Abstract
Junctional ectopic tachycardia (JET) occurs postoperatively or after catheter ablation in the region of Koch's triangle. The post-ablation incidence of JET reported in the medical literature is very low. We report the case of a 13-year-old female patient who underwent catheter ablation of the slow pathway for atrioventricular node reentrant tachycardia and subsequently developed JET. An accelerated automatic ectopic focus was found in the atrioventricular junction area due to radiofrequency applications. Treatment with metoprolol, ivabradine, propafenone, and amiodarone was ineffective in stopping the arrhythmia. However, JET resolved within 30 days without other antiarrhythmic drugs.
Introduction
Junctional ectopic tachycardia (JET) occurs in children due to increased automatism in two main clinical settings: (1) near the atrioventricular junction in the initial postoperative phase1 and (2) in the region of Koch’s triangle after catheter ablation. It has been associated with ischemia, stretch, and direct damage to the heart’s atrioventricular (AV) conduction tissue during radiofrequency (RF) application. JET appears on a 12-lead electrocardiogram (ECG) as a narrow QRS tachycardia without detectable P waves2. It can be regular or irregular. It is focal, and unlike AV nodal reentry and AV reentry supraventricular arrhythmias, it does not involve a reentry circuit. It might have 1:1 retrograde atrial conduction or AV dissociation.
The post-ablation incidence of symptomatic JET reported in the medical literature is very low (3 cases per 37,541 [0.008%]) and is reported exclusively in pediatric patients3.
We report the case of a 13-year-old female patient who underwent catheter ablation of the slow pathway for atrioventricular node reentrant tachycardia (AVNRT) and subsequently developed JET. An accelerated automatic ectopic focus was found in the AV junction area due to RF applications.
Case presentation
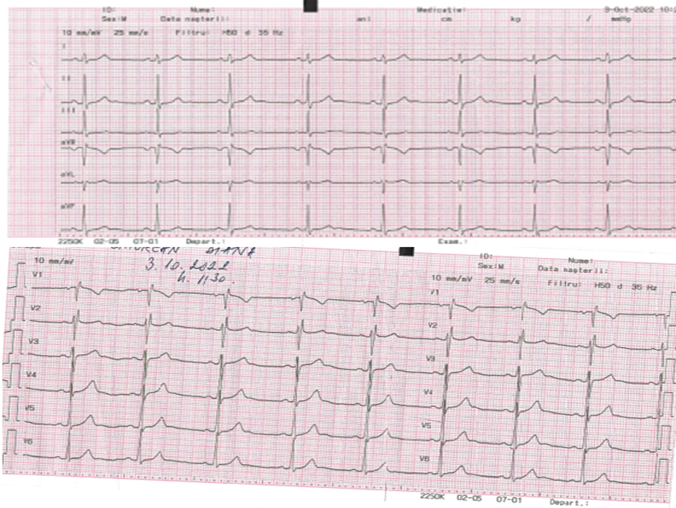
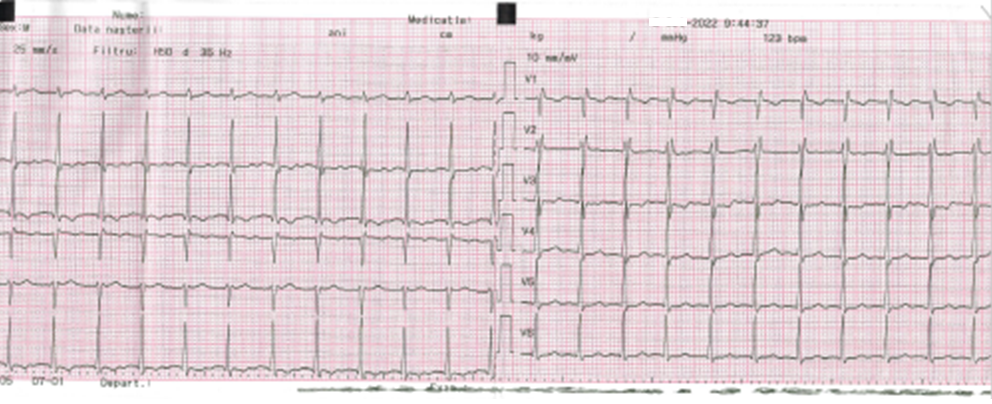
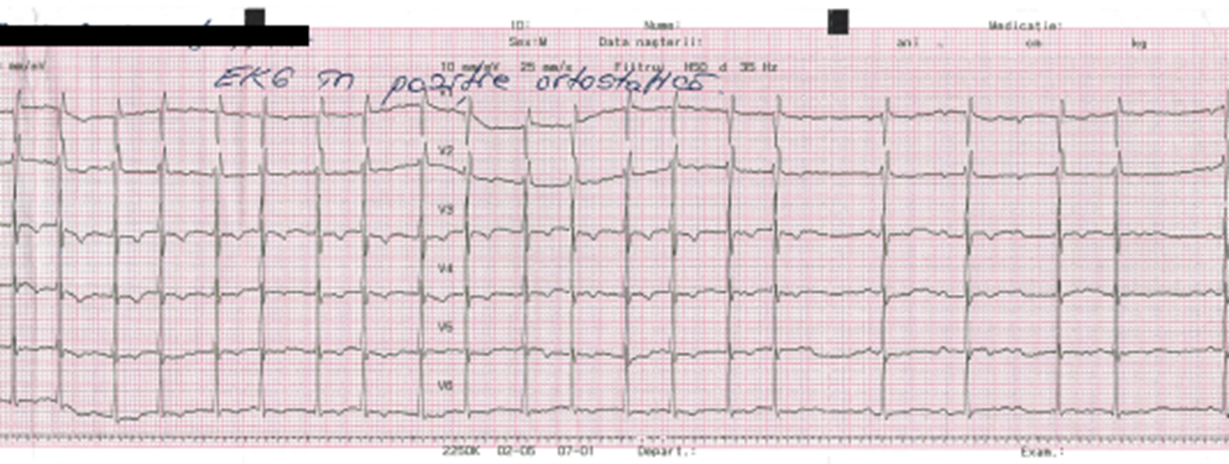
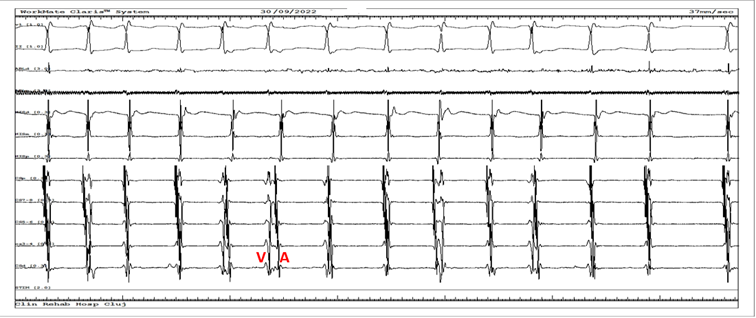
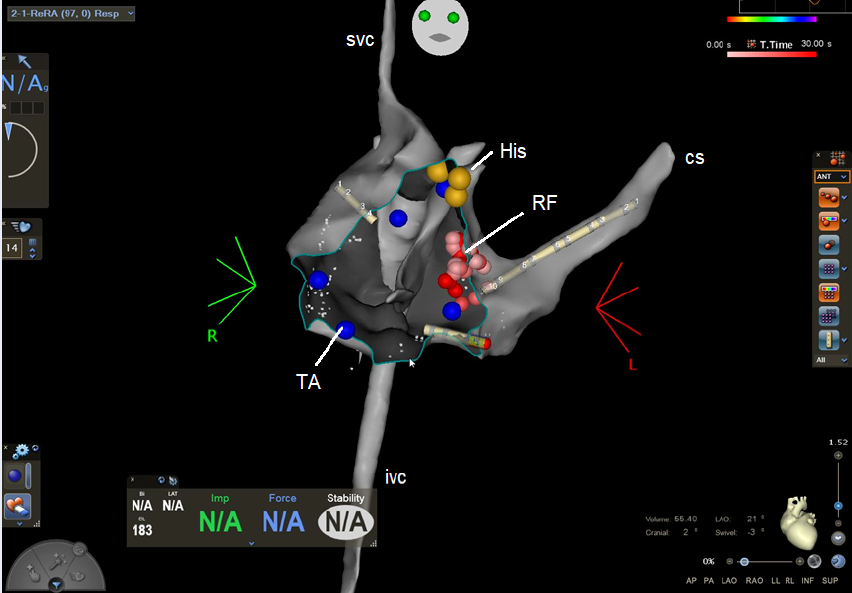
A 13-year-old female patient was admitted to the Cardiology Department for palpitations that started five years ago in 2018. The palpitations had a fast rhythm (190 bpm), regular character, variable duration (5 – 15 minutes) with spontaneous remission, and appeared during effort or rest. In 2022, she had weekly palpitation episodes. At presentation, she had a heart rate of 80 bpm and blood pressure of 120/70 mmHg without any sign of left or right heart failure. Her ECG showed a normal sinus rhythm with a normal PR interval (Figure 1). Her echocardiography was also normal. Due to the recurring nature of the arrhythmia, an electrophysiological study was performed using the Carto 3 Biosense Webster system without X-ray exposure4. An anatomical map of the right atrium was created (Figure 2), and the His bundle was marked. We identified fast and slow nodal pathways, and RF ablated the slow pathway in the posteroseptal area. Due to multiple applications at the slow pathway level (Figure 2) without its complete disappearance, a JET occurred with a heart rate of 125 – 130 bpm. The tachycardia became incessant after more applications to the region. Vagal maneuvers were ineffective in stopping JET. In the first 24 hours post-ablation, the patient received intravenous (i.v.; 10 mg) and oral (100 mg) metoprolol, ivabradine (10 mg), i.v. propafenone (140 mg), and i.v. amiodarone (300 mg). However, her arrhythmia remained incessant (24/24 hours). On the second day, she received amiodarone and metoprolol and experienced short sinus rhythm episodes. On the third day, she stayed 16 hours in sinus rhythm and 8 hours in JET. Before discharge, she performed a stress test stopped at 125 W without any JET episode. She was discharged with amiodarone and metoprolol. After 30 days, both drugs were interrupted without any arrhythmia recurrence.
Discussion and Conclusion
Catheter ablation is a successful therapeutic option for treating AVERT. However, arrhythmic complications such as complete AV block or JET are possible. These are distinct from the junctional rhythm commonly produced during RF applications in the posteroseptal region of Koch’s triangle, which is a sign of success during ablation for AVNRT5.
Another possible AVNRT ablation complication can be impaired conduction through the AV node. Complete AV block is an uncommon AVNRT catheter ablation complication. Most cases are transient and occur during RF application. In this case, AV conduction was temporarily impaired due to edema caused by the RF current in the tissue around the AV node. AV conduction recovers following tissue edema resolution. However, persistent high-degree AV block is believed to result from permanent tissue damage with necrosis caused by the ablation. The AV block mostly occurs in the early phase after ablation. Delayed AV block has been seen in very few cases. Brembilla et al. reported three patients with complete AV block that developed 1–3 days after catheter ablation and further resolved with one-to-one AV conduction. Fenelon et al. described a patient with a delayed Mobitz I second-degree AV block at rest and Mobitz II block during physical activity three months after catheter ablation. Williamson et al. described three cases of complete AV block developing 36 – 72 hours after catheter ablation. Several studies reported a positive effect of anti-inflammatory drugs in cases with AV block following catheter ablation of the slow pathway. Parwani et al. described a case of third-degree AV block that occurred three days after catheter ablation, which was further treated with i.v. prednisolone (250 mg) continued with oral prednisone and ibuprofen (600 mg) daily. At the 12-month follow-up, they described a normal PR interval during a 24-hour Holter ECG. Hoshiyama et al. described a case of complete AV block after catheter ablation of the slow pathway. Their patient was treated with colchicine (1 mg/kg) with complete resolution of the AV block after seven days.
In JET, increased automaticity is believed to be the primary cause of arrhythmia5. Other mechanisms were also implicated, such as triggered activity, calcium overload, and increased inflammation with high tumor necrosis factor-alpha and interleukin 1-beta levels6. JET arising post-surgery7 and post-ablation may have a similar mechanism since RF applications in the region of Koch’s triangle may cause localized micro-hemorrhages and coagulation necrosis, similar to those produced during surgery or electrocauterization8. In addition, Zahn et al. and Thibault et al. showed through experimental studies that introducing ice or warm water into the region of Koch’s triangle near its anteriormost point induced an active junctional rhythm9, 10, 11.
While 37,541 AVNRT ablation cases have been examined in the literature3, only three occurrences of JET, all in pediatric patients, were documented, providing a reported incidence of 0.008%. These three patients required therapeutic intervention (medication or repeat ablation), which is likely why they were explicitly mentioned. It is conceivable that transitory JET forms that disappear soon after ablation go unreported.
The medical literature contains limited information about JET. In most instances, JET appears to cease within days following catheter ablation for AVNRT. Nevertheless, its brief duration renders it of minimal clinical significance. However, medical therapy should be recommended when JET persists for several hours over several days and is associated with symptoms. JET is treated using beta blockers, flecainide, and anti-inflammatory drugs, including steroids. When symptoms persist after drug administration, the junctional region may be re-ablated. Since cryoablation requires a gentler energy type from the tissue necrosis perspective and greater lesion reversibility when not using extremely low temperatures, it remains the treatment of choice for JET resistant to antiarrhythmic drugs12.
AVNRT alternately using two slow pathways cannot be excluded in Figure 3, Figure 4, Figure 5 since the ECG shows consecutive short and long cycles with constant cycle lengths. However, this tachycardia began and terminated spontaneously, was repetitive, and lasted seconds to minutes.
Abbreviations
AVNRT: atrio-ventricular node reentrant tachycardia, JET: junctional ectopic tachycardia.
Acknowledgments
None.
Author’s contributions
All author equally contributed to this work. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The data used and analyzed during the case report are available from the corresponding author upon reasonable request.
Ethics approval and consent to participate
Informed written consent was obtained from the patient’s mother to publish this case report and any accompanying medical images.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Catton
K.G.,
Peterson
J.K.,
Junctional Ectopic Tachycardia: Recognition and Modern Management Strategies. Critical Care Nurse.
2020;
40
(1)
:
46-55
.
View Article PubMed Google Scholar -
Alasti
M.,
Mirzaee
S.,
Machado
C.,
Healy
S.,
Bittinger
L.,
Adam
D.,
Junctional ectopic tachycardia (JET). Journal of Arrhythmia.
2020;
36
(5)
:
837-44
.
View Article PubMed Google Scholar -
Liu
C.F.,
Ip
J.E.,
Lin
A.C.,
Lerman
B.B.,
Mechanistic heterogeneity of junctional ectopic tachycardia in adults. Pacing and Clinical Electrophysiology.
2013;
36
(1)
:
e7-10
.
View Article PubMed Google Scholar -
Cismaru
G.,
Muresan
L.,
Puiu
M.,
Rosu
R.,
Gusetu
G.,
Pop
D.,
Ablation of a left-sided accessory pathway with near-zero fluoroscopy in a 9-year-old boy. Oxford Medical Case Reports.
2017;
2017
(9)
:
omx052
.
View Article PubMed Google Scholar -
Poret
P.,
Leclercq
C.,
Gras
D.,
Mansour
H.,
Fauchier
L.,
Daubert
C.,
Junctional rhythm during slow pathway radiofrequency ablation in patients with atrioventricular nodal reentrant tachycardia: beat-to-beat analysis and its prognostic value in relation to electrophysiologic and anatomic parameters. Journal of Cardiovascular Electrophysiology.
2000;
11
(4)
:
405-12
.
View Article PubMed Google Scholar -
Zahn
A.,
Experimenielle Uniersuchungen ijber Reizbildung und reizleitung im atrioventricularknoten. Pflüger, Arch..
1913;
151
(151)
:
247-78
.
View Article Google Scholar -
Thibault
B.,
De Bakker JMT. Hocini M. Loh P. Wittkampf FHM. Janse MJ: origin of heat-indticed accelerated junctional rhythm. Journal of Cardiovascular Electrophysiology.
1998;
9
:
631-41
.
View Article PubMed Google Scholar -
Ruder
M.A.,
Davis
J.C.,
Eldar
M.,
Abbott
J.A.,
Griffin
J.C.,
Seger
J.J.,
Clinical and electrophysiologic characterization of automatic junctional tachycardia in adults. Circulation.
1986;
73
(5)
:
930-7
.
View Article PubMed Google Scholar -
Sasikumar
N.,
Kumar
R.K.,
Balaji
S.,
Diagnosis and management of junctional ectopic tachycardia in children. Annals of Pediatric Cardiology.
2021;
14
(3)
:
372-81
.
View Article PubMed Google Scholar -
Huang
S.K.,
Bharati
S.,
Graham
A.R.,
Lev
M.,
Marcus
F.I.,
Odell
R.C.,
Closed chest catheter desiccation of the atrioventricular junction using radiofrequency energy - a new method of catheter ablation. Journal of the American College of Cardiology.
1987;
9
(2)
:
349-58
.
View Article PubMed Google Scholar -
Kusterer
N.,
Morales
G.,
Butt
M.,
Darrat
Y.,
Parrott
K.,
Ogunbayo
G.,
Junctional ectopic rhythm after AVNRT ablation: an underrecognized complication. Pacing and Clinical Electrophysiology.
2018;
41
(2)
:
182-93
.
View Article PubMed Google Scholar -
Garson
A.,
Gillette
P.C.,
Junctional ectopic tachycardia in children: electrocardiography, electrophysiology and pharmacologic response. The American Journal of Cardiology.
1979;
44
(2)
:
298-302
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 2 (2023)
Page No.: 5545-5549
Published on: 2023-02-28
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4013 times
- PDF downloaded - 1575 times
- XML downloaded - 84 times
 Biomedpress
Biomedpress