The markers of platelet functions and Von Willebrand factor serum content from patients with type 2 diabetes mellitus and ishemic stroke
Abstract
Introduction: The estіmated number of people with diabetes worldwide in 2015 is 415 million persons, up to 91% of adults hadtype 2 diabetes and the crude incidence of stroke among patients with diabetes of the 2ndtype can be more than 3 times that in the general population. It is known platelet activation and aggregation are critical in the pathogenesis of acute ischemic cerebrovascular diseases. Thus to examine the evidence of platelet functioning such as platelet count,aggregation in response to ADP, coagulation von Willebrand factor and serotonin content, monoamine oxidase (MAO) activity in the blood of patients with ischemic stroke and with ischemic stroke complicated with the 2ndtype diabetes are the aim of the present study.
Methods: The platelet aggregation was assayed for photo-optical aggregometer, von Willebrand factor was determined by Elisa, serotonin determination included ion-exchange chromatography and fluorescence spectrophotometry. Determination of monoamine-oxidase serum activity was spectophotometry.
Results: The investigation has shown an increase of serotonin and Von Willebrand factor blood content in both groups of patients with ischemic stroke andtype 2 diabetes and stroke alone compared with the values of the control group. The monoamine oxidase activity and platelet count were reduced in blood of patients with diabetes of the 2ndtype with ischemic stroke against to the values from the group of healthy donors. Platelet aggregation in response to ADP increased under the investigated pathologies.
Conclusions: These obtained data suggested a significant imbalance in vascular platelet element of hemostasis under the ischemic stroke and amplification of negative changes under the stroke with the 2ndtype diabetes.
Introduction
According to the International Diabetes Federation data more than 193 million people have undiagnosed diabetes, and the number of estimated cases of this disease in 2015 reached 415 million persons. The most extended form of the diabetes is the type 2 (noninsulin- dependent) form of the disease; occurring in 91% of adults with diabetes in high-income countries Federation, 2015. This is equivalent to about 6% of the world's adult populationTamayo et al., 2014. Persons with diabetes, especially undiagnosed form, who have no corrective treatment, are particularly at high risk group of complications developing. Microvascular damages (retino-, nephro- and neuropathy) are the most frequent pathological manifestations appearing in conditions of hyperglycemia, which primarily defined under diabetes. This damage leads to diminished quality of life, increase morbidity and growth the probability of developing macrovascular disease (stroke, coronary heart disease and peripheral vascular disease), that reduces life expectancy Organization, 2006.
Cerebrovascular disease is the one of the most common reasons for death and disability causes among people with diabetes. In patients suffering cerebrovascular disease, the presence of diabetes of the 2nd type increases the risk of ischemic cerebral infarction, resulting in more than three quarters of all strokes, but at the same time is not associated with an increased risk of cerebral hemorrhage. The incidence of stroke among patients with diabetes of the 2nd type can be 3 times higher, comparing to the general population Davis et al., 1999.
Numerous attempts have been made to identify the elements through which diabetes increases the risk of stroke. The like studies have taken prompts from the cardiovascular literature data where diabetes with the associated components of metabolic syndrome (such as insulin resistance, hyperglycemia, hyperlipidemia and hypertension and obesity,) have been detected as contributing factors to the development of cardiovascular disease. Though the approach has in general been informative, the relationships between diabetes and stroke also involve endothelial dysfunction with hypercoaguability.
However, the platelet function laboratory measurements have established that its reactivity is increased in the acute phase of most strokes Smith et al., 1999 the platelet activation and aggregation are also critical in the pathogenesis of acute ischemic cerebrovascular diseases Fateh-Moghadam et al., 2007. Besides it is known that platelets in patients with the 2nd type of diabetes adhere to vascular endothelium and aggregate more frequently than the ones of healthy people Vinik et al., 2001 so activated platelets release serotonin Hara et al., 2011 and therefore, changes of serotonin levels and enzymes activity responding of serotonin metabolism (i.e. monoamine oxidases) in blood could be a signalling biomarker of the risk of cardioand cerebrovascular occurrences in the future.
But there is no enough evidence about platelet, coagulability parameters and serotonin level under the ischemic stroke in 2 type diabetes patients. Thus to examine the evidence of platelet functioning such as platelet count, aggregation in response to ADP, coagulation von Willebrand factor and serotonin content, monoamine oxidases (MAO) activityin the patients’ blood with ischemic stroke with the 2nd type of diabetes are the primary aim of the given study.
Materials and methods
The experimental group consisted of 65 individuals including 34 persons with type 2 diabetes complicated with ischemic stroke and 31 patients with a stroke alone. The diagnosis of ischemic stroke was confirmed by neurovisualization with computed tomography and magnetic resonance imaging of the brain. The type II diabetes was diagnosed by measurement of serum glucose, glycosylated hemoglobin content and glucose tolerance test. All patients or their relatives had been warned about the clinical research and gave written agreement to participate. The control group consisted of the 20 healthy donors.
The blood for the investigation was withdrawn from an antecubital vein fasting patients from 8 to 9 am into a plastic syringe containing one-tenth volume of 3.8% (0.13 M) trisodium citrate and placed to a tube. The mixture gently stirring and blood plasma was isolated according to the method Tokar AV Makogonenko EM,1994.
The platelet aggregation was assayed for Photo-optical aggregometer AR2110 "Solar" (Belarus). Blood plasma and platelet rich plasma was prepared according to the recommendations of the «Solar» manufacturer. Platelet aggregation was investigated during the first 2 h after blood sampling. The concentration of platelets in the samples was standardized according to the parameters got with the aggregometer. The degree of aggregation was determined as a maximum level of light transmission of blood plasma after application aggregation inducer. Platelet aggregation was induced by ADP solution at a final concentration of 2.5 μM. Working Dilution reagent prepared immediately before the test.
The serotonin serum contents were determined using the ion-exchange chromatography with KM-Sepharose method Maksimenko E., 2000. Measurement of serotonin was performed on Shimadzu fluorescence spectrophotometer at an excitation wavelength of 295 nm and absorption wavelength of 550 nm against samples containing distilled water Weissbach et al., 1958. Determination of monoamineoxidase serum activity was performed by Balakleevskoho and others (A, 1976).
The method principle was the formation of benzaldehyde from benzylamine hydrochloride under the monoamine oxidase action. Benzaldehyde reacts with a 2,3- dinitrophenylhydrazine and formed the insoluble product, which could be precipitated by centrifugation. The precipitate formed the steady crimson colored compound in an alkaline medium, the content of which was determined by spectrophotometer. Von Willebrand factor content in plasma was determined by Elisa.
Statistical analysis was performed using the Statistica statistical analysis software. The Student's parametric criterion was used for assessment of the inter-group differences. The difference between readings was considered as statistically significant at p <0.05.
Results
The investigated parameters were studied among 85 individuals, 34 persons with ischemic stroke complicated with type 2 diabetes, 31 patients with a stroke alone and 20 healthy donors for the control.
Platelet counts measurement showed the overall mean of this parameter for the diabetics with ischemic stroke was 162,3 ± 27,9 *109/L, for ischemic stroke 151,4 ± 33,1*109/L and controls, 205,6 ± 47,6 *109/L ( Figure 1 ). So the studies revealed a downward trend in platelet counts in patients with ischemic stroke complicated with type 2 diabetes on 21% and on 26 % under stroke conditions comparing with the control value.
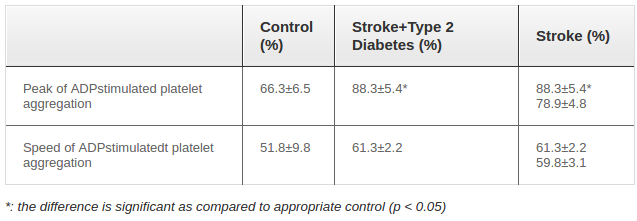
The results obtained in the study of platelets aggregation in response to ADP are presented in Table 1 . An enhancement of the both investigated parameters (peak and speed of ADP-dependent platelet aggregation) was established. The blood obtained from the person with stroke alone characterized less expressed changes comparing with the type 2 diabetes complicated stroke. The peak of platelet aggregation in response to ADP in patient with type 2 diabetes and stroke exceeded the control parameters more than one-third and this aggregation index increased less than 20% under ischemic stroke conditions.
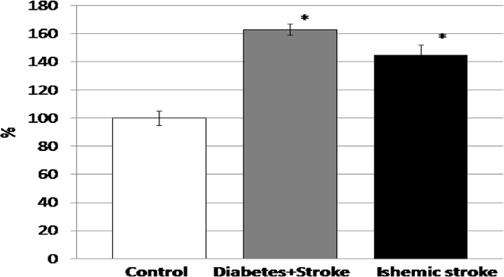
The investigation of content of blood glycoprotein that mediates the platelet adhesion to vascular damage sites binding to specific glycoprotein on platelet membrane and to constituents of exposed connective tissue, von Willebrand factor (VWF) revealed its growing up in patients with stroke both with or without type 2 diabetes ( Figure 2 ). What is more the increase of plasma VWF content under stroke complicated hyperglycemia was more expressed and reached 163% from the control value while the ischemic stroke patient plasma characterized 145% from the control content of von Willebrand factor.
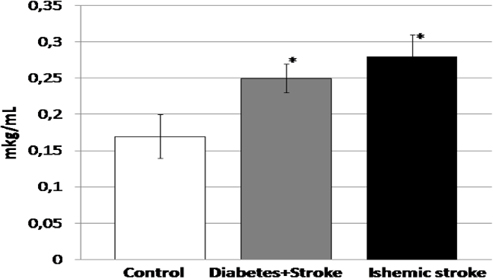
The serotonin serum content measurements showed the statistically significant increase of this parameter in 1.5 times ( Figure 3 ). Besides the rising of the biogenic amine content was more in patients with ischemic stroke and amount more than 164% comparing the control.
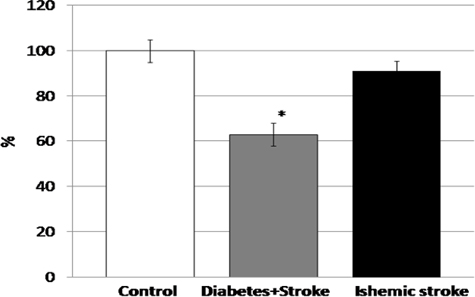
Unlike abovementioned parameters investigated in the present study having tendency to raise the activity of monoamino oxidase enzyme was decrease of 37% comparing with the control in case of ischemic stroke complicated with type 2 diabetes ( Figure 4 ).
Discussion
Previous studies have documented various platelet abnormalities in cerebrovascular disease, e.g., platelet count, mean platelet volume andplatelet aggregation parameters Smith et al., 1999. There was a data that platelet count was reduced in acute stroke patients compared with control subjects Smith et al., 1999. Thus the similar results were got in our investigations. So the overall mean platelet count for ischemic stroke was much lower of the control values. It is however in contrast to the findings of a ischemic stroke there were a lot of studies revealed a higher mean platelet count for diabetics than for the controls Akinsegun et al., 2014. But our results showed the decrease of platelet count in patients with stroke complicated by type 2 diabetes, although this decrease was less than in case of stroke alone. So, it was established, ischemic stroke was characterized by reduced platelet count even in diabetes condition. The platelet counts are thrombotic potential indicators and risk factor for microvascular complications. The identified changes of platelet count could make a negative impact, particularly on the condition of severe bleeding and breach of clot formation. Platelet aggregation blood test in response to ADP checks how well platelets, clump together and cause blood to clot Schmaier, 2013. The numerous previous investigation had generally showed platelet aggregation enhance in post-ischemic period Smith et al., 1999. This data confirmed wide and effective using for prevention and treatment of stroke platelet aggregation inhibitors aspirin and clopidogrel. Clopidogrel acts by inhibiting the P2Y12 subtype of ADP receptor on platelet cell membranes Topçuoglu et al., 2011. Thus our results indicate the increase of both the peak and speed of platelet aggregation in response to ADP in subjects with ischemic stroke. So platelet hyperactivation plays a crucial role in the pathophysiology of cerebral ischemia disease and to some extent could be a compensatory response to the decrease in platelet count identified by us. It should also be noted that platelet aggregation in response to ADP in a stroke with type 2 diabetes increased even more comparing with stroke alone. Hyperglycemia and other metabolic conditions of diabetes are aggravating factors for the development of platelets functioning changes, although the effect on platelet count was less pronounced in case of stroke with diabetes. The previous platelets studies of patients with diabetes have revealed the increased aggregation in response to ADP, a reaction assumed to be mediated by the upregulation of GPIIb-IIIa receptors occurring in patients with diabetes. It is normally insulin that inhibits platelet aggregation in response to ADP in vitro; though, this reaction is lowered in patients with diabetes as well as thromboxane A2 increased levels, possibly contributing to hyperaaggregation Air and Kissela, 2007.
The number of studies has therefore suggested that factors of coagulation, including von Willebrand, rise together with resistance to insulin under diabetes and thus amplified procoagulation state. Besides it is known that high von Willebrand factor levels are usually associated with the risk of stroke in relatively healthy people. The plasma glycoprotein von Willebrand factor (vWF) plays an important role in hemostasis as it promotes platelet joining and aggregation to vascular injury sites and acts as a protein carrier for Factor VIII. The release of vWF increases when endothelial cells are activated or damaged. Therefore, the level of vWF in plasma is considered to be a signalling factor of endothelial dysfunction, a condition that predisposes to atherosclerosis and thrombosis. Because of its direct role in hemostasis, and its indirect role as a signalling factor of endothelial dysfunction, vWF is a potential risk indicator for cerebrovascular disease Wieberdink et al., 2010.
So the increase of von Willebrand factor content in the blood of patients with ischemic stroke was established in our investigation corresponded to the literature data. Ourstudies have revealed aggravating diabetes influence on rising of vWF blood content in patients with stroke. The ischemic stroke conditions characterized increase vWF blood content more than 40 percent and stroke complicated of type 2 diabetes -60 percent comparing with the control.
Whereas vWF plays a major role in blood coagulation, increased vWF plasma levels accompanied by reinforced platelet aggregation in response to ADP could contribute to an increased risk of thrombosis particularly in the 2nd type of diabetes condition, so plasma vWF levels could be associated with the risk of stroke specialy with complicated by diabetes.
Von Willebrand factor is accumulated in α-granules of platelet and δ granules containing ADP or ATP and serotonin (5-hydroxytryptamine (5-HT). Extrication of ATP and serotonin are both increased in acute ischemic stroke. In addition, the basal level of 5-HT has been depicted to be less in IS in comparison to a control group, suggesting that the platelet storage granules are partially depleted prior to stimulation with agonists Smith et al., 1999. So the next aim of our study was to measure the serum 5- hydroxytryptamine blood content in ischemic stroke alone and with stroke and diabetes subjects. The pronounced increase of 5-HT content was demonstrated in both studied pathologies. Moreover, a large deviation from the control was observed in the blood of patients with IS alone. The platelets release serotonin to blood when they bind to a clot. It serves as a vasoconstrictor and helps to regulate hemostasis and blood clotting so the excessively high amount of this amine in blood could have the negative consequences particularly for normal blood flow. The causes of identified changes of 5-HT content could be or its increased synthesis and accumulation or a violation of its decay, which is provided by an enzyme monoamine oxidase. The activity of MAO was reduced especially pronounced in patients with stroke accompanied by diabetes. Such results confirmed by A. D. Mosnaim et.al, that showeda significant reduction in blood platelets' monoamine oxidase (MAO) activity in insulin-dependent diabetics when compared with the controls Mosnaim et al., 1979.
Conclusion
The obtained data suggested a significant imbalance in vascular platelet element of hemostasis under the ischemic stroke and amplification of negative changes of such indicators like aggregation in response to ADP, content of von Willebrand factor and MAO activity in blood persons with stroke accompanying of type 2 diabetes.
References
-
B.
A.
The colorimetric method for determining the monoamine oxidase activity in blood serum. Laboratory case.
1976;
3
:
151-152
.
-
E.L.
Air,
B.M.
Kissela.
Diabetes, the metabolic syndrome, and ischemic stroke epidemiology and possible mechanisms. Diabetes care.
2007;
30
:
3131-3140
.
-
A.
Akinsegun,
D.A.
Olusola,
J.-O.
Sarah,
O.
Olajumoke,
A.
Adewumi,
O.
Majeed,
O.
Anthonia,
U.
Ebele,
O.
Olaitan,
A.
Olanrewaju.
Mean platelet volume and platelet counts in type 2 Diabetes: Mellitus on treatment and non-diabetic mellitus controls in Lagos, Nigeria. Pan African Medical Journal.
2014;
18
.
-
T.M.
Davis,
H.
Millns,
I.M.
Stratton,
R.R.
Holman,
R.C.
Turner.
Risk factors for stroke in type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS) 29. Archives of internal medicine.
1999;
159
:
1097-1103
.
-
S.
Fateh-Moghadam,
P.
Htun,
B.
Tomandl,
D.
Sander,
K.
Stellos,
T.
Geisler,
H.
Langer,
K.
Walton,
R.
Handschu,
C.
Garlichs.
Hyperresponsiveness of platelets in ischemic stroke. THROMBOSIS AND HAEMOSTASIS-STUTTGART-.
2007;
97
:
974
.
-
I.D.
Federation.
I.D.A.S. Edition, ed. 2015
.
-
K.
Hara,
Y.
Hirowatari,
Y.
Shimura,
H.
Takahashi.
Serotonin levels in platelet-poor plasma and whole blood in people with type 2 diabetes with chronic kidney disease. Diabetes research and clinical.
2011;
practice94
:
167-171
.
-
E. S.V.
Maksimenko.
The level of tryptophan and serotonin in the convulsive readiness conditions of cerebrum. the bulletin of Kharkiv Karazin University The series “Medicine”.
2000;
494
:
440-443
.
-
A.D.
Mosnaim,
M.E.
Wolf,
S.
Huprikar,
S.P.
Singh,
E.A.
Zeller.
Reduced monoamine oxidase activity in blood platelets from insulin-dependent diabetic subjects. Diabetes.
1979;
28
:
455-456
.
-
T.
O’malley,
P.
Langhorne,
R.
Elton,
C.
Stewart.
Platelet size in stroke patients. Stroke.
1995;
26
:
995-999
.
-
W.H.
Organization.
Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: report of a WH. 2006
.
-
A.
Schmaier.
Laboratory evaluation of hemostatic and thrombotic disorders. Hoffman Hematology: Basic Principles and Practice 6th ed Philadelphia, Pa: Churchill Livingstone Elsevier.
2013;
:
319
.
-
N.M.
Smith,
R.
Pathansali,
P.M.
Bath.
Platelets and stroke. Vascular Medicine.
1999;
4
:
165-172
.
-
T.
Tamayo,
J.
Rosenbauer,
S.
Wild,
A.
Spijkerman,
C.
Baan,
N.
Forouhi,
C.
Herder,
W.
Rathmann.
Diabetes in Europe: an update. Diabetes research and clinical practice.
2014;
103
:
206-217
.
-
T.P.
Tokar AV Makogonenko EM.
Modern methods of laboratory diagnosis of intravascular blood microcoagulation (guidelines). Science idea Kyiv.
1994
.
-
M.A.
Topçuoglu,
E.M.
Arsava,
H.
Ay.
Antiplatelet resistance in stroke. Expert review of neurotherapeutics.
2011;
11
:
251-263
.
-
A.I.
Vinik,
T.
Erbas,
T.S.
Park,
R.
Nolan,
G.L.
Pittenger.
Platelet dysfunction in type 2 diabetes. Diabetes care.
2001;
24
:
1476-1485
.
-
H.
Weissbach,
T.P.
Waalkes,
S.
Udenfriend.
A simplified method for measuring serotonin in tissues; simultaneous assay of both serotonin and histamine. Journal of Biological Chemistry.
1958;
230
:
865-871
.
-
R.G.
Wieberdink,
M.C.
van Schie,
P.J.
Koudstaal,
A.
Hofman,
J.C.
Witteman,
M.P.
de Maat,
F.W.
Leebeek,
M.M.
Breteler.
High von Willebrand Factor Levels Increase the Risk of Stroke The Rotterdam Study. Stroke.
2010;
41
:
2151-2156
.
Comments
Downloads
Article Details
Volume & Issue : Vol 3 No 03 (2016)
Page No.: 542-547
Published on: 2016-03-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5203 times
- Download PDF downloaded - 1836 times
- View Article downloaded - 5 times
 Biomedpress
Biomedpress