Abstract
Introduction: Cervical cancer, predominantly associated with high-risk Human Papillomavirus (HPV) types 16 and 18, presents a substantial public health challenge, particularly impacting women in low and middle-income countries. This study aims to address a vital knowledge gap by examining the relationship between age, menstrual status, and histopathological types of cervical carcinoma in Vietnamese patients.
Methods: The research was conducted at a major provincial public maternity and pediatric hospital in Vietnam from August 2019 to July 2022. A total of 48 adult female patients with histopathologically confirmed invasive cervical carcinoma were included in this combined retrospective and prospective observational study. Demographic and clinical data were collected and analyzed using univariate analysis to determine the associations between different factors and histopathological types. Statistical significance was set at p < 0.05, with odds ratios (ORs), 95% confidence intervals (CIs), and p-values calculated accordingly.
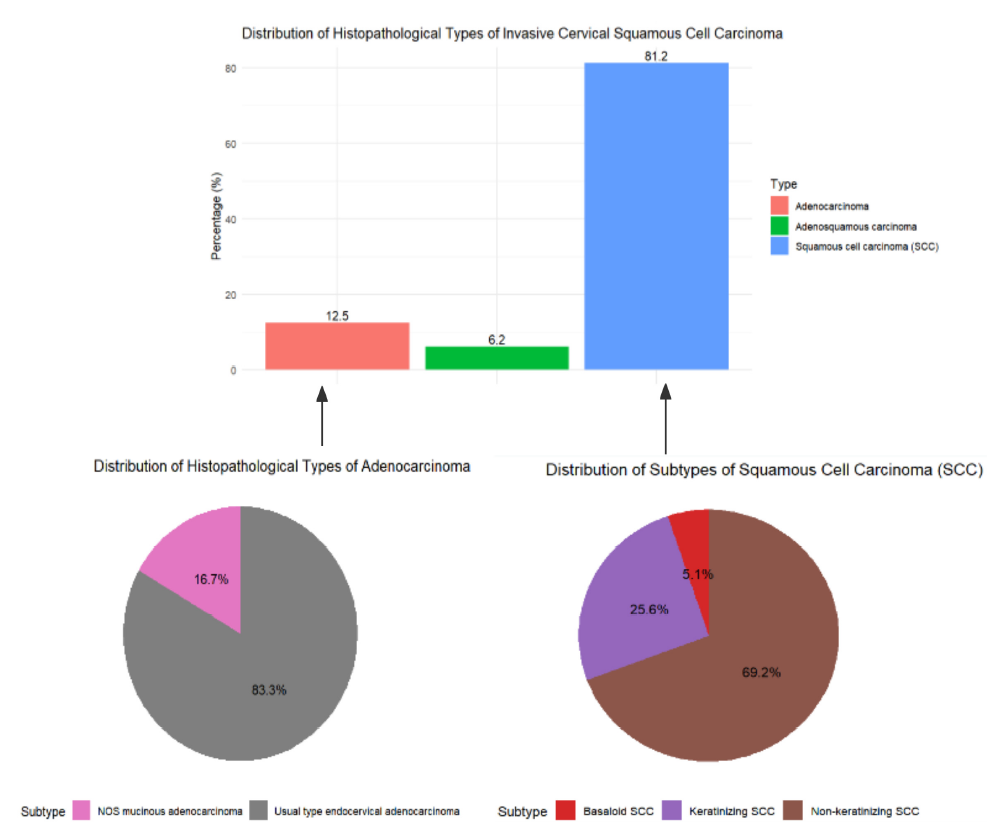
Results: The results revealed that squamous cell carcinoma (SCC) was the most common histopathological type (81.2%), followed by adenocarcinoma (12.5%) and adenosquamous carcinoma (6.2%). Within the SCC subtype, non-keratinizing SCC was the most prevalent (69.2%). Individuals aged 50 years and older had significantly higher odds of being diagnosed with SCC compared to those aged 39 years or younger (OR = 10.40, 95% CI: 1.48-73.00, p = 0.02). Menopausal individuals also had significantly increased odds of SCC compared to those who were menstruating (OR = 10.35, 95% CI: 1.18-90.95, p = 0.04).
Conclusion: These findings underscore the significant correlations between age, menstrual status, and the prevalence of SCC in Vietnamese patients, underscoring the importance of targeted public health initiatives. The study provides crucial insights that could inform the development of effective prevention and management strategies in Vietnam and similar settings.
Introduction
Cervical cancer, primarily caused by high-risk Human Papillomavirus (HPV) types 16 and 18, continues to pose a significant public health challenge globally, particularly in low and middle-income countries. It is ranked as the fourth most common cancer among women, with approximately 530,000 new cases and 275,000 deaths reported annually, highlighting the urgency for extensive research to unravel its epidemiology and risk factors1, 2, 3, 4.
The incidence of squamous cell carcinoma (SCC) globally tends to increase with age, peaking around 55 years before declining, whereas adenocarcinoma (AC) rises until age 45 and then stabilizes. Regional variations in incidence rates exist; for instance, SCC in Eastern Asia, Central and Eastern Europe, and North America follows an inverted U-shaped pattern, contrasting with the continuous increase seen in the Caribbean, Central America, and South-Eastern Asia. These regional disparities underline the necessity for localized research efforts to address specific gaps in data and customize effective public health strategies3.
In Viet Nam, more than 39 million women aged 15 and above face the risk of cervical cancer, making it the sixth most prevalent cancer among Vietnamese women. The country grapples with a high burden of HPV, with significant prevalence rates observed across various cervical conditions: 82.8% in cervical cancer cases, 21.2% in low-grade lesions, and 37.4% in high-grade lesions5. Annually, 4,132 new cases and 2,223 deaths are reported, with projections indicating a potential 200,000 deaths among Vietnamese women by 20706. Despite these alarming statistics, vaccination and screening rates remain low, with only 12% of young women and 28% of those aged 30-49 receiving screenings as of 20215, 6.
Early detection through screening is crucial for improving survival rates, yet many Vietnamese cancer patients receive diagnoses at advanced stages. A National Cancer Control Programme carried out screenings for cervical and breast cancer on 100,000 women between 2008 and 2015, facing constraints due to limited resources and inadequate follow-up. Additionally, the shortage of skilled pathologists and advanced diagnostic facilities in many provincial hospitals exacerbates delays and potential misdiagnoses in cancer treatment7, 8.
Despite the high prevalence of cervical cancer in Viet Nam, comprehensive data elucidating correlations between age, menstrual status, and histopathological types within the country remains scarce. This knowledge gap underscores the significance of our study, which is the first to delve into these relationships among Vietnamese patients by analyzing data from a prominent provincial public maternity and pediatric hospital in Vietnam.
Our research aims to uncover the distinctive epidemiological patterns of cervical cancer in this population to enhance understanding of its etiology and guide the development of tailored public health interventions. By delving into these specific factors, our study contributes vital insights necessary for enhancing cancer care and prevention strategies in Vietnam and other comparable socio-economic settings.
Methods
Study Design and Participants
This study was conducted at the Nghe An Maternity and Pediatric Hospital, utilizing a combined retrospective and prospective observational design to evaluate patients diagnosed with cervical carcinoma between August 2019 and July 2022.
Study Design Overview
We implemented a mixed-methods approach, incorporating both retrospective analysis of existing medical records and histopathological samples, alongside prospective data collection during the study period. This dual approach was designed to minimize selection bias and ensure a comprehensive analysis of the data available, covering a wide range of patient demographics and clinical outcomes.
Participants
Participants included adult female patients aged 18 years or older with a histopathologically confirmed primary diagnosis of invasive cervical carcinoma. Patients with recurrent cervical carcinoma, inadequate biopsy samples, cervical cancers secondary to other primary tumors, or non-squamous histopathological types were excluded from the study. A total of 48 patients met these inclusion criteria, forming a robust dataset for subsequent analysis.
Data Collection
Systematic data collection was employed, gathering detailed clinical and demographic information from patient records. Collected data included age, occupation, residential status, obstetric history, menstrual status, history of abortion, and specific histopathological diagnoses. Data integrity was ensured by aligning classifications with the WHO Classification of Tumors of Female Reproductive Organs, 2014 edition4.
Research Procedure
Retrospective Phase (Before February 2022): For existing cases before February 2022, we retrieved and reviewed original histopathological slides and paraffin blocks using patient and specimen codes. Clinical information was extracted from medical records, and slides were assessed following the WHO 2014 histopathological classification. If necessary, slides with poor quality were re-sectioned and re-stained with Hematoxylin and Eosin (H&E) for accurate evaluation4.
Prospective Phase (From February 2022 Onwards): For new cases from February 2022, clinical data and specimens were collected contemporaneously. These specimens were processed and slides were prepared according to standard histopathological procedures, subsequently reviewed to establish diagnoses based on the WHO 2014 guidelines4.
Histopathological Analysis
Histopathological specimens underwent a thorough review by two experienced pathologists who were blinded to the clinical data. Blinding was achieved by coding the specimens with unique identifiers, which concealed any clinical information. This process adhered to the Standard Operating Procedures (SOP) of Nghe An Maternity and Pediatric Hospital, ensuring that all histopathological reviews were conducted independently and without prior knowledge of the clinical context. Standard histological techniques were employed, including staining with Hematoxylin and Eosin, and examination using the Olympus BX43 microscope. All 48 patients' samples underwent histopathological analysis to ensure comprehensive assessment. Any discrepancies in diagnosis were resolved through consensus or consultation with a third pathologist. Quality control measures, including the use of structured data collection forms and strict adherence to the WHO histopathological classification, were implemented to minimize potential errors and ensure the reliability of findings4, 9.
Sample Processing and Histopathological Examination
Tissue specimens were fixed in 10% formalin, processed using a Thermo Scientific STP 120-2 tissue processor, and embedded in paraffin. Sections of 3 μm thickness were cut using a Thermo Scientific HM 325 microtome and stained with Hematoxylin and Eosin. Histopathological examination was consistent with the WHO 2014 classification guidelines4.
Statistical Analysis
Data analysis was performed using Stata version 17 (Stata Corp, College Station, TX, USA). Demographic and clinical characteristics were summarized using descriptive statistics. Associations between various factors (age, occupation, residential status, menstrual status, number of childbirths, and history of abortion) and histopathological types of cervical carcinoma were assessed using univariate analysis. Odds ratios (OR) and 95% confidence intervals (CI) were calculated to quantify the strength of these associations. The Chi-square test or Fisher's Exact test was used to determine statistical significance, with a p-value of less than 0.05 considered statistically significant. This robust statistical approach ensured the reliability and validity of the study findings.
Ethical Considerations
The study was conducted in compliance with the Declaration of Helsinki, ensuring ethical standards were met throughout the research process. All participant information was handled with strict confidentiality, and informed consent was obtained from all patients where applicable. The research protocol was reviewed and approved by the Ethical Review Board of Nghe An Maternity and Pediatric Hospital. The approval code is 16/QĐ-BVSN, and the date of approval is 14/01/2022.
| Characteristics | Squamous Cell Carcinoma (SCC), n (%) | Adenocarcinoma, n (%) | Adenosquamous carcinoma, n (%) | Total |
|---|---|---|---|---|
| Age group | ||||
| ≤ 29 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) |
| 30-39 | 4 (50.0) | 3 (37.5) | 1 (12.5) | 8 (100.0) |
| 40-49 | 8 (72.7) | 2 (18.2) | 1 (9.1) | 11(100.0) |
| 50-59 | 11 (91.7) | 0 (0.0) | 1 (8.3) | 12 (100.0) |
| ≥ 60 | 15 (93.8) | 1 (6.3) | 0 (0.0) | 16 (100.0) |
| Number of childbirths | ||||
| 1 | 2 (66.7) | 0 (0.0) | 1 (33.3) | 3 (100.0) |
| 2 | 9 (69.2) | 3 (23.1) | 1 (7.7) | 13 (100.0) |
| 3 | 12 (80.0) | 2 (13.3) | 1 (6.7) | 15 (100.0) |
| 4 | 5 (83.3) | 1 (16.7) | 0 (0.0) | 6 (100.0) |
| 5 | 4 (100.0) | 0 (0.0) | 0 (0.0) | 4 (100.0) |
| 6 | 5 (100.0) | 0 (0.0) | 0 (0.0) | 5 (100.0) |
| 7 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) |
| 8 | 1 (100.0) | 0 (0.0) | 0 (0.0) | 1 (100.0) |
| Place of residence | ||||
| Rural | 33 (80.5) | 6 (14.6) | 2 (4.9) | 41 (100.0) |
| Urban | 6 (85.7) | 0 (0.0) | 1 (14.3) | 7 (100.0) |
| Occupation | ||||
| Farming | 28 (84.9) | 4 (12.1) | 1 (3.0) | 33 (100.0) |
| Administrative | 0 (0.0) | 1 (50.0) | 1 (50.0) | 2 (100.0) |
| Commerce | 5 (100.0) | 0 (0.0) | 0 (0.0) | 5 (100.0) |
| Worker | 0 (0.0) | 1 (50.0) | 1 (50.0) | 2 (100.0) |
| Retire | 6 (100.0) | 0 (0.0) | 0 (0.0) | 6 (100.0) |
| Menstrual status | ||||
| Menopause | 22 (95.7) | 1 (4.4) | 0 (0.0) | 23 (100.0) |
| Menstruating | 17 (68.0) | 5 (20.0) | 3 (12.0) | 25 (100.0) |
| History of Abortion | ||||
| No | 26 (76.5) | 6 (17.7) | 2 (5.9) | 34 (100.0) |
| Yes | 13 (92.9) | 0 (0.0) | 1 (7.1) | 14 (100.0) |
| Total | 39 (81.3) | 6 (12.5) | 3 (6.3) | 48 (100.0) |
| Factors | SCC (n, %) | Non-SCC (n, %) | OR (95%CI) | p |
| Age | ||||
| ≤ 39 years | 5 (55.6) | 4 (44.4) | 1 | |
| 40-49 years | 8 (72.7) | 3 (27.3) | 2.13 (0.33-13.81) | 0.43 |
| ≥ 50 years | 26 (92.9) | 2 (7.1) | 10.40 (1.48-73.00) | 0.02 |
| Number of childbirths | ||||
| 1-2 children | 11 (68.8) | 5 (31.3) | 1 | |
| ≥3 children | 28 (87.5) | 4 (12.5) | 3.18 (0.72-14.09) | 0.13 |
| Place of residence | ||||
| Rural | 33 (80.5) | 8 (19.5) | 1 | |
| Urban | 6 (85.7) | 1 (14.3) | 1.45 (0.15-13.85) | 0.75 |
| Occupation | ||||
| Others | 11 (73.3) | 4 (26.7) | 1 | |
| Farming | 28 (84.9) | 5 (15.2) | 2.04 (0.46-9.02) | 0.35 |
| Menstrual status | ||||
| Menstruating | 17 (68.0) | 8 (32.0) | 1 | |
| Menopause | 22 (95.7) | 1 (4.4) | 10.35 (1.18-90.95) | 0.04 |
| History of abortion | ||||
| No | 26 (76.5) | 8 (23.5) | 1 | |
| Yes | 13 (92.9) | 1 (7.1) | 4.00 (0.45-35.49) | 0.21 |
| Note : SCC : squamous cell carcinoma | ||||
Results
Characteristics of Participants
The comprehensive analysis of 48 cases of invasive cervical carcinoma provided detailed insights into the demographic distribution and histopathological characteristics of our study cohort. Squamous cell carcinoma (SCC) was the most prevalent histopathological type, accounting for 81.2% of all cases. This was followed by adenocarcinoma and adenosquamous carcinoma. The non-keratinizing variant of SCC was identified as the most common subtype (Table 1 and Figure 1).
The age distribution of the participants showed that those aged 60 and above comprised 33.3% of the cases. This was followed by the age groups 50 – 59 and 40 – 49. The youngest age group (≤ 29 years) represented 2.1% of the cases. The median age of diagnosis was 53.5 years (Table 1).
A majority of the participants (68.8%) were engaged in farming, and 85.4% resided in rural areas. Regarding reproductive history, all participants had experienced childbirth, and 66.7% reported having three or more children (Table 1). The study patients were almost evenly divided between menstruating (52.1%) and menopausal (47.9%) patients at the time of diagnosis (Table 1).
Distribution of Histopathological Types
The distribution of histopathological types and subtypes of invasive cervical carcinoma among the study participants is illustrated in Table 1. The bar chart at the top of the figure shows the percentage distribution of the primary histopathological types: 81.2% of cases were squamous cell carcinoma (SCC), 12.5% were adenocarcinoma, and 6.2% were adenosquamous carcinoma.The pie charts at the bottom of the figure provide a detailed breakdown of the subtypes within SCC and adenocarcinoma. For SCC, the most common subtype was non-keratinizing SCC, accounting for 69.2% of SCC cases, followed by keratinizing SCC at 25.6%, and basaloid SCC at 5.1%. For adenocarcinoma, the usual type endocervical adenocarcinoma constituted 83.3% of the cases, with mucinous adenocarcinoma, not otherwise specified (NOS), making up 16.7%.
Microscopic Histopathology Identification of Cervical Cancer Tissues
In non-keratinizing squamous cell carcinoma (Figure 2A), the notable absence of keratin pearl formation highlights the undifferentiated state of the tumor cells, which are characterized by pleomorphic nuclei and abundant cytoplasm. This suggests a more aggressive growth pattern compared to keratinizing squamous cell carcinoma (Figure 2B), where the presence of keratin pearls within the tumor cells indicates a higher degree of differentiation and possibly a different trajectory in tumor progression and response to therapy.
Additional complexity is observed in basaloid squamous cell carcinoma (Figure 2C), marked by high-grade tumor cells with hyperchromatic nuclei and minimal cytoplasm, often correlating with a poor prognosis. In contrast, the usual type of endocervical adenocarcinoma (Figure 2D) features glandular structures lined with mucinous cells, reflecting its origin and showing various degrees of cellular atypia. Mucinous adenocarcinoma, not otherwise specified (NOS) (Figure 2E), is characterized by the production of abundant mucin, embedding glandular structures and distinguishing it from other adenocarcinomas. Adenosquamous carcinoma (Figure 2F) exhibits mixed glandular and squamous differentiation, underscoring the histological diversity that can challenge diagnosis and treatment decisions. Lastly, glassy cell carcinoma (Figure 2G), a rare and aggressive subtype, is noted for its large cells with ground-glass cytoplasm and distinct cell borders, posing significant diagnostic and therapeutic challenges.
Factors Associated with Histopathological Types
The univariate analysis was performed to examine the factors associated with the presence of SCC (Table 2). A noteworthy finding emerged regarding age, where individuals aged ≥ 50 years displayed a markedly increased likelihood (OR = 10.40, 95% CI: 1.48 – 73.00, p = 0.02) of SCC diagnosis compared to the reference group of those under 39 years. Although not statistically significant, individuals aged 40-49 years also showed higher odds (OR = 2.13, 95% CI: 0.33-13.81, p = 0.43) of being diagnosed with SCC compared to the reference group.A significant correlation was observed between menstrual status and the incidence of SCC. Menopausal individuals had increased odds (OR = 10.35, 95% CI: 1.18-90.95, p = 0.04) of being diagnosed with SCC relative to the menstruating reference group.
Other factors, including the number of childbirths, place of residence, occupation, and history of abortion, did not demonstrate statistically significant associations with the prevalence of SCC in the univariate analysis. The odds ratios for these factors, in descending order, were: history of abortion (OR = 4.00), number of childbirths (OR = 3.18), occupation (OR = 2.04), and place of residence (OR = 1.45).
Discussion
Associations Between Age, Menstrual Status, and Histopathological Subtypes
This study highlights key relationships between age, menstrual status, and the histopathological subtypes of cervical carcinoma in the Vietnamese population, emphasizing a strong link between older age, menopausal status, and the predominance of squamous cell carcinoma (SCC). This insight is critical for developing targeted public health strategies and improving early detection methods. Our results align with global trends showing SCC as the most common subtype (81.2%), followed by adenocarcinoma (12.5%), mirroring global percentages3. High SCC rates in Sub-Saharan Africa and AC rates in South-East Asia call for tailored prevention measures, including improved HPV testing and specific screening protocols3. Further, our findings indicate that women over 50 have significantly higher SCC odds compared to younger women, with menopausal status further increasing susceptibility3, 10, 11, 12. These hormonal and immunological shifts highlight the necessity for age-adapted screening programs. Additionally, evidence from the EPIC cohort study suggests that menopausal hormone therapy may lower invasive cervical cancer risk, and recent reviews propose that hormone replacement therapy (HRT) could benefit cervical adenocarcinoma survivors, indicating potential therapeutic avenues for post-menopausal management11, 12.
Prognostic Implications of Histopathological Subtypes in Cervical Carcinoma
Recognizing the distinct characteristics of cervical carcinoma subtypes—squamous cell carcinoma (SCC) and adenocarcinoma (AC)—is essential for effective prognosis and treatment. Both subtypes are primarily caused by HPV, with HPV 18 more frequently associated with AC, particularly in younger women3. Risk factors vary, with cigarette smoking linked to SCC but not AC. Detection methods also differ: Pap smears effectively identify SCC but are less reliable for detecting AC, which often occurs in the upper endocervical canal. In contrast, HPV DNA testing improves AC detection3. Prognostically, AC typically shows worse outcomes compared to SCC, as indicated by lower survival rates for AC patients following treatments like radiotherapy or chemoradiotherapy3. Epidemiological data from the U.S. Cancer Statistics Incidence Analytic Database (1999–2015) reveal diverging trends between these subtypes, with SCC rates decreasing in most racial/ethnic groups, while AC rates have been rising among non-Hispanic whites aged 40–5913. This underscores the necessity for demographic-specific prevention efforts. Moreover, despite having the lowest incidence rates, Black women exhibit the highest mortality and the lowest 5-year relative survival rates for AC, emphasizing the critical need for equitable healthcare access to improve outcomes for all demographic groups14.
Demographic Specificity and Reproductive History in Cervical Cancer Incidence
Our study highlights the heightened incidence of cervical cancer among post-menopausal women and rural-based farmers, suggesting that environmental, lifestyle, and occupational factors play significant roles in cancer risk. International reviews, including those by the Asian National Cancer Centers Alliance (ANCCA), emphasize the impact of high-risk HPV in rural areas, compounded by poor access to health services and limited health professional availability15, 16. These factors necessitate tailored public health measures, such as better education and enhanced HPV vaccination access. Furthermore, our findings confirm the significant influence of reproductive history on cervical cancer risk. Increased parity and abortions are linked to higher HPV infection rates and cervical cancer, possibly due to extended hormonal exposure and cervical trauma17. Comparative studies demonstrate variability in the impact of abortion history on HPV prevalence, contrasting our findings of 29.17% in Vietnamese women (14/48) with 83.33% in Ethiopian HPV-positive women17. Additionally, research from the China Kadoorie Biobank indicates that rural residents with a history of pregnancy loss face a 38% increased risk of cervical cancer18. However, a Taiwanese study observed no significant risk difference related to abortions, suggesting that different types of pregnancy loss might impact cancer risk differently19. These observations underline the necessity of incorporating reproductive history into risk assessments and public health strategies to address cervical cancer effectively.
Personalized Strategies and Study Limitations
Our identification of diverse histopathological subtypes of cervical cancer, such as basaloid squamous cell carcinoma and usual type endocervical adenocarcinoma, underscores the need for personalized diagnostic and treatment approaches20, 21. Recent advancements in molecular pathology have facilitated the development of targeted therapies and precision medicine approaches in treating cervical cancer, highlighting the potential benefits of subtype-specific treatments22, 23. Despite these insights, our study acknowledges limitations, including a small sample size that impacts statistical power and generalizability. Future studies should aim for larger cohorts to validate these findings across diverse populations. Moreover, comprehensive demographic information, including socioeconomic status and detailed lifestyle factors, would provide a more nuanced understanding of risk factors and guide more effective prevention strategies.
Conclusions
This study reveals a strong link between age, menopausal status, and the incidence of squamous cell carcinoma (SCC) among Vietnamese patients. Specifically, those who are 50 years or older and women who have gone through menopause are at a significantly higher risk of developing SCC. These findings highlight the critical role that hormonal changes play in the development of cervical cancer, indicating that an individual's menstrual history is crucial in framing both screening and treatment approaches.
Given these results, there is an urgent need for more targeted public health initiatives and further research into the hormonal and reproductive elements that contribute to cervical cancer. Our study's insights are invaluable for crafting more effective prevention and management tactics, benefiting not just Vietnam but also other regions with similar socio-economic profiles.
Abbreviations
AC - Adenocarcinoma, ANCCA - Asian National Cancer Centers Alliance, CIs - Confidence Intervals, DNA - Deoxyribonucleic Acid, EPIC - European Prospective Investigation into Cancer and Nutrition, H&E - Hematoxylin and Eosin, HPV - Human Papillomavirus, HRT - Hormone Replacement Therapy, NOS - Not Otherwise Specified, OR - Odds Ratios, SCC - Squamous Cell Carcinoma, SOP - Standard Operating Procedures, U.S. - United States
Acknowledgments
The authors would like to thank all the patients who participated in the study.
Author’s contributions
HP, VP and HT conceptualized and designed the study. VP, CB, TN, and TT collected and summarized data. HL, VP, and HT were involved in the data interpretation. HP, VP made the first draft of the paper. All authors contributed significantly to the revision of the manuscript. All authors confirm they read and approved the final version.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Bosch
F.X.,
Lorincz
A.,
Muñoz
N.,
Meijer
C.J.,
Shah
K.V.,
The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology.
2002;
55
(4)
:
244-65
.
View Article PubMed Google Scholar -
Smith
J.S.,
Lindsay
L.,
Hoots
B.,
Keys
J.,
Franceschi
S.,
Winer
R.,
Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. International Journal of Cancer.
2007;
121
(3)
:
621-32
.
View Article PubMed Google Scholar -
Wang
M.,
Huang
K.,
Wong
M.C.,
Huang
J.,
Jin
Y.,
Zheng
Z.J.,
Global Cervical Cancer Incidence by Histological Subtype and Implications for Screening Methods. Journal of Epidemiology and Global Health.
2024;
14
(1)
:
94-101
.
View Article PubMed Google Scholar -
Kurman
R.J.,
Carcangiu
M.L.,
Herrington
C.S.,
Young
R.H.,
WHO classification of tumours of female reproductive organs. Monodermal teratomas and somatic-type tumours arising from a dermoid cyst.
2014;
2014
:
63-6
.
-
HPV Information Centre : Bruni L AG, Serrano B, Mena M, Collado JJ, Gómez D, Muñoz J, Bosch FX, de Sanjosé S. ICO/IARC Information Centre on HPV and Cancer Human Papillomavirus and Related Diseases in Viet Nam. 2023. Accessed 11 Jan 2024. https://hpvcentre.net/statistics/reports/VNM.pdf.
.
-
NIHE UV. An investment case study on HPV vaccination in Vietnam 2023. Accessed 11 Jan 2024. https://vietnam.unfpa.org/sites/default/files/pub-pdf/eng_final_pdf_0.pdf.
.
-
Thuan
T.V.,
Tu
D.V.,
Huong
T.T.T.,
Cancer control in Vietnam: Where are we now? . Updated 21 December 2017. https://www.cancercontrol.info/wp-content/uploads/2017/12/99-104-Thaun.pdf.
.
-
Pham
T.,
Bui
L.,
Kim
G.,
Hoang
D.,
Tran
T.,
Hoang
M.,
Cancers in Vietnam-Burden and Control Efforts: A Narrative Scoping Review. Cancer Control.
2019;
26
(1)
:
1073274819863802
.
View Article PubMed Google Scholar -
Elston
C.W.,
Ellis
I.O.,
Pathological prognostic factors in breast cancer. I. The value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology.
1991;
19
(5)
:
403-10
.
View Article PubMed Google Scholar -
Suresh
R.,
Twigg
A.,
Murase
J.E.,
The relationship between menopausal hormone therapy and keratinocyte carcinoma: A review. International Journal of Women's Dermatology.
2018;
5
(1)
:
8-13
.
View Article PubMed Google Scholar -
Roura
E.,
Travier
N.,
Waterboer
T.,
Sanjosé
S. de,
Bosch
F.X.,
Pawlita
M.,
The Influence of Hormonal Factors on the Risk of Developing Cervical Cancer and Pre-Cancer: results from the EPIC Cohort. PLoS One.
2016;
11
(1)
:
e0147029
.
View Article PubMed Google Scholar -
Villa
P.,
Bounous
V.E.,
Amar
I.D.,
Bernardini
F.,
Giorgi
M.,
Attianese
D.,
Hormone Replacement Therapy in Post-Menopause Hormone-Dependent Gynecological Cancer Patients: A Narrative Review. Journal of Clinical Medicine.
2024;
13
(5)
:
1443
.
View Article PubMed Google Scholar -
Islami
F.,
Fedewa
S.A.,
Jemal
A.,
Trends in cervical cancer incidence rates by age, race/ethnicity, histological subtype, and stage at diagnosis in the United States. Preventive Medicine.
2019;
123
:
316-323
.
View Article Google Scholar -
Cohen
C.M.,
Wentzensen
N.,
Castle
P.E.,
Schiffman
M.,
Zuna
R.,
Arend
R.C.,
Racial and Ethnic Disparities in Cervical Cancer Incidence, Survival, and Mortality by Histologic Subtype. Journal of Clinical Oncology.
2023;
41
(5)
:
1059-68
.
View Article PubMed Google Scholar -
Zhetpisbayeva
I. K.F.,
Sarmuldayeva
Sh,
Semenova
Y.,
Glushkova
N.,
Cervical Cancer Prevention in Rural Areas. Annals of Global Health.
2023;
89
(75)
:
1-15
.
View Article Google Scholar -
Ong
S.K.,
Abe
S.K.,
Thilagaratnam
S.,
Haruyama
R.,
Pathak
R.,
Jayasekara
H.,
Towards elimination of cervical cancer - human papillomavirus (HPV) vaccination and cervical cancer screening in Asian National Cancer Centers Alliance (ANCCA) member countries. The Lancet Regional Health. Western Pacific.
2023;
39
:
100860
.
View Article PubMed Google Scholar -
Jensen
K.E.,
Schmiedel
S.,
Norrild
B.,
Frederiksen
K.,
Iftner
T.,
Kjaer
S.K.,
Parity as a cofactor for high-grade cervical disease among women with persistent human papillomavirus infection: a 13-year follow-up. British Journal of Cancer.
2013;
108
(1)
:
234-9
.
View Article PubMed Google Scholar -
Zhan
Y.,
Wang
Y.,
Qu
Y.,
Zhang
L.,
Liu
X.,
Liu
R.,
Jun Lyu
Zhengming Chen Yu Jiang Liming Li China Kadoorie Biobank Collaborative Group,
Pregnancy Loss in Relation to the Risks of Female-Specific Cancers in a Population-Based Cohort and Mendelian Randomization Study - China, 2004-2017. China CDC Weekly.
2023;
5
(19)
:
413-8
.
View Article PubMed Google Scholar -
Shen
C.T.,
Tai
S.Y.,
Tsao
Y.H.,
Chen
F.M.,
Hsieh
H.M.,
Abortion and Female Cancer Risks among Women Aged 20 to 45 Years: A 10-Year Longitudinal Population-Based Cohort Study in Taiwan. International Journal of Environmental Research and Public Health.
2023;
20
(4)
:
3682
.
View Article PubMed Google Scholar -
Shimada
M.,
Tokunaga
H.,
Kigawa
J.,
Yaegashi
N.,
Impact of Histopathological Risk Factors on the Treatment of Stage IB-IIB Uterine Cervical Cancer. The Tohoku Journal of Experimental Medicine.
2020;
252
(4)
:
339-51
.
View Article PubMed Google Scholar -
Hasugian
S.,
Lubis
K.,
Doan
H.,
Profile of histopathology of cervical cancer tissues in patients of the Dr Pirngadi Medan hospital. Journal Biosains.
2020;
6
(3)
:
90
.
View Article Google Scholar -
Campos-Parra
A.D.,
Pérez-Quintanilla
M.,
Martínez-Gutierrez
A.D.,
Pérez-Montiel
D.,
Coronel-Martínez
J.,
Millan-Catalan
O.,
Molecular Differences between Squamous Cell Carcinoma and Adenocarcinoma Cervical Cancer Subtypes: Potential Prognostic Biomarkers. Current Oncology (Toronto, Ont.).
2022;
29
(7)
:
4689-702
.
View Article PubMed Google Scholar -
Van Anh
D.T.,
Thang
V.H.,
Dung
T.A.,
Huyen
T.T.,
Nhan
D.T.,
Van Giang
B.,
Outcome and toxicity of chemoradiation using volumetric modulated arc therapy followed by 3D image-guided brachytherapy for cervical cancer: Vietnam National Cancer Hospital experience. Reports of Practical Oncology and Radiotherapy : Journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology.
2024;
28
(6)
:
784-93
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 6 (2024)
Page No.: 6511-6519
Published on: 2024-06-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 2808 times
- PDF downloaded - 983 times
- XML downloaded - 112 times
 Biomedpress
Biomedpress



