Abstract
We report a rare case of portal vein thrombosis (PVT) secondary to idiopathic hypercoagulability leading to non-cirrhotic portal hypertension and cavernous transformation. The patient had a history of acute PVT and superior mesenteric vein thrombosis, which was initially managed successfully with anticoagulation therapy. However, the discontinuation of treatment precipitated a transition to chronic PVT and subsequent cavernous transformation. This condition manifested clinically as esophageal and gastric varices, posing a significant bleeding risk. Attempts to mitigate portal hypertension through medical management and endoscopic interventions had limited success. The anatomical complexities presented an insurmountable challenge to transjugular intrahepatic portosystemic shunt (TIPS) placement, and thus alternative treatment strategies were considered. A splenectomy markedly improved the patient's condition. Over a 2-year follow-up period, with the aid of direct oral anticoagulants (DOACs), the patient remained stable; further endoscopic procedures were not required, and the patient did not experience a recurrence of thromboembolic or hemorrhagic events. This case underscores the complexity of PVT management and highlights the need for individualized treatment approaches in the face of anatomical and therapeutic challenges.
Introduction
Chronic extrahepatic portal vein obstruction is a vascular liver disorder characterized by the blockage and cavernomatous transformation of the portal vein that can affect the intrahepatic portal vein, splenic vein, or superior mesenteric vein. Portal vein thrombosis is an uncommon condition in individuals without liver disease1, 2. The causes can be related to primary and secondary hypercoagulable states. Acute treatment involves anticoagulation and addressing the underlying hypercoagulability3. If portal vein thrombosis progresses to a chronic condition, complications of portal hypertension, including variceal bleeding, can arise. The management of these complications is similar to that of cirrhotic portal hypertension, including pharmacotherapy and endoscopic intervention3. However, endoscopic treatment has various limitations, particularly for gastric varices4. Transjugular intrahepatic portosystemic shunt (TIPS) is a suitable option, but anatomical variations can make it challenging5. We present a case of a patient with non-cirrhotic portal hypertension with chronic portal vein thrombosis treated with splenectomy and long-term anticoagulation, demonstrating the efficacy and safety of the treatment over a 2-year follow-up period.
| Results | Reference range | |
|---|---|---|
| ANA | 0.54 | S/Co < 0.8 |
| Anti ds-DNA | 9.58 | < 25 IU/mL |
| C3 | 114.5 | 80-170 mg/dL |
| C4 | 32.3 | 15-45 mg/dL |
| Lupus anticoagulant screen | Negative | Negative |
| Lupus anticoagulant confirm | 1.11 | 0.80-1.19 IU/mL |
| Anti beta 2 glycoprotein | 2.9 | < 7 IU/mL |
| Anti cardiolipin | 0.72 | < 12 MPL/mL |
| Protein C | 82 | 70-140% |
| Protein | 93 | 55-124% |
| Antithrombin III | 79 | 83-128% |
| Platelet count before splenectomy | 204 | 150-400 G/L |
| Platelet count after splenectomy | 854 |
| Timeline | April 2019 | May 2021 | March 2022 | August 2023 |
|---|---|---|---|---|
| Diagnosis | Acute thromboembolism at portal and superior mesenteric veins | - Total chronic portal vein thrombosis with carvernous transformation - Partial chronic superior mesenteric vein - Severe easophageal and gastric varices | - Total chronic portal vein thrombosis with carvernous transformation - Partial chronic superior mesenteric vein - Easophageal and gastric varices at risk of rupture | - Total chronic portal vein thrombosis with carvernous transformation - Easophageal and gastric varices without rupture risk - Post-splenectomy |
| Treatment | Heparin and VKA | - Carvedilol, ISMN - Prophylatic ligation and slerotherapy via endoscopy - DOACs | - Splenectomy - Carvedilol - DOACs | - Carvedilol - DOACs |
| Notes | Cancelled checkup after 3 months follow-up | Refractory varices despite repetitive endoscopic intervention | - Early resolution of varices - No more endoscopic intervention | 6-month to 1-year endoscopic follow-up |
Clinical Case Information
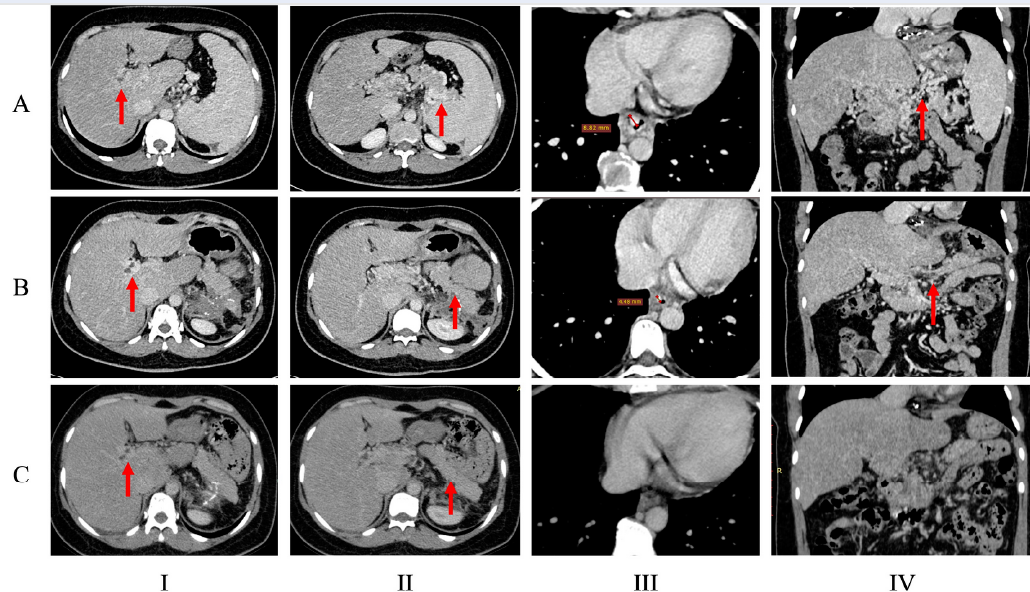
A 46-year-old female patient had a history of acute superior mesenteric and portal vein thrombosis successfully treated with medical therapy at age 44 (i.e., in 2019). During outpatient follow-up, the patient was prescribed long-term vitamin K antagonists (VKAs) for 3–6 months and was scheduled for a re-evaluation of the thrombotic condition and underlying hypercoagulability. However, after 3 months of treatment, the patient, having no symptomatic recurrence, chose to discontinue anticoagulation therapy and did not return for further follow-up until May 2021 when she was admitted to the hospital with epigastric pain. During this hospitalization, the patient underwent gastroduodenal endoscopy, revealing multiple gastric ulcers accompanied by grade III esophageal and gastric varices with red signs (Figure 1 A series). The gastric appearance suggested portal hypertension-related gastropathy, and the ulcers were considered the cause of the gastric pain. A subsequent contrast-enhanced computerized tomography (CT) scan identified chronic thrombosis and cavernomatous transformation of the portal vein extending to intrahepatic distal branches and other splanchnic veins, along with esophageal and gastric varices (Figure 2 A series). Partial thrombosis was noted in the superior mesenteric vein.
The treatment strategy was discussed during the first multidisciplinary consultation, which involved gastroenterologists, cardiologists, radiologists, interventionists, and surgeons. TIPS was deemed unfeasible because of the altered anatomy of the portal and hepatic veins. The medical board opted for the prophylaxis of portal hypertension-related bleeding, including medical management to reduce portal pressure and a combination of endoscopic variceal band ligation and sclerotherapy of gastric varices. The patient was subsequently treated with non-selective beta-blockers, isosorbide mononitrate (ISMN), and gastrointestinal endoscopic intervention. The maximum tolerated doses of carvedilol and ISMN were achieved. Furthermore, the patient received VKAs and was transitioned to DOACs after excluding antiphospholipid syndrome-associated hypercoagulability. The patient was screened for inherited thrombophilia and malignant causes; however, the tests yielded negative results, suggesting idiopathic etiology (Table 1 ).
After 3 months of follow-up, a repeat endoscopy revealed slightly improved esophageal varices but worsening gastric varices, prompting prophylactic intervention. Despite repeated ligation and sclerotherapy, two subsequent 3-month endoscopic assessments did not show adequate improvement. A second multidisciplinary consultation led to the decision for splenectomy after carefully assessing portal venous circulation via CT and preoperative liver function, which was within the normal range. The patient underwent endoscopic splenectomy with low-molecular-weight heparin (LMWH) bridging for anticoagulation. The procedure proceeded smoothly, without bleeding or thromboembolic complications. Postoperatively, the patient was switched to DOACs and discharged after 5 days. Portal pressure-lowering medications were continued. Postoperatively, gastrointestinal endoscopy and CT scans showed significant improvement in esophageal and gastric varices (Figure 1 B series, Figure 2 B series).
The patient was followed for 2 years and remained on medical treatment, including DOACs and carvedilol. Repeated 3-month endoscopic assessments showed sustained improvement and stability characterized by the significant regression of varices, and no high-risk features were observed. Remarkably, the gastric varices almost completely disappeared (Figure 2 C series). A follow-up CT scan after 2 years also indicated drastically improved gastric and esophageal varices. No changes in portal vein morphology were observed, but no mesenteric thrombosis was detected (Figure 2 C series). Notably, the patient did not experience any incidents of thromboembolism or hemorrhaging. The follow-up D-dimer test showed no elevation. The comprehensive diagnostic and treatment details are presented in Table 2.
Discussion
Diagnosis of portal vein thrombosis often relies on Doppler ultrasound or contrast-enhanced CT/magnetic resonance imaging (MRI). Typical imaging features include absent or reduced blood flow into the portal vein, which is replaced by porto-portal collateral vessels in the perihepatic region because of portal venous system shunting; this is referred to as cavernomatous transformation in the absence of recanalization. This transformation may compress the bile duct, leading to biliary stasis. In patients without cirrhosis, liver function is typically normal or mildly impaired, contrasting with the degree of portal hypertension6. Elevated portal venous pressure results in collateral circulation in which gastric varices are mostly seen concomitantly esophageal varices are observed in approximately 40% of the patients in portal vein thrombosis. Portal gastropathy is also a rare feature of this condition7. Chronic portal vein thrombosis might not exhibit prominent clinical symptoms compared with acute cases until complications arise, notably gastrointestinal bleeding from ruptured esophageal or gastric varices6.
In our case, medical treatment of non-cirrhotic portal hypertension included non-selective beta-blockers and ISMN to reduce portal pressure. However, the efficacy of these drugs in patients without cirrhosis is not proven7. Similarly, imaging-guided interventions for portal vein recanalization can be performed but present challenges for interventionists4. Additionally, because of the longer life expectancy of patients without cirrhosis, repeated endoscopic interventions may become a burden. TIPS remains an ideal choice for portal pressure reduction, especially when hepatic encephalopathy is not a concern (e.g., in patients without cirrhosis)3. Technical demands pose significant limitations for TIPS because of altered portal venous anatomy in transposed portal veins, complicating shunt placement5.
The patient was unresponsive to medical treatment, and prophylactic endoscopic intervention and was deemed unsuitable for TIPS. Consequently, we contemplated an unconventional splenectomy approach because of resource limitations precluding liver transplantation. Notably, significant splenic vein drainage into the gastric veins prompted our expectation that reducing this venous flow could substantially ameliorate variceal conditions, leading to improved esophageal variceal control after the splenectomy. Another potential mechanism for post-splenectomy portal pressure reduction was ET-1 and NO reduction8. The risk of perioperative thromboembolism was also considered, and heparin was chosen for bridging to DOACs9, 10. Our expectations were closely aligned with the clinical and subclinical improvements observed in the patient. Of note, the complication of portal cavernoma cholangiopathy did not occur after 2 years of follow-up, suggesting that this is also a benefit of splenectomy.
Indications for splenectomy in non-cirrhotic portal hypertension are not clearly established11. Spleen removal for cirrhotic portal hypertension has been described in several cases; the efficacy of this approach has been reported as a 25% reduction in the hepatic venous pressure gradient and a 21% reduction in portal vascular resistance. Laparoscopic splenectomy is safe in patients with cirrhosis patients and can be extrapolated to be safe in patients with non-cirrhotic portal hypertension with preserved liver function8. Post-splenectomy thrombocytosis and hypercoagulability have an increased risk of vascular incidents that require close observation12, 13.
The treatment of coagulation abnormalities should not be overlooked, as it relates to recanalization within the first 6 months of therapy and the prevention of thrombosis elsewhere in the venous system. This was especially true in this patient, who also had thrombi in the superior mesenteric vein6, 14. In this case, the patient’s refusal of treatment and follow-up, combined with an occluded splenic vein and underlying prothrombotic disorders, may have led to the failure of recanalization during the first admission. Furthermore, long-term concurrent anticoagulation treatment might help recanalize the occluded portions of the portal vein, consequently lowering portal venous pressure, as observed in patients with cirrhosis15. Historically, VKAs have been selected, with a target international normalized ratio (INR) of 2–3. DOACs have recently gained prominence in non-cirrhotic portal vein thrombosis16. They offer the advantage of not requiring monitoring and having fewer drug interactions3. The recent consensus statements recommend DOACs as the primary option in selective cases without anti-phospholipid syndrome since VKAs have more robust recommendations in this group16, 17. Despite the lack of head-to-head comparisons, DOACs show similar PVT recanalization rates to LMWH and VKAs in the early phase, without an increased bleeding risk14.
Conclusions
In summary, this report present the first documented case in Vietnam in which multimodal management was employed. Over 2 years, our patient with chronic portal vein thrombosis and associated portal hypertension-related complications yielded stable and successful outcomes. This case is particularly noteworthy in that it demonstrates the effectiveness of laparoscopic splenectomy in cases where anatomical considerations render other options, such as TIPS placement and liver transplantation, are not viable. Furthermore, it is imperative to emphasize the importance of DOAC therapy in the management of idiopathic hypercoagulability, as it serves as a pivotal preventive measure against thromboembolic events.
Abbreviations
TIPS - Transjugular Intrahepatic Portosystemic Shunt, DOACs - Direct Oral Anticoagulants, VKAs - Vitamin K Antagonists, ISMN: Isosorbide Mononitrate, LMWH: Low Molecular Weight Heparin, CT: Computerized Tomography, INR: International Normalized Ratio, ET-1: Endothelin-1, NO: Nitric Oxide.
Acknowledgments
None.
Author’s contributions
- Tien Manh Huynh: Data curation, Formal analysis, Writing-review & editing and Approval of final manuscript.
- Sang Thanh Nguyen: Data curation, Resources and Approval of final manuscript.
- Ngoc Thanh Lam: Data curation, Formal analysis, Supervision, Visualization and Approval of final manuscript.
- An Le Pham: Supervision and Approval of final manuscript.
- Si Van Nguyen: Conceptualization, Formal analysis, Investigation, Project administration, Visualization, Writing-original draft, Writing-review & editing and Approval of final manuscript.
All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used during the current study are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. The patient gave informed consent, and the patient’s anonymity was preserved.
Consent for publication
Written informed consent for publication was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Okuda
K.,
Ohnishi
K.,
Kimura
K.,
Matsutani
S.,
Sumida
M.,
Goto
N.,
Incidence of portal vein thrombosis in liver cirrhosis. An angiographic study in 708 patients. Gastroenterology.
1985;
89
(2)
:
279-86
.
View Article PubMed Google Scholar -
Bayraktar
Y.,
Balkanci
F.,
Ozenc
A.,
Arslan
S.,
Koseoglu
T.,
Ozdemir
A.,
The" Pseudo--Cholangiocarcinoma Sign" in Patients with Cavernous Transformation of the Portal Vein and Its Effect on the Serum Alkaline Phosphatase and Bilirubin Levels. The American Journal of Gastroenterology.
1995;
90
(11)
:
2015-9
.
PubMed Google Scholar -
Northup
P.G.,
Garcia-Pagan
J.C.,
Garcia-Tsao
G.,
Intagliata
N.M.,
Superina
R.A.,
Roberts
L.N.,
Vascular Liver Disorders, Portal Vein Thrombosis, and Procedural Bleeding in Patients With Liver Disease: 2020 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology (Baltimore, Md.).
2021;
73
(1)
:
366-413
.
View Article PubMed Google Scholar -
Kapoor
A.,
Dharel
N.,
Sanyal
A.J.,
Endoscopic Diagnosis and Therapy in Gastroesophageal Variceal Bleeding. Gastrointestinal Endoscopy Clinics of North America.
2015;
25
(3)
:
491-507
.
View Article PubMed Google Scholar -
Artru
F.,
Vietti-Violi
N.,
Sempoux
C.,
Vieira Barbosa
J.,
Becce
F.,
Sah
N.,
Portal vein recanalisation alone to treat severe portal hypertension in non-cirrhotic patients with chronic extrahepatic portal vein obstruction. JHEP Reports : Innovation in Hepatology.
2022;
4
(8)
.
View Article PubMed Google Scholar -
Gioia
S.,
Nardelli
S.,
Ridola
L.,
Riggio
O.,
Causes and Management of Non-cirrhotic Portal Hypertension. Current Gastroenterology Reports.
2020;
22
(12)
:
56
.
View Article PubMed Google Scholar -
Harmanci
O.,
Bayraktar
Y.,
Portal hypertension due to portal venous thrombosis: etiology, clinical outcomes. World Journal of Gastroenterology.
2007;
13
(18)
:
2535-40
.
View Article PubMed Google Scholar -
Kawanaka
H.,
Akahoshi
T.,
Kinjo
N.,
Iguchi
T.,
Ninomiya
M.,
Yamashita
Y.I.,
Effect of laparoscopic splenectomy on portal haemodynamics in patients with liver cirrhosis and portal hypertension. British Journal of Surgery.
2014;
101
(12)
:
1585-93
.
View Article PubMed Google Scholar -
Li
M.X.,
Zhang
X.F.,
Liu
Z.W.,
Lv
Y.,
Risk factors and clinical characteristics of portal vein thrombosis after splenectomy in patients with liver cirrhosis. Hepatobiliary & Pancreatic Diseases International.
2013;
12
(5)
:
512-9
.
View Article PubMed Google Scholar -
Lee
D.H.,
Barmparas
G.,
Fierro
N.,
Sun
B.J.,
Ashrafian
S.,
Li
T.,
Ley
E.J.,
Splenectomy is associated with a higher risk for venous thromboembolism: A prospective cohort study. International Journal of Surgery.
2015;
24
:
27-32
.
View Article Google Scholar -
Weledji
E.P.,
Benefits and risks of splenectomy. International Journal of Surgery.
2014;
12
(2)
:
113-9
.
View Article PubMed Google Scholar -
Ghaffari
S.,
Pourafkari
L.,
Acute myocardial infarction in a patient with post-splenectomy thrombocytosis: a case report and review of literature. Cardiology Journal.
2010;
17
(1)
:
79-82
.
PubMed Google Scholar -
Kristinsson
S.Y.,
Gridley
G.,
Hoover
R.N.,
Check
D.,
Landgren
O.,
Long-term risks after splenectomy among 8,149 cancer-free American veterans: a cohort study with up to 27 years follow-up. Haematologica.
2014;
99
(2)
:
392-8
.
View Article PubMed Google Scholar -
Elkrief
L.,
Payancé
A.,
Plessier
A.,
d'Alteroche
L.,
Ronot
M.,
Paradis
V.,
Management of splanchnic vein thrombosis. JHEP Reports : Innovation in Hepatology.
2023;
5
(4)
.
View Article PubMed Google Scholar -
Wang
L.,
Guo
X.,
Xu
X.,
De Stefano
V.,
Plessier
A.,
Noronha Ferreira
C.,
Anticoagulation Favors Thrombus Recanalization and Survival in Patients With Liver Cirrhosis and Portal Vein Thrombosis: results of a Meta-Analysis. Advances in Therapy.
2021;
38
(1)
:
495-520
.
View Article PubMed Google Scholar -
Naymagon
L.,
Tremblay
D.,
Zubizarreta
N.,
Moshier
E.,
Troy
K.,
Schiano
T.,
The efficacy and safety of direct oral anticoagulants in noncirrhotic portal vein thrombosis. Blood Advances.
2020;
4
(4)
:
655-66
.
View Article PubMed Google Scholar -
Pastori
D.,
Menichelli
D.,
Cammisotto
V.,
Pignatelli
P.,
Use of Direct Oral Anticoagulants in Patients With Antiphospholipid Syndrome: A Systematic Review and Comparison of the International Guidelines. Frontiers in Cardiovascular Medicine.
2021;
8
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 11 No 2 (2024)
Page No.: 6203-6208
Published on: 2024-02-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 3076 times
- PDF downloaded - 1120 times
- XML downloaded - 101 times
 Biomedpress
Biomedpress



