Abstract
Introduction: Pelvic venous incompetence (PVI) is the most common chronic pathology, mainly affecting women of different ages. Its characteristic signs include pelvic venous fullness syndrome and chronic pelvic pain, contributing to temporary disability and impaired reproductive function. While there are known surgical treatment methods for pelvic pain in PVI, they have numerous complications.
Case presentation: A 39-year-old female patient presented with PVI and chronic pelvic pain, dysmenorrhea, and infertility. They underwent simultaneous combined reconstructiveplastic conservative surgical treatment under 3D laparoscopic video monitoring.
Conclusion: The patient's treatment outcome was characterized by decreased pelvic pain, normalized menstrual function, and a long-awaited uterine pregnancy ending with the birth of a full-term baby. The two successively performed surgical treatment procedures had a cumulative therapeutic effect, relieving the patient's varicose pelvic pain due to various causes and restoring their reproductive function.
Introduction
Pelvic venous incompetence (PVI) is the most common chronic pathology, mainly affecting women of different ages1. Its characteristic signs include pelvic congestion syndrome and chronic pelvic pain, contributing to temporary disability and impaired reproductive function2. PVI has been shown to reduce life expectancy by an average of 18%, and fatal outcomes are possible without proper treatment3. Its risk factors induce heredity, sex, age, nature of activity, sedentary lifestyle, multiple pregnancies, and bad habits4.
The primary defect in PVI is reflux through failed ovarian valves and pelvic veins2. There are concomitant hemodynamic changes in the veins: increased vessel diameter, slowing of the blood flow, a change in the laminar blood flow in the vessels to turbulent, deterioration of perfusion-metabolic processes, decreased tissue oxygenation, and the vulnerability of the ovaries’ follicular apparatus5, 6. Regardless of the provoking events, prolonged venous dilation causes inflammation, further destroying the valve’s structure and leading to significant reflux3. Endothelial cells, which are the first to encounter free radicals, oxidized low-density lipoproteins, and chemical agents, are known to be the critical link in the chain of reactions in venous wall rearrangement7.Excessive reactive oxygen species production in PVI is caused by pelvic venous dyscirculatory disorders, hypoxemia, and ischemia of organs that accelerate the formation of toxic lipid peroxidation products while reducing their neutralization processes8, 9, 10, 11. Hemodynamic disorders in the ovarian vein basin and activation of lipid peroxidation processes in regional blood flow are factors leading to hypoxia, ovarian dysfunction, reduced ovarian reserve, and infertility12.
Surgical methods are considered among the primary modalities for treating PVI. However, postoperative recurrences reach 80% and constitute today a topical problem of surgical phlebology13, 14, 15, 16, 17, 18. Existing operative treatment methods for pelvic pain in PVI are presacral neurectomy, excision of the uterovaginal ganglion, ovarian sympathectomy, and dissection of sacroiliac ligaments16. The primary objective of all these techniques is to interrupt the flow of afferent pain impulses coming from the female internal genitalia.It should be noted that the above surgical interventions have insufficiently high clinical efficacy (33%–63%) in relieving pelvialgia and are accompanied by serious complications, including a high probability of injury to large blood vessels (middle sacral vein and artery, common iliac vein, and vena cava), lymph vessels, and ureters; and the development of remote complications such as bowel and bladder dysfunction14. Ovarian sympathectomy has a high probability of vascular injury followed by retroperitoneal hematoma formation, development of cystic ovarian remodeling, decreased ovarian reserve due to insufficient blood supply to the ovaries, ovarian insufficiency, and endocrine sterility development19, 20, 21.
Case Presentation
Patient K. was a 39-year-old woman with a six-year history of PVI who was suffering from chronic and recurrent inflammation of the uterine appendages, which manifested as recurrent pelvic pains, especially on the eve of menstruation, dysmenorrhea in the form of uterine bleeding for 5–7 days, and infertility. Periodic conservative treatment with anti-inflammatory, styptic, and analgesic drugs contributed to the short-term relief of the pathological symptomatology and the recurrence of the clinical presentation of the disease.
Outpatient ultrasonic angioscans with Dopplerometry revealed pelvic varicose veins of 7–10 mm and a blood flow velocity in the vessels of the venous plexuses of the uterine appendixes of 5.0 ± 2.3 cm/s; when the Valsalva test with pressure was performed, a marked decrease in blood flow velocity, up to retrograde, was observed, indicating valve insufficiency.
Conservative complex treatment was prescribed, including long-term (12-month) courses of phlebotropic and antiplatelet drugs. Despite relief from varicose veins symptoms and disease remission within eight months after therapy started, dynamic ultrasound monitoring of the venous system indicated PVI progression.
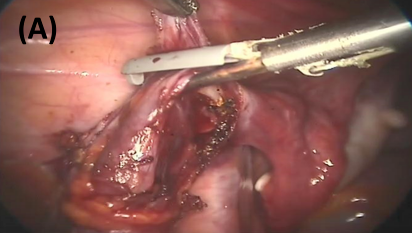
Laparoscopy was performed in two stages22 Figure 1. In the first stage, a combined laparoscopic examination was performed using a retrograde hemodynamic test, allowing for reliable topical diagnostics with a video recording of varicose veins in the pelvic basin and subsequent maximum possible removal of varicose foci.
This task was accomplished by using soft endoscopic clamps to mobilize the distal and proximal sections of varicose veins, and blood was evacuated with a thin needle (26–28 G) from a limited vascular lumen. Then, a foam form of a sclerosant solution was injected into the “dry” lumen of the vein in a volume equal to the previously removed blood volume. The treated vascular venous lumen was exposed to the sclerosant for 180 seconds, which was sufficient to irreversibly destroy endothelial cells in the treated vascular zone.
In the second stage, a denervating laparoscopic operation was performed, which included the thermal destruction of nerve fibers in the sacro-uterine ligaments within a limited area of 3 mm, equal to the width of the working part of the thermal clamps. The thermal exposure interrupted the flow of afferent pain impulses from the internal genitals to the submandibular plexus.
The effectiveness of the operation was evaluated according to duplex ultrasound scanning, which indicated the absence of reverse venous flow and organ stagnant venous fullness in the internal genitals. Another criterion for evaluating the effectiveness of combined laparoscopic treatment of varicose pelvic pain was the use of a visual analog scale (VAS), which grades pain from 0 (no pain) to 10 (unbearable pain), and the quality of life index, an integral indicator that reliably reflects a patient’s clinical condition and allows assessing the negative impact pain has on certain aspects of everyday life (general activity, mood, relationships with other people, ability to take walks, performance, sleep patterns, and overall well-being) in the long-term postoperative period19, 23.
The patient’s treatment outcome was characterized by decreased pelvic pain from 8–10 points to 2–4 (on the VAS scale), normalization of menstrual function during three years of follow-up, and a long-awaited uterine pregnancy ending with the birth of a full-term baby.
Discussion and Conclusion
The proposed method could be used to treat varicose chronic pelvic pain in women of any age. Surgical methods for treating chronic pelvic pain caused by PVI in women exist, but they are characterized by insufficiently high clinical efficacy and serious complications. Therefore, open extraperitoneal resection of gonadal veins provides an insufficiently high percentage of relief from varicose pelvic pain (73.3%), which in the postoperative period is accompanied by significant intraperitoneal pain syndrome, pain in the postoperative suture area, wound infection complications, and low cosmetic effects14, 24, 25.
Laparoscopic transperitoneal resection of gonadal veins is a minimally invasive operation. The negative aspects of this operation are: high traumatism in the abdominal cavity from the surgical techniques with a risk of damage to organs and tissues—with the allocation of gonadal veins for ≥10 cm in the right and left iliac regions, with an additional allocation of the sigmoid and blind sections of the large intestine, and postoperative intestinal paresis14, 15, 25.
Transposition of the left renal vein serves as an approach to eliminate compression of the left renal vein by the superior mesenteric artery—the “nutcracker” syndrome. The operation is performed by laparotomic or laparoscopic access, forming a new renocaval venous junction. This surgical intervention is traumatic and risks serious complications, such as ischemic kidney damage, venous anastomosis, thrombosis, bleeding, and wound infection26, 27.
Gonadal-ileocecal bypass surgery is used to eliminate left-sided reno-ovarian hypertension due to mesaortic compression of the left renal vein. There are unidirectional and bidirectional gonadal-iliac anastamoses. The hemodynamic basis of the operation is the redistribution of blood flow from the left renal and gonadal veins to the left common iliac vein. Despite the positive effect of these surgical interventions on reno-ovarian hemodynamics, this surgical intervention carries high risks of bleeding and traumatization of the kidney, ovary, and main veins and wound infection16, 17, 18.
Endovascular embolization of gonadal veins with metal spirals and balloon angioplasty reduces blood flow through these vessels by placing intravenous occluders in them. The quality of the operation results in relief of varicose pelvic pain is about 60%–86%, with a possibility of increased pain syndrome after the intervention in 10% of patients. The negative consequences of endovascular occlusion of the gonadal veins are the migration of occluders into the pulmonary arterial bed (in 4% of cases) and the protrusion of the occluder through the vessel wall. In addition, this method is contraindicated when the gonadal veins expand >8 mm and when patients are intolerant of contrast agents14, 26, 28.
The method of endovascular sclerobliteration of gonadal veins is the closest to the proposed method of varicose pelvic pain treatment. However, the experience of using this medical aid is relatively small and has no more than 50 observations. In their work, the authors noted a decrease in pelvic pain in 88% of patients. However, three patients were diagnosed with ovarian vein thrombophlebitis29.
The basis of this operation is catheterizing the gonadal veins by introducing a liquid or foam form of a phlebosclerosing drug into their lumen. The disadvantage of this technique is the need to use expensive imported angiographic equipment and the presence of an experienced interventional radiologist. This operation was performed after preliminary catheterization of the right femoral vein by Seldinger, followed by catheterization of the inferior vena cava and left renal veins, after which superselective catheterization of the left ovarian vein was performed. Similarly, catheterization of the right ovarian vein was conducted, which is entered directly from the inferior vena cava.
The technical result of the proposed method for treating the patient was the complete topical diagnosis of all varicose veins in the pelvic basin, which is achieved by the simultaneous use of a retrograde hemodynamic test with a 3D video recording of varicose foci, followed by obliteration of all diagnosed varicose veins using a foam form of sclerosant, eliminating the possibility of damage to nearby intact veins. Injection sclerotherapy includes sclerobliteration of multiple varicose trunks, additional collateral branches, and satellite veins of ovarian and uterine veins, contributing to the restoration of full functional activity of the internal reproductive organs of a woman and reducing the number of relapses in the long term (3–5 years) postoperative period.
Therefore, consistently performed therapeutic procedures of this surgical treatment have a cumulative therapeutic effect, relieving the patient’s varicose pelvic pain due to various causes and restoring their reproductive function. The patient’s treatment outcome was characterized by decreased pelvic pain, normalization of menstrual function, and a long-awaited uterine pregnancy ending with the birth of a full-term baby.
Abbreviations
PVI: pelvic venous incompetence; VAS: visual analog scale
Acknowledgments
None.
Author’s contributions
Research concept and design: Andrey A. Semendyaev, Dmitriy A. Stupin; Collection and processing of material: Dmitriy A. Stupin, Andrey A. Semendyaev, Konstantin V. Pesterev; Text writing: Marina A. Darenskaya, Andrey A. Semendyaev, Sergey I. Kolesnikov; Editing: Sergey I. Kolesnikov, Lyubov I. Kolesnikova; Approval of the final version of the article: Sergey I. Kolesnikov, Lyubov I. Kolesnikova. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study, and a participant provided written informed consent.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
References
-
Khilnani
N.M.,
Meissner
M.H.,
Learman
L.A.,
Gibson
K.D.,
Daniels
J.P.,
Winokur
R.S.,
Research Priorities in Pelvic Venous Disorders in Women: Recommendations from a Multidisciplinary Research Consensus Panel. Journal of Vascular and Interventional Radiology.
2019;
30
(6)
:
781-9
.
View Article PubMed Google Scholar -
Riding
D.M.,
Hansrani
V.,
McCollum
C.,
Pelvic vein incompetence: clinical perspectives. Vascular Health and Risk Management.
2017;
13
:
439-47
.
View Article PubMed Google Scholar -
Barge
T.F.,
Uberoi
R.,
Symptomatic pelvic venous insufficiency: a review of the current controversies in pathophysiology, diagnosis, and management. Clinical Radiology.
2022;
77
(6)
:
409-17
.
View Article PubMed Google Scholar -
Khilnani
N.M.,
Winokur
R.S.,
Scherer
K.L.,
Meissner
M.H.,
Clinical presentation and evaluation of pelvic venous disorders in women. Techniques in Vascular and Interventional Radiology.
2021;
24
(1)
:
100730
.
View Article PubMed Google Scholar -
Darenskaya
M.A.,
Stupin
D.A.,
Semendyaev
A.A.,
Comparative analysis of lipid peroxidation in peripheral and regional blood flows in women with primary varicose veins of the small pelvis. Klinichescheskaya Laboratornaya Diagnostika.
2022;
67
(7)
:
374-80
.
View Article PubMed Google Scholar -
Darenskaya
M.,
Stupin
D.,
Semendyaev
A.,
Kolesnikov
S.,
Shcherbatykh
A.,
Tolkachev
K.,
Pelvic venous insufficiency: lipid peroxidation levels in ovarian venous blood. Biomedical Research and Therapy.
2022;
9
(2)
:
4884-91
.
View Article Google Scholar -
Bendek
B.,
Afuape
N.,
Banks
E.,
Desai
N.A.,
Comprehensive review of pelvic congestion syndrome: causes, symptoms, treatment options. Current Opinion in Obstetrics & Gynecology.
2020;
32
(4)
:
237-42
.
View Article PubMed Google Scholar -
Kolesnikova
L.I.,
Darenskaja
M.A.,
Kolesnikov
S.I.,
Free radical oxidation: a pathophysiologist's view. Bjulleten' sibirskoj mediciny.
2017;
16
(4)
:
16-29
.
View Article Google Scholar -
Kolesnikova
L.I.,
Semendyaev
A.A.,
Stupin
D.A.,
Darenskaya
M.A.,
Grebenkina
L.A.,
Natyaganova
L.V.,
The intensity of lipid peroxidation processes in women with primary varicose veins of the pelvic depending on the stage of the disease. Annals of the Russian Academy of Medical Science..
2018;
73
(4)
:
229-35
.
View Article Google Scholar -
Darenskaya
M.A.,
Semendyaev
A.A.,
Stupin
D.A.,
Grebenkina
L.A.,
Danusevich
I.N.,
Kolesnikova
L.I.,
Activity of antioxidant enzymes in the regional blood flow during pelvic venous disorders in women. Bulletin of Experimental Biology and Medicine.
2020;
169
(6)
:
747-50
.
View Article PubMed Google Scholar -
Darenskaya
M.A.,
Stupin
D.A.,
Semendyaev
A.A.,
Kolesnikov
S.I.,
Semenova
N.V.,
Kolesnikova
L.I.,
Cytokine profile and oxidative stress parameters in women with initial manifestations of pelvic venous insufficiency. AIMS Medical Science.
2022;
9
(3)
:
414-23
.
View Article Google Scholar -
Kolesnikova
L.I.,
Gus
A.I.,
Taranenko
A.V.,
Informativeness of estimating CD34 expression in the development of pelvic varicose veins in women. Obstetrics and gynecology / Akusherstvo y ginekologiya (Moscow).
2019;
2019
(2)
:
120-125
.
View Article Google Scholar -
Gargiulo
T.,
Mais
V.,
Brokaj
L.,
Cossu
E.,
Melis
G.B.,
Bilateral laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndrome. The Journal of the American Association of Gynecologic Laparoscopists.
2003;
10
(4)
:
501-4
.
View Article PubMed Google Scholar -
Kirienko
A.I.,
Gavrilov
S.G.,
Yanina
A.M.,
Evaluation of the effectiveness of surgical methods for the treatment of pelvic venous plethora. Flebologiya..
2016;
10
(1)
:
44-9
.
View Article Google Scholar -
Rogers
A.,
Beech
A.,
Braithwaite
B.,
Transperitoneal laparoscopic left gonadal vein ligation can be the right treatment option for pelvic congestion symptoms secondary to nutcracker syndrome. Vascular.
2007;
15
(4)
:
238-40
.
View Article PubMed Google Scholar -
Bredikhin
R.A.,
Ignat'ev
I.M.,
Fomina
E.E.,
Volodiukhin
M.I.,
Gaptravanov
A.G.,
Mikhaĭlov
M.K.,
[Diagnosis and treatment of varicose disease of small pelvic veins]. Angiologiia i Sosudistaia Khirurgiia.
2012;
18
(1)
:
63-9
.
PubMed Google Scholar -
Strachov
S.N.,
Pryadko
S.I.,
Bondar
Z.M.,
Kosyreva
N.B.,
Variants of architectonics, hemodynamics of the left renal and testicular veins and the choice of a pathogenetically substantiated method of surgical treatment of left-sided varicocele. Annals of Surgery (In Russian).
2014;
2014
(3)
:
32-40
.
-
Pryadko
S.I.,
Arakelyan
V.S.,
Malinin
A.A.,
Reconstructive surgery on the renal veins in patients with renal and pelvic plethora. Byulleten’ NCSSKH im A.N. Bakuleva RAMN Serdechno-sosudistye zabolevaniya.
2018;
19
(S6)
:
142
.
-
Savitsky
G.A.,
Ivanova
R.D.,
Shcheglova
I.Y.,
Popov
P.A.,
Surgical treatment of pelvic pain syndrome in gynecological practiceELBI: St. Petersburg; 2000.
Google Scholar -
Linde
V.A.,
Rymashevsky
A.N.,
Kogan
M.I.,
Chronic pelvic painHippocrates: St. Petersburg; 2012.
Google Scholar -
Orlova
O.A.,
Naumovich
E.G.,
Shipovsky
V.N.,
Podzolkova
N.M.,
Method for determining the functional state of the venous system of the small pelvis in women. Patent RF № 2646563; 2018. . Obstetrics and gynecology / Akusherstvo y ginekologiya (Moscow).
2004;
2004
(2)
:
33-40
.
-
Semendyaev
A.A.,
Stupin
D.A.,
Cherepanova
M.A.,
Method for determining the functional state of the venous system of the small pelvis in women. Patent RF № 2646563; 2018. . 2018
.
-
Huskisson
E.C.,
Measurement of pain. Lancet.
1974;
2
(7889)
:
1127-31
.
View Article PubMed Google Scholar -
Rundqvist
E.,
Sandholm
L.E.,
Larsson
G.,
Treatment of pelvic varicosities causing lower abdominal pain with extraperitoneal resection of the left ovarian vein. Annales Chirurgiae et Gynaecologiae.
1984;
73
(6)
:
339-41
.
PubMed Google Scholar -
Gargiulo
T.,
Mais
V.,
Brokaj
L.,
Cossu
E.,
Melis
G.B.,
Bilateral laparoscopic transperitoneal ligation of ovarian veins for treatment of pelvic congestion syndrome. The Journal of the American Association of Gynecologic Laparoscopists.
2003;
10
(4)
:
501-4
.
View Article PubMed Google Scholar -
Scultetus
A.H.,
Villavicencio
J.L.,
The nutcracker syndrome: its role in the pelvic venous disorders. Journal of vascular surgery.
2001;
34
(5)
:
812-9
.
View Article Google Scholar -
Hartung
O.,
Barthelemy
P.,
Berdah
S.V.,
Alimi
Y.S.,
Laparoscopy-assisted left ovarian vein transposition to treat one case of posterior nutcracker syndrome. Annals of Vascular Surgery.
2009;
23
(3)
.
View Article PubMed Google Scholar -
Hamoodi
I.,
Hawthorn
R.,
Moss
J.G.,
Can ovarian vein embolization cause more harm than good?. Journal of Obstetrics and Gynaecology Research.
2015;
41
(12)
:
1995-7
.
View Article PubMed Google Scholar -
Gandini
R.,
Konda
D.,
Abrignani
S.,
Chiocchi
M.,
Da Ros
V.,
Morosetti
D.,
Treatment of symptomatic high-flow female varicoceles with stop-flow foam sclerotherapy. Cardiovascular and Interventional Radiology.
2014;
37
(5)
:
1259-67
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 5 (2023)
Page No.: 5666-5670
Published on: 2023-05-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 3851 times
- PDF downloaded - 1222 times
- XML downloaded - 133 times
 Biomedpress
Biomedpress



