-0
.
View Article PubMed Google Scholar -
Lv
W.,
Wu
M.,
Ren
Y.,
Zeng
N.,
Deng
P.,
Zeng
H.,
Coronavirus Disease 2019: Coronaviruses and Kidney Injury. The Journal of Urology.
2020;
204
(5)
:
918-25
.
View Article PubMed Google Scholar -
Jeyalan
V.,
Storrar
J.,
Wu
H.H.,
Ponnusamy
A.,
Sinha
S.,
Kalra
P.A.,
Native and transplant kidney histopathological manifestations in association with COVID-19 infection: A systematic review. World Journal of Transplantation.
2021;
11
(11)
:
480-502
.
View Article PubMed Google Scholar -
Abdul-Rasool
S.,
Fielding
B.C.,
Understanding Human Coronavirus HCoV-NL63. The Open Virology Journal.
2010;
4
(1)
:
76-84
.
View Article PubMed Google Scholar -
Moorani
K.N.,
Aziz
M.,
Amanullah
F.,
Rapidly progressive glomerulonephritis in children. Pakistan Journal of Medical Sciences.
2022;
38
(2)
:
417-25
.
View Article PubMed Google Scholar -
Lednicky
J.A.,
Waltzek
T.B.,
McGeehan
E.,
Loeb
J.C.,
Hamilton
S.B.,
Luetke
M.C.,
Isolation and genetic characterization of human coronavirus NL63 in primary human renal proximal tubular epithelial cells obtained from a commercial supplier, and confirmation of its replication in two different types of human primary kidney cells. Virology Journal.
2013;
10
(1)
:
213
.
View Article PubMed Google Scholar -
Castillo
G.,
Mora-Díaz
J.C.,
Breuer
M.,
Singh
P.,
Nelli
R.K.,
Giménez-Lirola
L.G.,
Molecular mechanisms of human coronavirus NL63 infection and replication. Virus Research.
2023;
327
:
199078
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 7 (2024)
Page No.: 6568-6572
Published on: 2024-07-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 1989 times
- PDF downloaded - 815 times
- XML downloaded - 76 times
 Biomedpress
Biomedpress


