Abstract
Background: Few studies have investigated the pain-reducing effects of bupivacaine after laparoscopic hysterectomy. Therefore, this study compared the efficacy of three methods of bupivacaine injection?subcutaneous injection into the trocar site, intraperitoneal injection, and posterior transversus abdominis muscle block under laparoscopic guidance?for reducing pain after laparoscopic hysterectomy; the efficacy of each method was also compared with that of placebo.
Methods: This double-blind randomized clinical trial study included 95 patients with good general health who underwent elective laparoscopic hysterectomy for benign disease in 2021. The patients were allocated into three intervention groups (subcutaneous injection of 10 cc bupivacaine 0.25%, heavy under trocar sites; 10 cc bupivacaine 0.25%, heavy injection into the transversus abdominis plane block; and 10 cc bupivacaine 0.25%, heavy intraperitoneal injection) and a control group. Abdominal and shoulder pain 2?4, 8, 12, and 24 h after the surgery were compared between groups.
Results: The four groups were homogenous in age, weight, height, body mass index, surgery duration, surgery type, and family history of cancer (P > 0.05). The mean abdominal and shoulder pain score significantly decreased from the first time point (hours 2?4) to 8, 12, and 24 hours after surgery in the trocar site, intraperitoneal, and control groups (P < 0.001). However, we did not observe a significant decrease in abdominal and shoulder pain in the transversus abdominis plane block group (P > 0.05).
Conclusion: The present study indicates that bupivacaine administration methods of transversus abdominis plane block and trocar site injection are effective and safe for reducing pain following laparoscopic hysterectomy.
Introduction
Laparoscopy is a common surgical method for the diagnosis and treatment of gynecological diseases1. During laparoscopy, the surgeon injects carbon dioxide (CO2) gas into the patient’s abdomen (pneumoperitoneum). This inflates the abdomen, allowing the surgeon to see the organs inside the abdominal cavity and perform the surgery. However, the inflation of the abdomen may cause nerve irritation extending from the upper abdomen (diaphragm) to the shoulders and neck. This phenomenon often causes pain, especially in the surgical area and shoulders2. Visceral pain or pain at the surgical site is generally caused by stretching in the abdominal cavity and irritation of the peritoneum due to CO2 gas. In addition, shoulder pain is attributable to the stimulation of the phrenic nerve by injecting CO2 gas into the abdominal cavity and below the diaphragm. Shoulder pain is also associated with the stimulation of the parietal peritoneum. Patients typically experience severe pain in the first 24 hours after laparoscopic surgery3. Evidence suggests that over 80% of women experience pain at the surgical site and shoulder after laparoscopy, which can cause complications, delays in discharge, and rehospitalization2, 4. These problems increase the financial burden and reduce patient satisfaction5.
The intraperitoneal injection of several drugs, such as bupivacaine, is a method of reducing pain after laparoscopic surgery6. Studies have also investigated other methods to reduce pain after surgery, including local anesthesia7. However, pain control after surgery emphasizes non-drug approaches or reduced drug doses8; this is because excessive narcotic painkiller use is a clinical challenge that can cause overdose, sedation, increased nausea and vomiting, ileus paralysis, and even death9, 10.
In addition to the intraperitoneal injection of bupivacaine and other drugs11, transversus abdominis muscle block injection can also be used to reduce lower abdominal visceral pain after surgery. Posterior transversus abdominis muscle block blocks anterior cutaneous branches T9–T1212. In recent years, researchers have directed much attention toward preventive analgesia—specifically, preventing pain transmission before pain stimulation by beginning treatment before pain occurs and continuing treatment afterward13. Because of the lack of studies in this field, this study compared the efficacy of three methods of bupivacaine administration—subcutaneous injection, intraperitoneal injection, and posterior transversus abdominis muscle block under laparoscopic guidance—for reducing pain after laparoscopic hysterectomy surgery. The efficacy of each method was also compared with that of placebo.
Methods
This study was a double-blind randomized clinical trial study involving 95 patients who underwent elective laparoscopic hysterectomy for benign disease at Arash Hospital (affiliated with Tehran University of Medical Sciences). All patients had good general health (classified as American Society of Anesthesiologists (ASA) Grades 1 and 2) and underwent surgery in 2021.
The estimated required sample size was 20 patients per group (three intervention groups and one control group), considering a type 1 error level of 5% and a power of 80% as well as the parameters in Karman et al.’s study14, in which the average pain score after 24 hours in the resting state for the intraperitoneal levobupivacaine and periportal groups were 14.9 ± 7.6 and 9.7 ± 2.2, respectively. The following equation was used to calculate the required sample size in the control group:
Sample size in placebo group = n×Number of treatment group=20 × 3=35
All patients who were candidates for elective laparoscopic hysterectomy were referred to Arash Hospital and had good general health (ASA grades 1 and 2). Moreover, they were candidates for hysterectomy due to benign disease. Patients with chronic pelvic pain, pregnancy, sensitivity to bupivacaine, emergency surgery, and cancer were excluded from the study.
The Ethical Committee of the Tehran University of Medical Sciences approved the protocol of the present study (ethics committee code: IR.TUMS.MEDICINE.REC.1401.020), and it was registered in the Iranian Registry of Clinical Trials (IRCT registration number: IRCT20110530006640N9, registration date: 2022-09-11).
After providing written informed consent, the patients were allocated into the three intervention groups (subcutaneous injection of 10 cc bupivacaine 0.25%, heavy under trocar sites; 10 cc bupivacaine 0.25%, heavy injection into the transversus abdominis plane block; and 10 cc bupivacaine 0.25%, heavy intraperitoneal injection) and a control group.
The balance block randomization method (considering a block size equal to 19 and five sequences) was used for the randomization process to ensure that the sample size was the same in each group. The study used a double-blind design, so neither the patients nor the pain evaluator were aware of the method of analgesia after laparoscopic hysterectomy surgery. A laparoscopic fellowship doctor performed the anesthesia injection half an hour before the end of anesthesia induction.
Abdominal and shoulder pain were assessed 2–4, 8, 12, and 24 h after the surgery with a visual analog scale (VAS). The nurses of the ward performed scoring after the surgery without knowing the method of anesthesia administration. Complications after surgery, including the amount of narcotic use, the number of diclofenac suppositories and ketorolac ampoules, and nausea and vomiting, were recorded.
The baseline characteristics of the patients in the four groups were compared with the Chi-square test and one-way ANOVA. The mean analgesic dose and mean shoulder and abdominal pain scores at different time points after the intervention were compared with one-way ANOVA. Moreover, differences between the three intervention groups in the changes in the shoulder and abdominal pain scores over time were analyzed by repeated-measures ANOVA. Statistical significance was set as P ≤ 0.05. All statistical analyses were performed with Stata version 14.
| Variables | Treatment groups Treatment groups | P-value | ||||
|---|---|---|---|---|---|---|
| Group 1 (N = 20) | Group 2 (N = 20) | Group 3 (N = 20) | Group 4 (N = 35) | |||
| Continuous variables | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | ||
| Age (year) | 43.77 ± 9.14 | 38.20 ± 13.65 | 40.50 ± 11.48 | 39.64 ± 10.56 | 0.41 | |
| Weight (Kg) | 73.1 ± 10.83 | 70.35 ± 10.41 | 70.10 ± 13.01 | 69.45 ± 10.23 | 0.68 | |
| Height (cm) | 161.94 ± 5.55 | 164.7 ± 4.52 | 162.1 ± 4.77 | 162.51 ± 4.77 | 0.26 | |
| BMI (Kg/m 2 ) | 27.46 ± 4.16 | 26.1 ± 4.81 | 26.69 ± 5 | 26.37 ± 4.21 | 0.79 | |
| surgery duration (Hour) | 2.11 ± 0.23 | 2.13 ± 0.24 | 2.22 ± 0.15 | 2.15 ± 0.31 | 0.51 | |
| Categorical variables | N (%) | N (%) | N (%) | N (%) | < 0.001 | |
| Nausea | Yes | 0 | 0 | 6 (30) | 29 (82.9) | |
| No | 20 (100) | 17 (100) | 14 (70) | 6 (17.1) | ||
| Vomiting | Yes | 0 | 0 | 2 (10) | 11 (31.4) | < 0.001 |
| No | 20 (100) | 17 (100) | 18 (90) | 24 (68.6) | ||
| Family history of cancer | No | 19 (95) | 19 (95) | 20 (100) | 35 (100) | 0.41 |
| Yes | 1 (5) | 1 (5) | 0 | 0 | ||
| Surgery type | TLH ± BSO | 12 (60) | 13 (76.5) | 16 (84.2) | 20 (57.1) | 0.47 |
| TLH | 6 (30) | 4 (23.5) | 3 (15.8) | 12 (34.3) | ||
| TLH ± LSO | 2 (10) | 0 | 0 | 1 (2.9) | ||
| TLH ± RSO | 0 | 0 | 0 | 2 (5.7) | ||
| Group 1 N (%) | Group 2 N (%) | Group 3 N (%) | Group 4 N (%) | p | ||
|---|---|---|---|---|---|---|
| Narcotic | Mean ± SD | 0 | 0.20 ± 0.41 | 1.25 ± 0.63 | 1.45 ± 0.51 | < 0.001 |
| 0 mg | 20 (100) | 16 (80) | 2 (10) | 0 | < 0.001 | |
| 25 mg | 0 | 4 (20) | 11 (55) | 19 (54.3) | ||
| 50 mg | 0 | 0 | 7 (35) | 16 (45.7) | ||
| Diclofenac | Mean ± SD | 186.36 ± 56.02 | 220 ± 110.5 | 335 ± 81.27 | 402.85 ± 51.36 | < 0.001 |
| 0 mg | 1 (5) | 3 (15) | 0 | 0 | < 0.001 | |
| 100 mg | 1 (5) | 0 | 0 | 0 | ||
| 200 mg | 17 (75) | 8 (40) | 1 (5) | 0 | ||
| 300 mg | 1 (5) | 8 (40) | 13 (65) | 4 (11.4) | ||
| 400 mg | 0 | 1 (5) | 5 (25) | 26 (74.3) | ||
| 500 mg | 0 | 0 | 0 | 5 (14.3) | ||
| 600 mg | 0 | 0 | 1 (5) | 0 | ||
| Ketorolac | Mean ± SD | 24.54 ± 15.3 | 36.81 ± 20.56 | 68 ± 24.62 | 42.86 ± 15.06 | < 0.001 |
| 0 mg | 5 (25) | 3 (15) | 0 | 0 | < 0.001 | |
| 30 mg | 14 (70) | 10 (50) | 4 (20) | 20 (57.1) | ||
| 60 mg | 1 (5) | 7 (35) | 16 (80) | 15 (42.9) |
| Pain | Treatment groups | P-value | ||||
|---|---|---|---|---|---|---|
| Group 1 (Mean ± SD) | Group 2 (Mean ± SD) | Group 3 (Mean ± SD) | Group 4 (Mean ± SD) | |||
| Abdominal pain | 2-4 hours after surgery | 1.04 ± 0.21 | 2.3 ± 0.73 | 2.4 ± 0.6 | 3.31 ± 0.53 | < 0.001 |
| 8 hours after surgery | 1.18 ± 0.50 | 2 ± 0.92 | 2.74 ± 0.56 | 3 | < 0.001 | |
| 12 hours after surgery | 1.59 ± 0.50 | 1.75 ± 0.72 | 2.63 ± 0.49 | 2.17 ± 0.43 | < 0.001 | |
| 24 hours after surgery | 1.27 ± 0.46 | 1.4 ± 0.68 | 2.1 ± 0.45 | 2 | < 0.001 | |
| 48 hours after surgery | 1.09 ± 0.29 | 1.05 ± 0.69 | 1.8 ± 0.52 | 1.8 ± 0.41 | < 0.001 | |
| Shoulder pain | 2-4 hours after surgery | 1.04 ± 0.21 | 2.25 ± 0.71 | 2.20 ± 0.61 | 3.11 ± 0.41 | < 0.001 |
| 8 hours after surgery | 1.85 ± 0.87 | 2.47 ± 0.69 | 2.94 ± 0.69 | 2.94 ± 0.23 | < 0.001 | |
| 12 hours after surgery | 1.54 ± 0.51 | 1.50 ± 0.76 | 2.50 ± 0.61 | 2.28 ± 0.45 | < 0.001 | |
| 24 hours after surgery | 1.18 ± 0.39 | 1.50 ± 0.68 | 2.10 ± 0.55 | 2 ± 0.001 | < 0.001 | |
| 48 hours after surgery | 1.09 ± 0.29 | 1.05 ± 0.68 | 1.70 ± 0.47 | 1.77 ± 0.42 | < 0.001 | |
Results
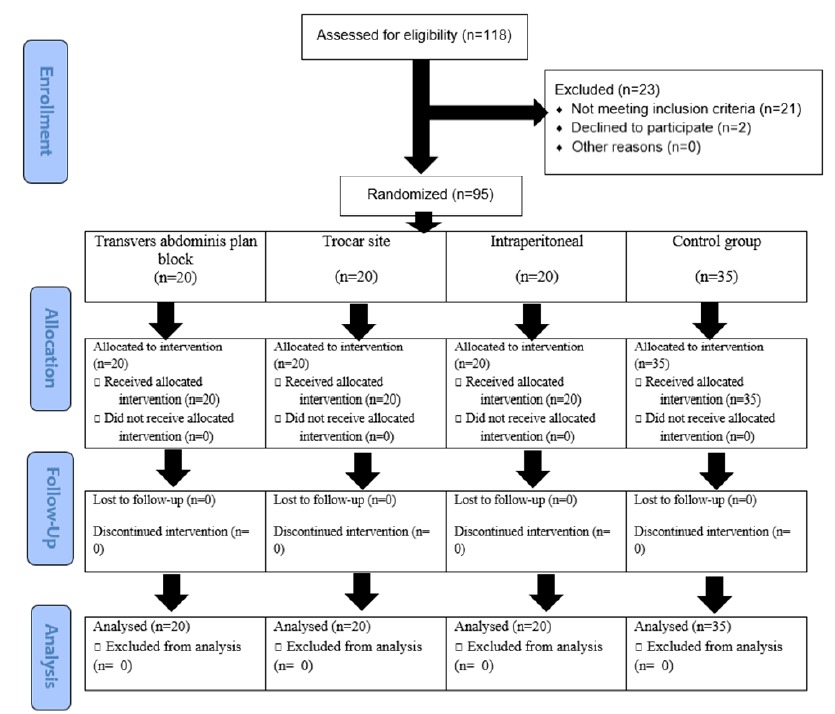
A total of 118 patients were assessed for eligibility; 21 patients did not meet the eligibility criteria, and 2 patients declined to participate in the study. The remaining 95 eligible patients were randomly allocated into the four groups. All patients received the allocated intervention, continued the intervention until the end of the study, and were included in the final analysis (Figure 1). Table 1 displays a comparison of the demographic and clinical characteristics of the patients between study groups. The four groups were homogenous in age, weight, height, body mass index (BMI), surgery duration, surgery type, and family history of cancer (P > 0.05). The rate of nausea and vomiting was significantly higher in the control group than in the three intervention groups (P < 0.001).
Table 2 presents a comparison of the study groups according to the doses of administered analgesics. Patients in the control group received higher doses of narcotics and diclofenac than patients in the transversus abdominis plane block group, who did not receive any narcotics (P < 0.001). Patients in the transversus abdominis plane block group received a lower dose of ketorolac (24.54 ± 15.3 mg), and patients in the intraperitoneal group received a higher dose of this drug (P < 0.001).
Table 3 and Figure 2 present a comparison of the mean abdominal and shoulder pain scores between the four groups of patients 2–4, 8, 12, and 24 h after the surgery. The mean abdominal and shoulder pain score differed significantly between the groups at the mentioned time points; at most time points, patients in the control group reported higher pain scores, and patients in the transversus abdominis plane block group reported lower pain scores (P < 0.001). The mean abdominal and shoulder pain scores were significantly decreased from the first time point (hours 2–4) to hours 8, 12, and 24 after the surgery in the trocar site, intraperitoneal, and control groups (P < 0.001). However, we did not observe a significant decrease in abdominal and shoulder pain in the transversus abdominis plane block group (P > 0.05).
Discussion
Hysterectomy surgery is a common major surgical procedure in women15. Patients experience less postoperative pain and lower morbidity with laparoscopic hysterectomy than with open surgery, and they recover more quickly and stay in the hospital for a shorter time16. After laparoscopic surgery, uncontrolled pain negatively impacts patients’ well-being by disrupting their sleep and potentially causing myocardial infarction, cardiac arrhythmia, ileus, and poor wound healing17. In recent years, alternative methods of pain relief, such as intraperitoneal local anesthesia, have become increasingly popular because they have fewer side effects and require less invasive approaches18.
Non-opioid pain therapy has been evaluated in patients undergoing laparoscopic and vaginal hysterectomies. It is challenging to draw convincing conclusions from the literature on this subject because the data are heterogeneous and contradictory19. Therefore, it is essential to conduct high-quality research on each medication type and approach for post-hysterectomy pain management. Bupivacaine is a well-known local anesthetic that reduces sodium permeability, increases the threshold of action, and prevents nerve conduction20.
This study compared the efficacy of three methods of bupivacaine administration for reducing pain after laparoscopic hysterectomy. The patients in transversus abdominis plane block and trocar site groups did not report any nausea or vomiting. Patients in the transversus abdominis plane block group did not receive any narcotics and received lower doses of ketorolac and diclofenac than patients in the other groups. Moreover, patients in this group had the lowest abdominal and shoulder pain scores. Previous meta-analyses have found that bupivacaine has no major side effects in patients undergoing laparoscopic gynecologic surgery who received intraperitoneal local analgesia, and bupivacaine was effective in reducing postoperative pain21, 22.
Our results are consistent with those previous reports that have examined intraperitoneal local anesthesia for postoperative pain control23, 24. However, other results contradict those of the present study. Another double-blind, randomized controlled trial reported that intraperitoneal bupivacaine instillation at the end of laparoscopic hysterectomy did not reduce postoperative pain, and overall patient satisfaction and complication rates were unchanged, as were opioid analgesic use, hospital stay length, and opioid analgesic use. However, laparoscopic gynecologic surgery resulted in low levels of self-reported postoperative pain in both groups25. Moreover, the results of El Hachem et al.’s study found no statistically significant difference in pain reduction between injection in the transversus abdominis plane block site versus injection in the trocar area26. Contrary to the results of the present study, Tam et al. demonstrated that bupivacaine injection at the trocar site did not significantly improve pain scores after laparoscopic surgery27. This difference could be partially explained by the difference in sample size and thus the difference in power.
In line with the results of the present study, a study conducted by Elkabarity et al. in 2020 showed that patients who received subcutaneous bupivacaine injection as transversus abdominis plane block had significantly lower pain scores in the first 24 hours after surgery compared with those who received intraperitoneal injections, and they received significantly fewer narcotics. They concluded that this form of injection allows superior pain control and reduces the need for opioids after the operation28.
One limitation of the present study is that the surgeries were performed by two surgeons, and the patient-reported pain scores were collected by two people; therefore, inter-rater variability may have affected the results. Second, we conducted this study only on patients undergoing laparoscopic hysterectomy surgery, and therefore, more evidence is necessary to generalize the findings of this study to patients receiving other types of surgery.
Conclusions
This study showed that bupivacaine administration methods of transversus abdominis plane block and trocar site injection were effective and safe for reducing pain after laparoscopic hysterectomy.
Abbreviations
ASA: American Society of Anesthesiologists; BMI: Body mass index; SD: Standard deviation; VAS: Visual analog scale
Acknowledgments
Deputy of Research and Technology of Tehran University of Medical Sciences approved our study and financially supported the study. We would like gratefully acknowledge the medical staff of Arash Hospital.
Author’s contributions
All authors had the same contribution in different parts of the data collection and manuscript writing. MNM developed the study idea. NM analyzed the data. All authors read and approved the final manuscript.
Funding
Tehran University of Medical Sciences Funded the present study.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The Ethical Committee of the Tehran University of Medical Sciences approved the protocol of the present study (ethics committee code: IR.TUMS.MEDICINE.REC.1401.020), and it was registered in the Iranian Registry of Clinical Trials (IRCT registration number: IRCT20110530006640N9, registration date: 2022-09-11).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Argentino
G.L.,
Bueloni-Dias
F.N.,
Leite
N.J.,
Peres
G.F.,
Elias
L.V.,
Bortolani
V.C.,
The role of laparoscopy in the propaedeutics of gynecological diagnosis1. Acta Cirurgica Brasileira.
2019;
34
(1)
:
e20190010000010
.
View Article PubMed Google Scholar -
Kaloo
P.,
Armstrong
S.,
Kaloo
C.,
Jordan
V.,
Interventions to reduce shoulder pain following gynaecological laparoscopic procedures. Cochrane Database of Systematic Reviews.
2019;
1
.
View Article Google Scholar -
Zeeni
C.,
Chamsy
D.,
Khalil
A.,
Abu Musa
A.,
Al Hassanieh
M.,
Shebbo
F.,
Effect of postoperative Trendelenburg position on shoulder pain after gynecological laparoscopic procedures: a randomized clinical trial. BMC Anesthesiology.
2020;
20
(1)
:
27
.
View Article PubMed Google Scholar -
Sao
C.H.,
Chan-Tiopianco
M.,
Chung
K.C.,
Chen
Y.J.,
Horng
H.C.,
Lee
W.L.,
Pain after laparoscopic surgery: focus on shoulder-tip pain after gynecological laparoscopic surgery. Journal of the Chinese Medical Association.
2019;
82
(11)
:
819-26
.
View Article PubMed Google Scholar -
Taurchini
M.,
Del Naja
C.,
Tancredi
A.,
Enhanced Recovery After Surgery: a patient centered process. Journal of Visualized Surgery.
2018;
4
:
40
.
View Article PubMed Google Scholar -
Brusko
G.D.,
Kolcun
J.P.,
Heger
J.A.,
Levi
A.D.,
Manzano
G.R.,
Madhavan
K.,
Reductions in length of stay, narcotics use, and pain following implementation of an enhanced recovery after surgery program for 1- to 3-level lumbar fusion surgery. Neurosurgical Focus.
2019;
46
(4)
:
4
.
View Article PubMed Google Scholar -
Goto
T.,
What is the best pain control after thoracic surgery?. Journal of Thoracic Disease.
2018;
10
(3)
:
1335-8
.
View Article PubMed Google Scholar -
Webster
F.,
Rice
K.,
Katz
J.,
Bhattacharyya
O.,
Dale
C.,
Upshur
R.,
An ethnography of chronic pain management in primary care: the social organization of physicians' work in the midst of the opioid crisis. PLoS One.
2019;
14
(5)
:
e0215148
.
View Article PubMed Google Scholar -
Eldalal
O.,
Mosa
F.,
Oyebanji
O.,
Mahajan
A.,
Oroszi
T.,
The Correlation between Pharmacological Param-eters of Oxycodone and Opioid Epidemic. Journal of Pharmacy & Pharmaceutical Sciences.
2020;
4
:
186
.
-
Lavand'homme
P.,
Steyaert
A.,
Opioid-free anesthesia opioid side effects: tolerance and hyperalgesia. Best Practice & Research. Clinical Anaesthesiology.
2017;
31
(4)
:
487-98
.
View Article PubMed Google Scholar -
Zahra
A.A.,
Abo-Elenin
K.M.,
El-Fiky
E.M.,
Kasemy
Z.A.,
Helwa
A.M.,
Intra Peritoneal Instillation of Bupivacaine or Bupivacaine plus Magnesium Sulphate or Bupivacaine plus Dexamethasone on Post-Operative Pain after Laparoscopic Cholecystectomy: A Randomized Controlled Study. The Egyptian Journal of Hospital Medicine.
2021;
84
(1)
:
2655-62
.
View Article Google Scholar -
Suner
Z.C.,
Kalayci
D.,
Sen
O.,
Kaya
M.,
Unver
S.,
Oguz
G.,
Postoperative analgesia after total abdominal hysterectomy: is the transversus abdominis plane block effective?. Nigerian Journal of Clinical Practice.
2019;
22
(4)
:
478-84
.
View Article PubMed Google Scholar -
Glare
P.,
Aubrey
K.R.,
Myles
P.S.,
Transition from acute to chronic pain after surgery. Lancet.
2019;
393
(10180)
:
1537-46
.
View Article PubMed Google Scholar -
Karaman
Y.,
Kebapç\i
E.,
Görgün
M.,
Güvenli
Y.,
Tekgül
Z.,
Post-laparoscopic cholecystectomy pain: effects of preincisional infiltration and intraperitoneal levobupivacaine 0.25% on pain control-a randomized prospective double-blinded placebo-controlled trial. Turkish Journal of Anaesthesiology and Reanimation.
2014;
42
(2)
:
80-5
.
View Article PubMed Google Scholar -
Lee
S.H.,
Oh
S.R.,
Cho
Y.J.,
Han
M.,
Park
J.W.,
Kim
S.J.,
Comparison of vaginal hysterectomy and laparoscopic hysterectomy: a systematic review and meta-analysis. BMC Women & Health.
2019;
19
(1)
:
83
.
View Article PubMed Google Scholar -
Gendy
R.,
Walsh
C.A.,
Walsh
S.R.,
Karantanis
E.,
Vaginal hysterectomy versus total laparoscopic hysterectomy for benign disease: a metaanalysis of randomized controlled trials. American journal of obstetrics and gynecology.
2011;
204
(5)
:
388. e1-e8
.
View Article Google Scholar -
Sinatra
R.,
Causes and consequences of inadequate management of acute pain. Pain Medicine.
2010;
11
(12)
:
1859-71
.
View Article PubMed Google Scholar -
Das
N.T.,
Deshpande
C.,
Effects of intraperitoneal local anaesthetics bupivacaine and ropivacaine versus placebo on postoperative pain after laparoscopic cholecystectomy: a randomised double blind study. Journal of Clinical and Diagnostic Research : JCDR.
2017;
11
(7)
:
08-12
.
View Article PubMed Google Scholar -
Blanton
E.,
Lamvu
G.,
Patanwala
I.,
Barron
K.I.,
Witzeman
K.,
Tu
F.F.,
Non-opioid pain management in benign minimally invasive hysterectomy: A systematic review. American Journal of Obstetrics and Gynecology.
2017;
216
(6)
:
557-67
.
View Article PubMed Google Scholar -
Nikoubakht
N.,
Faiz
S.H.,
Mousavie
S.H.,
Shafeinia
A.,
Borhani Zonoz
L.,
Effect of bupivacaine intraperitoneal and intra-abdominal bicarbonate in reducing postoperative pain in laparoscopic cholecystectomy: a double-blind randomized clinical trial study. BMC Research Notes.
2022;
15
(1)
:
191
.
View Article PubMed Google Scholar -
Marks
J.L.,
Ata
B.,
Tulandi
T.,
Systematic review and metaanalysis of intraperitoneal instillation of local anesthetics for reduction of pain after gynecologic laparoscopy. Journal of Minimally Invasive Gynecology.
2012;
19
(5)
:
545-53
.
View Article PubMed Google Scholar -
Marchand
G.,
Ware
K.,
Govindan
M.,
Masoud
A.T.,
King
A.,
Ruther
S.,
A Systematic Review and Meta-Analysis of Intraperitoneal Bupivacaine in Laparoscopic Gynecologic Surgery. Journal of Pain Research.
2021;
14
:
2699-707
.
View Article PubMed Google Scholar -
El-Sherbiny
W.,
Saber
W.,
Askalany
A.N.,
El-Daly
A.,
Sleem
A.A.,
Effect of intra-abdominal instillation of lidocaine during minor laparoscopic procedures. International Journal of Gynaecology and Obstetrics: the Official Organ of the International Federation of Gynaecology and Obstetrics.
2009;
106
(3)
:
213-5
.
View Article PubMed Google Scholar -
Chou
Y.J.,
Ou
Y.C.,
Lan
K.C.,
Jawan
B.,
Chang
S.Y.,
Kung
F.T.,
Preemptive analgesia installation during gynecologic laparoscopy: a randomized trial. Journal of Minimally Invasive Gynecology.
2005;
12
(4)
:
330-5
.
View Article PubMed Google Scholar -
Arden
D.,
Seifert
E.,
Donnellan
N.,
Guido
R.,
Lee
T.,
Mansuria
S.,
Intraperitoneal instillation of bupivacaine for reduction of postoperative pain after laparoscopic hysterectomy: a double-blind randomized controlled trial. Journal of Minimally Invasive Gynecology.
2013;
20
(5)
:
620-6
.
View Article PubMed Google Scholar -
Hachem
L. El,
Small
E.,
Chung
P.,
Moshier
E.L.,
Friedman
K.,
Fenske
S.S.,
Randomized controlled double-blind trial of transversus abdominis plane block versus trocar site infiltration in gynecologic laparoscopy. American journal of obstetrics and gynecology.
2015;
212
(2)
:
182. e1-e9
.
View Article Google Scholar -
Tam
T.,
Harkins
G.,
Wegrzyniak
L.,
Ehrgood
S.,
Kunselman
A.,
Davies
M.,
Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. Journal of Minimally Invasive Gynecology.
2014;
21
(6)
:
1015-21
.
View Article PubMed Google Scholar -
Elkabarity
R.H.,
Ammar
M.,
Zakry
M.R.,
Comparison between ultrasound guided Transversus abdominis plane block and local anesthetic instillation in patients undergoing laparoscopic hysterectomy. Evidence Based Women's Health Journal..
2020;
10
(3)
:
230-8
.
View Article Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 9 (2023)
Page No.: 5934-5941
Published on: 2023-09-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 3905 times
- PDF downloaded - 1150 times
- XML downloaded - 81 times
 Biomedpress
Biomedpress



