Abstract
Background: Acquired hemophilia A (AHA) develops due to autoantibodies directed against factor VIII. It can occur spontaneously or be triggered by various factors. Here, we report a case of AHA induced by the Pfizer-BioNTech COVID-19 vaccine in an older patient.
Case presentation: The patient presented with multiple spontaneous bruises after receiving the Pfizer-BioNTech COVID-19 vaccine. Laboratory investigations revealed an isolated prolonged activated partial thromboplastin time (APTT) with an uncorrected mixing test. The factor VIII level was found to be low (0.6%). Additionally, the Bethesda assay evidenced the presence of an inhibitor of factor VIII. The patient was administered IV methylprednisolone and recombinant factor VIII. Then, he was maintained with oral azathioprine and prednisolone. However, the patient's condition showed no significant improvement. Thus, rituximab was administered, to which the patient responded well.
Discussion and conclusion: AHA is a rare adverse effect of the Pfizer-BioNTech COVID-19 vaccine. Although the exact mechanism underlying the development of this condition following vaccination against COVID-19 remains unclear, a diagnosis of AHA should be considered if a patient without a bleeding history presents with acute-onset bleeding and an isolated prolonged APTT.
Introduction
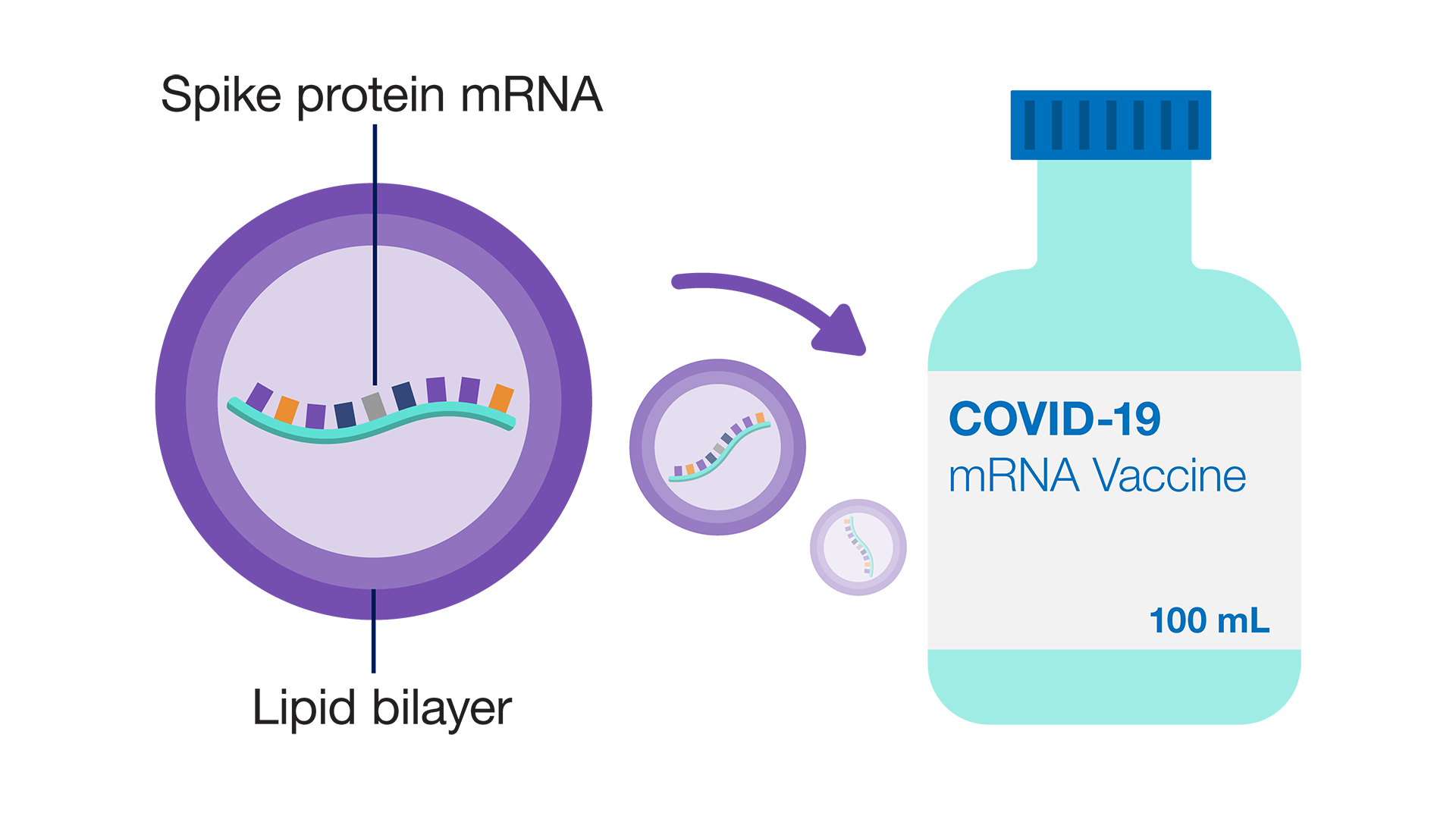
Acquired hemophilia A (AHA) is a rare condition characterized by the development of autoantibodies against clotting factor VIII. These autoantibodies are also known as inhibitors. AHA can occur spontaneously or be triggered by various factors, including pregnancy, immune diseases, dermatological disorders, medications, and infections. The presentation of AHA varies, encompassing no bleeding, mild bleeding, and life-threatening bleeding1. The nonlinear pharmacokinetics of the interaction between factor VIII and type II inhibitors characterize the inhibition of factor VIII by autoantibodies. The incidence of AHA is about 1 to 4 million cases per year2. AHA induced by COVID-19 vaccination is an exceedingly rare event. The number of reported cases remains very low, considering the large number of individuals who have received COVID-19 vaccination worldwide. The SARS-CoV-2 spike protein is a primary target of neutralizing antibodies encoded by the mRNA in some COVID-19 vaccines3. Here, we present the case of a patient with bleeding symptoms that developed after receiving the Pfizer BioNTech (BNT162b2) mRNA COVID-19 vaccine.
Case presentation
A 72-year-old man presented to a primary health clinic with spontaneous bruising on his left arm 5 days post the first dose of the Pfizer BioNTech (BNT162b2) mRNA COVID-19 vaccine. He also complained of worsening left cheek swelling. He denied a recent history of trauma. He was advised to apply cold compression and discharged. A week later, he presented again with new ecchymoses on the right flank and thigh. He also had underlying diabetes mellitus and hypertension. He had been on multiple medications, including metformin 500 mg BD, vildagliptin 50 mg BD, perindopril 4 mg and indapamide 1.25 mg OM, amlodipine 10 mg OD, and aspirin 75 mg OD. Examination revealed a 2×2 cm hematoma in the left buccal region. The ecchymoses on the right flank and right thigh measured about 15×10 cm and 6×8 cm, respectively. The initial coagulation profile showed an isolated prolonged activated partial thromboplastin time (APTT) and anemia with a hemoglobin level of 7.4 g/dL. Both an immediate mixing test and a test 2 hours post incubation were not corrected. The level of factor VIII was very low (0.6%) and that of factor IX was 80.5%. The Bethesda assay revealed a factor VIII inhibitor level of 19.2 BU. The patient was started on IV methylprednisolone 500 mg OD for 3 days. A single dose of recombinant factor VIII 90 mcg/kg was administered to reduce bleeding. The patient’s body weight was 74 kg. He was continued on oral azathioprine 100 mg OD for 2 months and prednisolone 40 mg OD, tapering to 5 mg OD within a 3-month duration. However, while on azathioprine and the tapering steroid dose, his factor VIII and factor VIII inhibitor levels showed no significant improvement (6.1% and 16.8 BU, respectively). He was then started on rituximab, to which he responded well; the factor VIII level rose to 221%, and the factor VIII inhibitor was not detected upon repeat testing. Von Willebrand factor activity was normal. Additionally, tumor markers and autoantibody screening were unremarkable. Lupus anticoagulant was not tested in this case. The patient’s laboratory investigations are summarized in Table 1. A computed tomography scan of the thorax-abdomen-pelvis did not reveal any malignancy, nor did esophagogastroduodenoscopy and sigmoidoscopy.
| Laboratory Parameters (unit) | Results |
|---|---|
| Haemoglobin (g/dL) | 7.4 |
| APTT (sec) | 94.8 (reference range: 28.1-39.7 sec) |
| PT (sec) | 10.7 (reference range: 9.4-12.5 sec) |
| APTT Mixing test (sec) | |
| Immediate | 47.0 (Not corrected) |
| Post 2 hours incubation | 63.5 (Not corrected) |
| Initial Factor assay (%) | |
| Factor VIII | 0.6 |
| Factor IX | 80.5 (reference range: 65-150%) |
| Initial Factor Inhibitor level (Bethesda Assay) (BU) | 19.2 |
| Von Willebrand’s study | |
| VWF RiCof (%) | 115.6 (reference range: 59.8-131.5%) |
| VWF Antigen (%) | 122.6 (reference range: 52.9-182.5%) |
| Follow up Factor VIII (%) | 221 |
| Follow up Factor Inhibitor level | Below lower limit of detection |
Discussion
The Pfizer BioNTech SARS-CoV-2 mRNA vaccine was among the first to receive emergency authorization for use to mitigate COVID-19 worldwide. Since then, certain adverse effects have been reported, including acute myocardial infarction, Bell’s palsy, cerebral venous sinus thrombosis, Guillain-Barre syndrome, myocarditis, pulmonary embolism, stroke, thrombosis with thrombocytopenia syndrome, lymphadenopathy, appendicitis, herpes zoster reactivation, neurological complications, autoimmune hepatitis, and autoimmune peripheral neuropathies4. AHA is a rare adverse effect of COVID-19 vaccination. Several case reports have documented the development of acquired hemophilia following COVID-19 vaccination. A systematic review by Massimo et al. describing 96 patients with acquired hemophilia reported COVID-19 vaccines as a suspected causative agent, regardless of the vaccine products. Most of the cases involved older patients over 65 years of age. Additionally, most of the cases (n = 70) were reported following vaccination with the Pfizer BioNTech vaccine, like in our case5.
AHA is a rare disease and occurs unexpectedly. Two peaks of AHA incidence are typically observed, one associated with pregnancy and the other with older age (> 60 years). Most older patients with AHA are found to have comorbidities and a history of medication use. A diagnosis of AHA should be considered if the patient presents with acute- or recent-onset bleeding, an isolated prolonged APTT, and no bleeding history. The diagnosis and treatment are described as usually delayed. However, the cause of AHA is still unknown1, 6.
In this case, the symptoms appeared on Day 5 after receipt of the Pfizer BioNTech COVID-19 vaccine, indicating their relation to the vaccination. To date, the exact mechanism underlying the development of acquired hemophilia after COVID-19 vaccination remains unclear. Vaccine-induced immune dysregulation may trigger the development of autoantibodies against clotting factors. The antigenic mimicry of SARS-CoV-2 regarding factor VIII may lead to the uncontrollable degradation of factor VIII. Anti-spike IgG is an antigen specificity that is induced by mRNA COVID-19 vaccines7. The vaccine antigens may mimic endogenous clotting factors, triggering an autoimmune response8. Another possible mechanism involves the stimulation of dormant T or B cells. The activation of T cell clones may result in the production of autoantibodies, occurring after the presentation of SARS-CoV-2 spike proteins to T cell clones. The stimulation of broad Toll-like receptors may also cause the activation of clonal B cells and lead to the production of antibodies against factor VIII7, 8, 9.
It is recommended that hemostatic treatment be initiated in patients with AHA and clinically relevant bleeding, irrespective of inhibitor titer and residual factor VIII activity. Controlling the acute bleeds and preventing further injury are priorities. The first-line treatment for acute bleeding includes recombinant activated factor VII and activated prothrombin concentrate complex. Recombinant or human factor VIII concentrates and desmopressin can only be used if a bypassing agent is unavailable. The next treatment goal is to achieve remission of AHA by starting immunosuppressive therapy, which includes corticosteroid therapy with or without cyclophosphamide. Rituximab can be used as a second-line therapy, as in our case. If factor VIII levels are > 1% and inhibitors are < 20 BU/ml, steroids can be administered alone for 3–4 weeks, and cyclophosphamide or rituximab can be added if no response is observed. If the factor VIII level is < 1% or the inhibitor is > 20 BU/ml, patients can be given steroids plus cyclophosphamide or rituximab1. Several AHA patients described by Lee et al. and Alvarado et al. were also given IV methylprednisolone 500 mg/day for 3 days, similar to this patient10, 11. Even though there are no articles highlighting the specific treatment of AHA induced by COVID-19 vaccination, our patient showed improvement after receiving treatment following the above recommendations.
Conclusions
In conclusion, this paper highlights AHA as one of the complications of the Pfizer-BioNTech COVID-19 vaccine and the need for clinicians to be alert if the same vaccine is to be administered in the future. Crucially, the occurrence of acquired hemophilia after COVID-19 vaccination is still being investigated, and more research is needed to establish a definite link. However, it is worth noting that the overall benefits of COVID-19 vaccination in preventing severe illness from this infection currently outweigh any potential risks.
Abbreviations
AHA : Acquired Haemophilia A, BD : Twice daily, BU : Bethesda unit, OD : Once daily, OM : Once in the morning, RiCof : Ristocetin cofactor, VWF : Von Willebrand factor
Acknowledgments
We would like to thank the staffs of Pathology Department, Hospital Tengku Ampuan Afzan who were directly or indirectly involved in the processing of this patient’s sample for the laboratory investigations.
Author’s contributions
A.D, M.A, and S.A wrote this manuscript, N.M.A and S.I.S involved in laboratory investigation interpretation, and S.A.W involved in the patients’ management. The final manuscript was reviewed and approved by all authors.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Tiede
A.,
Collins
P.,
Knoebl
P.,
Teitel
J.,
Kessler
C.,
Shima
M.,
International recommendations on the diagnosis and treatment of acquired hemophilia A. Haematologica.
2020;
105
(7)
:
1791-801
.
View Article PubMed Google Scholar -
Elezović
I.,
Acquired haemophilia syndrome: pathophysiology and therapy. Srpski Arhiv za Celokupno Lekarstvo.
2010;
138
:
64-8
.
View Article PubMed Google Scholar -
Teijaro
J.R.,
Farber
D.L.,
COVID-19 vaccines: modes of immune activation and future challenges. Nature Reviews Immunology.
2021;
21
(4)
:
195-7
.
View Article Google Scholar -
Trougakos
I.P.,
Terpos
E.,
Alexopoulos
H.,
Politou
M.,
Paraskevis
D.,
Scorilas
A.,
Adverse effects of COVID-19 mRNA vaccines: the spike hypothesis. Trends in Molecular Medicine.
2022;
28
(7)
:
542-54
.
View Article PubMed Google Scholar -
Franchini
M.,
Cappello
E.,
Valdiserra
G.,
Bonaso
M.,
Moretti
U.,
Focosi
D.,
Investigating a Signal of Acquired Hemophilia Associated with COVID-19 Vaccination: A Systematic Case Review. InSeminars in Thrombosis and Hemostasis.
2022;
49
(1)
:
015-026
.
View Article Google Scholar -
Nowak
K.M.,
Carpinteiro
A.,
Szalai
C.,
Saner
F.H.,
Acquired Hemophilia A: A Permanent Challenge for All Physicians. Medicines.
2022;
9
(3)
:
21
.
View Article Google Scholar -
Hirsiger
J.R.,
Martinez
M.,
Tsakiris
D.A.,
Cittone
M.G.,
Graf
L.,
Oldenburg
J.,
Investigating potential mechanisms underlying FVIII inhibition in acquired hemophilia A associated with mRNA COVID-19 vaccines. Journal of Thrombosis and Haemostasis.
2022;
20
(4)
:
1015-8
.
View Article Google Scholar -
Portuguese
A.J.,
Sunga
C.,
Kruse-Jarres
R.,
Gernsheimer
T.,
Abkowitz
J.,
Autoimmune- and complement-mediated hematologic condition recrudescence following SARS-CoV-2 vaccination. Blood Advances.
2021;
5
(13)
:
2794-8
.
View Article PubMed Google Scholar -
Amisha
F.,
Saluja
P.,
Malik
P.,
Van Rhee
F.,
Acquired hemophilia A (AHA) due to anti-SARS-CoV-2 vaccination: A systematic review. eJHaem.
2023;
4
(2)
:
532-43
.
View Article PubMed Google Scholar -
Alvarado
Y.,
Yao
X.,
Jumper
C.,
Hardwicke
F.,
D'Cunha
N.,
Cobos
E.,
Acquired hemophilia: a case report of 2 patients with acquired factor VIII inhibitor treated with rituximab plus a short course of steroid and review of the literature. Clinical and Applied Thrombosis/Hemostasis.
2007;
13
(4)
:
443-8
.
View Article PubMed Google Scholar -
Lee
C.P.,
Khalid
B.B.,
A case series of acquired haemophilia in a Malaysian hospital: unpredictably rare medical emergency. Oxford Medical Case Reports.
2015;
2015
(10)
:
330-2
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 11 (2023)
Page No.: 6019-6022
Published on: 2023-11-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 2706 times
- PDF downloaded - 1159 times
- XML downloaded - 86 times
 Biomedpress
Biomedpress

