Abstract
Introduction: Acute Obstructive Pyelonephritis (AOP) is a severe and prevalent infection within the urinary system, prone to rapidly escalate into urosepsis and potentially result in septic shock, which poses a significant mortality risk. This study investigates the potential of certain blood parameters to serve as indicators for predicting the likelihood of developing septic shock in AOP patients.
Methods: We conducted a retrospective cohort study involving 60 patients who were diagnosed with AOP as a result of urinary tract stones or benign ureteral strictures, enrolled from August 2023 to February 2024. Key hematological data, including white blood cell count, neutrophil, lymphocyte, and platelet levels, as well as ratios such as neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR), alongside the systemic immune-inflammation index (SII), were extracted from complete blood counts recorded at hospital admission. These parameters were analyzed using univariate and multivariate logistic regression models to assess their predictive value for septic shock.
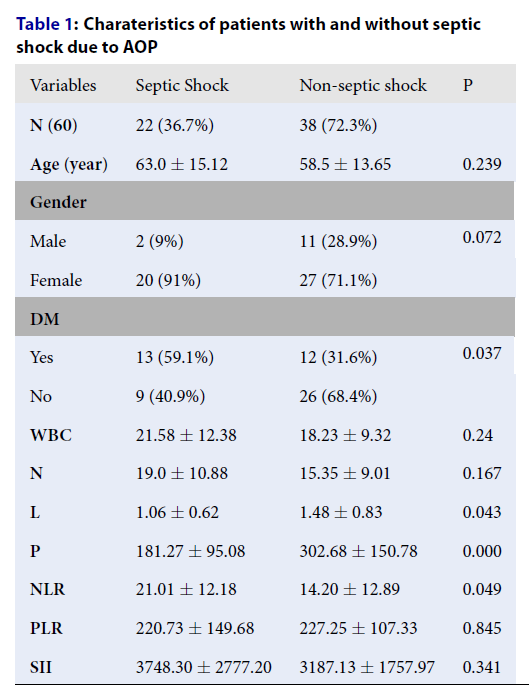
Results: The analysis revealed that 22 out of 60 participants (36.7%) progressed to septic shock following AOP. Notably, the likelihood of septic shock was higher in patients with diabetes mellitus (DM) (p = 0.037), those with diminished lymphocyte (p = 0.043) and platelet counts (p < 0.001), and elevated neutrophil-to-platelet ratio (p = 0.049) when compared to the non-septic shock cohort. Furthermore, multivariate logistic regression identified DM, NLR ≥ 8.7 (OR = 12.529, p = 0.030), and platelet counts below 150 x 109/L (OR = 4.375, p = 0.049) as independent predictors of septic shock.
Conclusion: Elevated NLR, reduced platelet count, and the presence of DM are significant predictors for the development of septic shock in patients afflicted with AOP. These findings suggest that closer monitoring and management of these parameters could be crucial in the early identification and treatment of patients at higher risk of septic shock.
Introduction
Acute pyelonephritis is an inflammatory condition significantly affecting the renal parenchyma, predominantly caused by various pathogens, especially bacteria. When this condition is accompanied by upper urinary tract obstruction, it is known as Acute Obstructive Pyelonephritis (AOP), which may result from urinary stones, ureteral strictures, or external pressures on the urinary tract1. Notably, pyelonephritis is classified as the fifth most common kidney disease, with AOP impacting a significant 84% of individuals suffering from all types of pyelonephritis1. The progression to urosepsis and bacteriotoxic shock in AOP cases is a dangerously high possibility, presenting a mortality risk of 70-90%2. These statistics underscore the need for immediate attention and action, positioning AOP as a predominant concern in urological emergencies.
The Complete Blood Count (CBC) stands as a foundational diagnostic tool in clinical practices. This accessible, economical test provides crucial insights into the blood's fundamental elements—red cells, white cells, and platelets—thereby reflecting the body’s reaction to infection, inflammation, and an array of conditions including cancer. Emerging research has spotlighted a number of pertinent hematological markers such as the Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and the Systemic Immune-Inflammation Index (SII). These indices are gaining recognition for their role in gauging the immune system's response to both infectious and non-infectious factors3, 4, 5. Elevated levels of NLR, PLR, or SII are increasingly associated with less favorable health outcomes, enhancing their utility as diagnostic and prognostic indicators for a wide spectrum of diseases, encompassing cardiovascular disorders, respiratory conditions, rheumatic diseases, and various cancers—gastric, lung, colorectal, and ovarian malignancies, among others, even stretching to urologic ailments3, 4, 5.
This paper aims to assess the prognostic importance of these hematological indices, derived from admission-phase CBC, in forecasting the development of septic shock in AOP patients. Through this lens, we seek to advance our understanding and approach towards effectively managing this critical urological emergency.
Methods
Study Design
We retrospectively analyzed all adult admissions to the Emergency Department and Department of Urology and Renal Transplantation at People’s Hospital 115 who were diagnosed with acute obstructive pyelonephritis by urologists between August 2023 and February 2024. The criteria for acute pyelonephritis included any two of the following criteria1, 2, 6: a) fever (axillary temperature ≥ 38.3°C); b) flank pain or costovertebral angle tenderness; c) preceding symptoms of cystitis (two or more of the following: dysuria, frequency, suprapubic pain, or urgency), along with the presence of pyuria (more than 5 white blood cells (WBCs)/high-power field in a centrifuged sediment), or a positive urine culture (more than 104 colony-forming units per high-power field). Acute obstructive pyelonephritis (AOP) was defined as acute pyelonephritis associated with upper urinary tract obstruction. Upper urinary tract obstruction was determined by acute hydronephrosis on imaging tests, usually such as abdominal ultrasound and contrast or non-contrast computed tomography (CT).
The exclusion criteria were as follows: pregnant women, upper urinary tract obstruction due to malignant factors, patients with a history of hematological disorders like leukemia, myeloproliferative disorders, etc., or those undergoing chemotherapy and radiotherapy, because these patients have more abnormalities in the complete blood count tests that induce bias.
Sepsis and Septic Shock
According to the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3), sepsis is defined as “life-threatening organ dysfunction caused by a dysregulated host response to infection.” An increase of two points or more in the Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score indicates the clinical diagnosis of organ failure. A quickSOFA (qSOFA) score was created for bedside rapid detection, which is based on three criteria: respiratory rate > 22/min, impaired mentation (Glasgow Coma Scale < 15), or systolic blood pressure ≤ 100 mmHg (positive if qSOFA ≥ 2)7.
The definition of septic shock is “a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone”. The clinical diagnosis of septic shock can be identified by the demand for vasopressors to maintain a mean arterial pressure of at least 65 mmHg and a serum lactate level greater than 2 mmol/L (>18 mg/dL) when hypovolemia is absent7.
Data Collection and Statistical Analysis
We divided the patients into two groups: septic shock and non-septic shock groups. Data on age, gender, medical history, and hematological indices derived from admission peripheral blood count, urinalysis, and urine culture were collected and analyzed. The peripheral CBC was performed on a Sysmex XN-2000 machine at People’s Hospital 115. The hematological parameters comprised absolute counts of white blood cells (WBC), neutrophils (N), lymphocytes (L), and platelets (P), and we also calculated the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and systemic immune-inflammation index (SII). The formulas for NLR and PLR were the ratios of the absolute counts of neutrophils and platelets to the absolute counts of lymphocytes, respectively. The formula for SII was (N x P)/L (109/L)3, 4.
We conducted univariate and multivariate statistical analyses using SPSS statistical software version 22 (SPSS Inc., Chicago, USA). We utilized t-tests and Mann-Whitney U tests to assess quantitative variables and Chi-square or Fisher’s exact tests for categorical variables between the septic shock and non-septic shock groups. The multivariate logistic regression was conducted to detect the association between the various potential risk factors mentioned above. Significance was defined as p < 0.05.
| Variables | Septic Shock | Non-septic shock | P |
|---|---|---|---|
| N (60) | 22 (36.7%) | 38 (72.3%) | |
| Age (year) | 63.0 ± 15.12 | 58.5 ± 13.65 | 0.239 |
| Gender | |||
| Male | 2 (9%) | 11 (28.9%) | 0.072 |
| Female | 20 (91%) | 27 (71.1%) | |
| DM | |||
| Yes | 13 (59.1%) | 12 (31.6%) | 0.037 |
| No | 9 (40.9%) | 26 (68.4%) | |
| WBC | 21.58 ± 12.38 | 18.23 ± 9.32 | 0.24 |
| N | 19.0 ± 10.88 | 15.35 ± 9.01 | 0.167 |
| L | 1.06 ± 0.62 | 1.48 ± 0.83 | 0.043 |
| P | 181.27 ± 95.08 | 302.68 ± 150.78 | 0.000 |
| NLR | 21.01 ± 12.18 | 14.20 ± 12.89 | 0.049 |
| PLR | 220.73 ± 149.68 | 227.25 ± 107.33 | 0.845 |
| SII | 3748.30 ± 2777.20 | 3187.13 ± 1757.97 | 0.341 |
| Variables | OR | 95% C.I | p | |
|---|---|---|---|---|
| DM Positive Negative | 4.773 | 1.248 - 18.253 | 0.022 | |
| NLR NLR ≥ 8.7 NLR < 8.7 | 12.529 | 1.272 - 123.426 | 0.030 | |
| Thrombocytopenia Yes No | 4.375 | 1.008 - 18.987 | 0.049 | |
| Lymphopenia Yes No | 2.132 | 0.541 - 8.397 | 0.279 |
Results
Among the 60 patients diagnosed with AOP (Acute obstructive pyelonephritis), 36.7% (22 patients) developed septic shock, a severe complication of AOP. These patients had a median age of 60.13 years, ranging from 21 to 103 years, with a gender distribution of 13 men to 47 women.
In comparing the characteristics of patients with and without septic shock (as shown in Table 1), those in the septic shock group were found to have a higher prevalence of diabetes mellitus (59.1% versus 31.6%, p = 0.037), a lower platelet count (181.27 ± 95.08 vs 302.68 ± 150.78, p < 0.001), a lower lymphocyte count (1.06 ± 0.62 vs 1.48 ± 0.83, p = 0.043), and a higher Neutrophil-to-lymphocyte ratio (NLR) (21.01 ± 12.18 vs 14.20 ± 12.89, p = 0.049). Meanwhile, factors such as age, gender, White Blood Cell (WBC) count, Neutrophil (N) count, Platelet-to-lymphocyte ratio (PLR), and Systemic Immune-Inflammation Index (SII) showed no significant differences between the two groups.
Thresholds for certain laboratory values were defined as thrombocytopenia (platelet count less than 150 x 10⁹/L) and lymphopenia (total lymphocyte count less than 1 x 10⁹/L). An NLR cut-off value was established at 8.7, with the Area Under the Curve (AUC) calculated to be 0.70, demonstrating a sensitivity of 95.5% and specificity of 39.5% (p = 0.012).
Further analysis through Multivariate Logistic Regression (Table 2) revealed that a history of diabetes mellitus, an elevated NLR equal to or greater than 8.7, and thrombocytopenia were independently associated with an increased risk of developing septic shock in the context of AOP. Specifically, patients with diabetes mellitus were around 4.8 times more likely to develop septic shock (OR = 4.773, 95% CI = 1.248-18.253, p = 0.022), those with an NLR ≥ 8.7 were about 12.5 times more likely (OR = 12.529, 95% CI = 1.272-123.426, p = 0.03), and patients with thrombocytopenia were roughly 4.4 times more likely to develop septic shock (OR = 4.375, 95% CI = 1.008-18.987, p = 0.049. Nevertheless, patients with lymphopenia were significantly less likely to progress septic shock due to AOP (OR = 2.132, 95% CI = 0.541-8.397, p = 0.279). These findings emphasize the importance of these factors in assessing the risk and managing patients with AOP to prevent the onset of septic shock.
Discussion
The urinary tract infection is the second or third most common cause of septic shock. It accounted for 6.2% to 38% of patients diagnosed with severe sepsis or septic shock6. Obstructive pyelonephritis is a complicated urinary tract infection requiring medical-surgical emergency intervention due to the possibility of serious consequences like bacteremia or uroseptic shock. Risk factors evaluated to predict the worsening development into septic shock in acute obstructive pyelonephritis (AOP) include diabetes mellitus (DM), procalcitonin, C-reactive protein, age, neutrophil count, serum creatinine level, serum albumin level, and platelet count2, 6, 8, 9.
Additionally, we discovered in this study that septic shock was more common in patients with DM than in those without, with p = 0.037. DM has always been associated with an increased risk of urinary tract infection, mostly due to glycosuria, which is exacerbated by obstruction. Furthermore, DM significantly induces peripheral neuropathy and an immunosuppressive condition, which may attenuate the host defense against urinary pathogens as well as the efficacy of the urinary apparatus’s sensory and voiding functions1.
Upon evaluating hematological indices obtained from the peripheral blood count upon admission, we found a lower lymphocyte count, lower platelet count, and a greater NLR in the septic shock group, compared with the non-septic group. In multivariate logistic regression analysis, only higher NLR and thrombocytopenia were independent factors for uroseptic shock. Numerous investigations demonstrate a substantial correlation between severe sepsis and the reduction in platelets1. Thrombocytopenia is an important criterion of the SOFA score, a useful tool to determine the severity of organ dysfunction in critically ill patients7. Decreased platelet generation, hemodilution, platelet consumption, elevated platelet sequestration in microvessles, and immune-mediated platelet destruction contribute to the declined peripheral platelet count in sepsis. In the severe forms of sepsis, disseminated intravascular coagulation (DIC) is diagnosed by the widespread activation of coagulation inducing thrombotic occlusion in small and mid-sized vessels. The platelets consumption via thrombin-mediated activation in concurrent DIC, triggered by cell-specific membrane components of microorganisms, results in the subsequent depletion of platelets. Furthermore, the activated platelets can encourage the recruitment of neutrophils to the site of injury and promote the formation of neutrophil extracellular traps (NETs) to capture and eliminate pathogens9, 10.Regarding the neutrophil-to-lymphocyte ratio (NLR), Zahorec (2001) first proposed the formula of the ratio between neutrophil and lymphocyte counts, which represents the two arms of the immune system: the innate immune response (neutrophil) and the adaptive immune response (lymphocyte)11. Since then, the Zahorec index, also known as NLR, has been the subject of much research in infectious diseases. It has been proposed as a biomarker for invasive systemic inflammatory responses in oncological diseases and other conditions5. For sepsis and a variety of infection types with different etiologies, NLR is a fairly sensitive but non-specific indication12. According to Zahorec, an adult’s physiological NLR value should normally fall between 1 and 2, with values more than 3 or less than 0.7 suggesting abnormal conditions5. This may be regarded as a novel biomarker within the panel of inflammatory responses like C-reactive protein (CRP), procalcitonin, interleukin-6, lactate, and platelet counts13, 14, 15. Ljungstrom et al. assessed the efficacy of several indicators in a total of 1572 adult patients for identifying bacterial sepsis. The outcomes demonstrated that NLR performed similarly to CRP and PCT. With a threshold of 3 (the upper limit of normal), NLR has a greater sensitivity for sepsis (95%) when compared to other tests. Sepsis is thus ruled out by a normal NLR (< 3). On the other hand, an NLR considerably more than 10 would support a sepsis diagnosis13. De Jager et al. found that lymphocytopenia and NLR outperformed CRP and the total count of white blood cells (WBC) for the diagnosis of bacteremia15. In our study, we found the cutoff for admission NLR was 8.7 with AUC = 0.70 (Sensitivity = 95.5% and Specificity = 39.5, p = 0.012) in diagnosing septic shock due to AOP. In a univariate analysis, there were also more patients with lymphocytopenia in the septic shock group than in the non-septic shock group, while no significant difference in the total white blood cell count and neutrophil count was found. Furthermore, the fluctuation of NLR may be utilized to forecast the severity of septic shock as well as the mortality risk12. A dynamic increase in NLR was associated with late death after five days14. Monitoring of NLR levels is necessary to assess the severity of sepsis, inflammatory response, and mortality risk. Sari et al. reported that non-responders or non-survivors had a very high NLR ≥ 15 on the third day of intensive care unit (ICU) stay, with a mortality odds ratio of 6.9616. Thus far, the three fundamental indicators are considered as the gold standard laboratory tests for monitoring sepsis and septic shock, including C-reactive protein, procalcitonin, and NLR12. Although NLR emerged as a routine, informative, and cost-effective biomarker, it has high sensitivity and low specificity because it can be influenced by various factors like age, race, medicine, diabetes, obesity, mental health, cancer, anemia, and stress5.
In this paper, we acknowledge some limitations, such as the small sample size, assessment only at the time of admission, and not considering the mortality risk of the patients as well as medical intervention.
Conclusions
In conclusion, this study highlights the significance of the neutrophil-to-lymphocyte ratio (NLR) ≥ 8.7, thrombocytopenia, and diabetes mellitus as important predictors for the onset of septic shock in individuals with acute obstructive pyelonephritis (AOP). Our findings reinforce the utility of routine hematological parameters, easily obtainable from complete blood counts at admission, in identifying patients at heightened risk for this serious complication. Given the potential for septic shock to rapidly deteriorate patient outcomes, early recognition of these risk factors permits timely intervention and close monitoring, thereby possibly improving the management and prognosis of AOP. This study underscores the value of integrating simple hematological indices with clinical evaluation to stratify risk and optimize care for patients facing this urological emergency.
Abbreviations
AOP - Acute Obstructive Pyelonephritis, AUC - Area Under the Curve, CBC - Complete Blood Count, C.I - Confidence Interval, CRP - C-reactive Protein, CT - Computed Tomography, DM - Diabetes Mellitus, ICU - Intensive Care Unit, L - Lymphocyte count, N - Neutrophil count, NLR - Neutrophil-to-Lymphocyte Ratio, OR - Odds Ratio, P - Platelet count, PLR - Platelet-to-Lymphocyte Ratio, qSOFA - quick Sequential [Sepsis-related] Organ Failure AssessmentSII - Systemic Immune-Inflammation Index, SOFA - Sequential [Sepsis-related] Organ Failure Assessment, WBC - White Blood Cell count
Acknowledgments
None.
Author’s contributions
Study concept and design: Minh Hoang Truong, Trung Quang Ngo, Phong Thanh Tran; Data acquisition: Trung Quang Ngo, Quang Thanh Nguyen, Phat Thanh To
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study’s procedures involving human subjects were carried out with the approval by the ethical standards of the People’s Hospital 115 ethics committee (1562/BVND115-NCKH). This was a retrospective cohort study, therefore, the informed consent to participate was waived by the Instituition Review Board of People’s Hospital 115.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Abi Tayeh
G.,
Safa
A.,
Sarkis
J.,
Alkassis
M.,
Khalil
N.,
Nemr
E.,
Determinants of pyelonephritis onset in patients with obstructive urolithiasis. Urologia.
2022;
89
(1)
:
100-3
.
View Article PubMed Google Scholar -
Buonaiuto
V.A.,
Marquez
I.,
De Toro
I.,
Joya
C.,
Ruiz-Mesa
J.D.,
Seara
R.,
Clinical and epidemiological features and prognosis of complicated pyelonephritis: a prospective observational single hospital-based study. BMC Infectious Diseases.
2014;
14
(1)
:
639
.
View Article PubMed Google Scholar -
Quang Ngo
T.,
Hoang Truong
M.,
Neutrophil-to-lymphocyte Ratio and Platelet-to-lymphocyte Ratio, Novel Biomarkers and Applications in Urology: an Update. J Regen Biol Med..
2022;
4
:
1-11
.
View Article Google Scholar -
Guo
W.,
Song
Y.,
Sun
Y.,
Du
H.,
Cai
Y.,
You
Q.,
Systemic immune-inflammation index is associated with diabetic kidney disease in Type 2 diabetes mellitus patients: evidence from NHANES 2011-2018. Frontiers in Endocrinology (Lausanne).
2022;
13
.
View Article PubMed Google Scholar -
Zahorec
R.,
Neutrophil-to-lymphocyte ratio, past, present and future perspectives. Bratisl Lek Listy.
2021;
122
(7)
:
474-88
.
View Article PubMed Google Scholar -
Ruiz-Mesa
J.D.,
Marquez-Gomez
I.,
Sena
G.,
Buonaiuto
V.A.,
Mora-Ordoñez
J.,
Salido
M.,
Factors associated with severe sepsis or septic shock in complicated pyelonephritis. Medicine.
2017;
96
(43)
:
e8371
.
View Article PubMed Google Scholar -
Singer
M.,
Deutschman
C.S.,
Seymour
C.W.,
Shankar-Hari
M.,
Annane
D.,
Bauer
M.,
The third international consensus definitions for sepsis and septic shock (Sepsis-3). Journal of the American Medical Association.
2016;
315
(8)
:
801-10
.
View Article PubMed Google Scholar -
Lee
J.H.,
Lee
Y.M.,
Cho
J.H.,
Risk factors of septic shock in bacteremic acute pyelonephritis patients admitted to an ER. Journal of Infection and Chemotherapy.
2012;
18
(1)
:
130-3
.
View Article PubMed Google Scholar -
Tambo
M.,
Okegawa
T.,
Shishido
T.,
Higashihara
E.,
Nutahara
K.,
Predictors of septic shock in obstructive acute pyelonephritis. World Journal of Urology.
2014;
32
(3)
:
803-11
.
View Article PubMed Google Scholar -
Vardon-Bounes
F.,
Ruiz
S.,
Gratacap
M.P.,
Garcia
C.,
Payrastre
B.,
Minville
V.,
Platelets are critical key players in sepsis. International Journal of Molecular Sciences.
2019;
20
(14)
:
3494
.
View Article PubMed Google Scholar -
Zahorec
R.,
Ratio of neutrophil to lymphocyte counts rapid and simple parameter of systemic inflammation and stress in critically ill. Bratislavske lekarske listy.
2001;
102
(1)
:
5-14
.
PubMed Google Scholar -
Firment
J.,
Hulin
I.,
Zahorec index or Neutrophil-to-lymphocyte ratio, valid biomarker of inflammation and immune response to infection, cancer and surgery. Bratislavske Lekarske Listy.
2024;
125
(2)
:
75-83
.
View Article PubMed Google Scholar -
Ljungström
L.,
Pernestig
A.K.,
Jacobsson
G.,
Andersson
R.,
Usener
B.,
Tilevik
D.,
Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One.
2017;
12
(7)
:
e0181704
.
View Article PubMed Google Scholar -
Riché
F.,
Gayat
E.,
Barthélémy
R.,
Le Dorze
M.,
Matéo
J.,
Payen
D.,
Reversal of neutrophil-to-lymphocyte count ratio in early versus late death from septic shock. Critical Care (London, England).
2015;
19
(1)
:
439
.
View Article PubMed Google Scholar -
Jager
C.P. de,
Wijk
P.T. van,
Mathoera
R.B.,
Jongh-Leuvenink
J. de,
Poll
T. van der,
Wever
P.C.,
Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Critical care.
2010;
2010
(14)
:
1-8
.
View Article Google Scholar -
Sar\i
R.,
Karakurt
Z.,
Ay
M.,
Çelik
M.E.,
Yalaz Tekan
Ü.,
Çiyiltepe
F.,
Neutrophil to lymphocyte ratio as a predictor of treatment response and mortality in septic shock patients in the intensive care unit. Turkish Journal of Medical Sciences.
2019;
49
(5)
:
1336-49
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 6 (2024)
Page No.: 6488-6493
Published on: 2024-06-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 2800 times
- PDF downloaded - 985 times
- XML downloaded - 106 times
 Biomedpress
Biomedpress


