Abstract
Introduction: The physical and chemical properties and biological effects of ozone that determine bactericidal, anti-inflammatory, antioxidant and immunocorrective effects are a direct prerequisite for the use of ozone therapy in the postoperative period of treatment of oral leukoplakia. This study aimed to establish the effectiveness of the combined use of cryosurgery and local ozone therapy in the complex treatment of patients with oral mucosa leukoplakia.
Methods: Thirty-three patients (14 men and 19 women) with oral mucosa leukoplakia (verrucose form) aged 30 to 75 years old were examined. Cryodestruction of the lesion was carried out with liquid nitrogen using autonomous cryoapplicators made of porous titanium nickelide. After the treatment, all patients, depending on the type of postoperative treatment, were divided into 2 groups. In the main group, ozonated olive oil was additionally used by applying it to the mucous membrane around the focus of destruction. Patients in the comparison group were prescribed traditional anti-inflammatory treatment. A score assessment of clinical signs (pain syndrome, mucous membrane condition in the surgery area, nature of the wound discharge, and epithelization degree) at different stages of the postoperative period was performed. An enzyme immunoassay was used to assess the activity of superoxide dismutase.
Results: In the main group, on the background of ozone therapy, there was a statistically significant decrease in the intensity of pain syndrome compared to the comparison group at all stages of the postoperative period: on the 5th day, this indicator was half as much as in the comparison group, and on the 14th day, pain completely disappeared (p < 0.05). Analysis of the state of the mucosa around the operative intervention area, as well as characteristics of the surrounding tissue edema, also confirmed a significant reduction in indicators against the comparison group at all stages of postoperative intervention, with complete recovery on the 14th day (p < 0.05). The highest rates of wound surface cleanup, granulation and epithelization were seen in the main group, with favorable ozone exposure on the 10th day relative to the data of the initial period. A significant difference relative to the comparison group was registered on the 7th, 10th and 14th day. It was revealed that the activity of salivary superoxide dismutase (SOD) showed a statistically significant increase from the first day in the patients of the main group, which remained on the 10th day, while the maximum SOD activity was registered on the 5th day after the surgery. The main group patients showed increased SOD activity at all stages of the study as compared to the comparison group (p < 0.05).
Conclusion: The study showed that patients with verrucous leukoplakia of the oral mucosa were more effectively treated using postoperative cryotherapy management alongside local ozone therapy.
Introduction
Leukoplakia is considered a fairly common pathology of the oral mucosa, and in 20-30% of cases, tends towards malignant degeneration1. Currently, it is considered as a multifactorial disease, but it is believed that smoking and alcohol are the most common factors in the development of leukoplakia2. There are 3 main forms of leukoplakia: flat, verrucous, and erosive. The verrucous form (characterized by whitish plaques protruding on the surface) is more prone to the process of malignant progression1.
Due to frequent and possible malignant change, the question of adequate treatment of oral mucosal leukoplakia is extremely urgent in dentistry. The effectiveness of care for these patients is determined by the timeliness and accuracy of diagnosis, with subsequent selection of an optimal treatment. Treatment choices depend on the features and duration of the pathology, the patient immune status, the local microflora, the intensity of the damaging factors, and the effectiveness of the ongoing conservative treatment3. Unfortunately, therapeutic methods do not always lead to complete structural and functional restoration of the oral mucosa4. When the disease is prolonged or recurrent, and complications are present, surgical treatment is the only method to treat leukoplakia.
Surgical treatment may include traditional surgery or laser ablation, electrocautery, or cryosurgery5. Leukoplakia recurrence after surgical treatment has been reported in more than 10% of cases6. Surgical removal of leukoplakia does not reduce the risk of subsequent malignant transformation, but allows a complete histopathological examination of the lesion. Surgical treatment is characterized by the development of a wound, the course and outcome of which depend on the type and severity of injury7. In this regard, there is a necessity to use particularly sparing methods. Local cryosurgery is pathogenetically justified and allows for risk reduction regarding malignant change while stimulating epithelization, all without formation of coarse scars8, 9, 10. By destroying nerve endings in the focus of cryo-exposure and reducing their sensitivity, a persistent analgesic effect is ensured, which excludes the need for anesthesia11.
Postoperative treatment should be aimed at arresting the inflammatory reaction, preventing secondary infection, and stimulating regeneration processes. Medical ozone is an ozone-oxygen mixture produced from ultrapure oxygen, either by its decomposition in a weak electric discharge or by ultraviolet irradiation12. The biological effect of ozone on the organism is provided indirectly through the formation of "ozonides" — compounds of ozone with organic substances that contain double bonds: amino acids, polyunsaturated fatty acids (PUFAs), nicotinamide enzyme, etc.13. It has been found that the peroxides formed when ozone interacts with PUFAs activate the antioxidant defense system (AOD), which improves the patient's immune status14. The physical and chemical properties and biological effects of ozone that determine bactericidal, anti-inflammatory, antioxidant and immunocorrective effects are a direct prerequisite for the use of ozone therapy in the postoperative period of oral leukoplakia13.
The aim of the study was to establish the effectiveness of the combined use of cryosurgery and local ozone therapy in the complex treatment of patients with oral mucosa leukoplakia.
Methods
Study Design
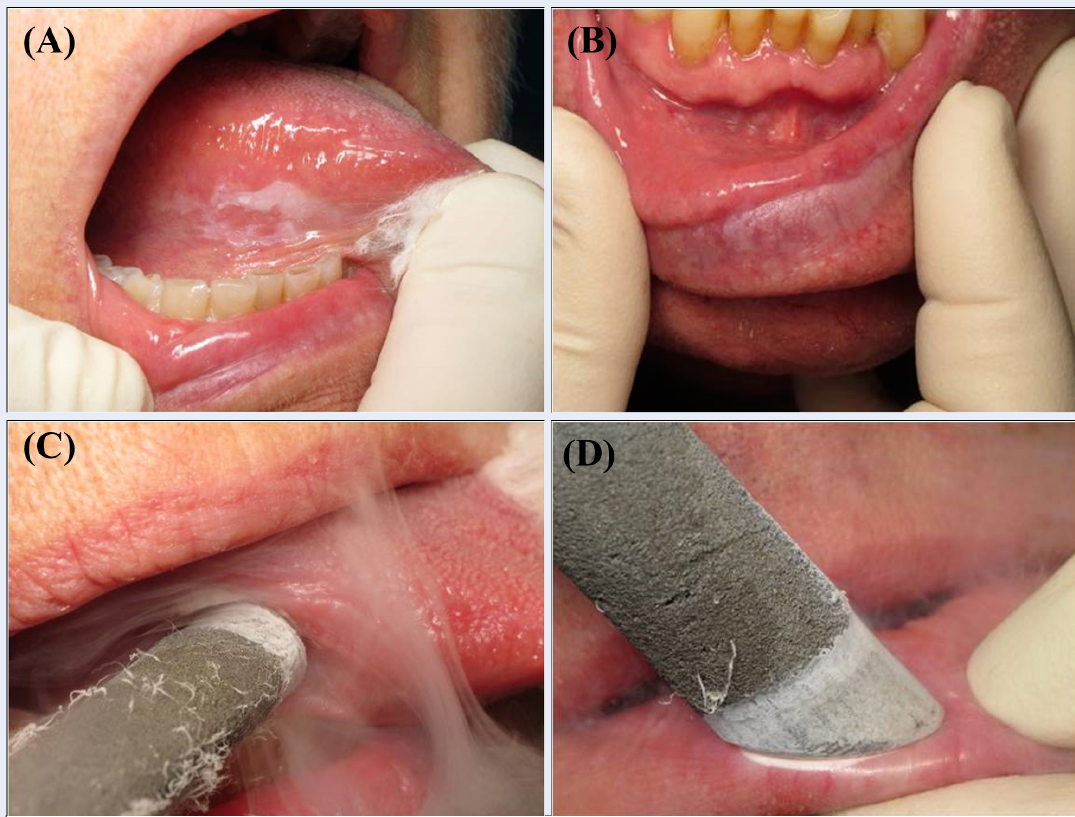
Thirty-three patients (14 men and 19 women) with oral mucosal leukoplakia (verrucous form) aged 30 to 75 years old were examined. The diagnosis was made by an oncologist on the basis of external examination (limited plaques protruding over the surrounding mucosa; grayish-white, irregularly shaped and with a rough surface not removable by scraping with an instrument) and histological findings. The verrucous form occurred most frequently in the age group 50-59 years (53% of patients), in contrast to the age groups 30-39 years (13%), 40-49 years (18%), and 60 and over (16%). Clinical pictures depended on the localization of lesions in the oral mucosa: cheek area (55% of patients), lateral surface of the tongue (6%), cheek area and alveolar process (12%), alveolar process (12%), retromolar process (9%), and floor of the mouth (6%). Cryodestruction of the lesion was undertaken with liquid nitrogen, using autonomous cryoapplicators made of porous titanium nickelide over 90 seconds (Figure 1)15.
After treatment, all patients, depending on the type of postoperative treatment, were divided into 2 groups: the main group and comparison group. Patients in the main group were treated with standardized ozonated olive oil for 15 minutes after cryodestruction, with applications then carried out 5 times a day for 7 days. The patients of the comparison group underwent anti-inflammatory treatment. A system of point assessment of clinical signs at stages across the postoperative period (days 3, 5, 7, 10 and 14) was developed to unify the data and for comparative analysis of the effectiveness of the suggested treatment method16.
Pain syndrome evaluation was as follows:
Assessment of the state of the mucous membrane in the operative area was as follows:
Color:
Condition of the wound surface:
Character of wound discharge:
Granulation tissue:
Degree of epithelization:
Scores were calculated both for an individual indication and for the total score.
Biochemical Measurements
The activity of the antioxidant enzyme, superoxide dismutase (SOD), in the oral fluid of patients with leukoplakia was also analyzed. Samples were taken before surgical intervention, 24 hours (1 day) after surgery, on the 3rd day, 5th day, 7th day, and 10th day. Oral fluid was sampled within 5–15 minutes into sterile measuring tubes. An eBioscience reagent kit (Bender MedSystems) was used for highly sensitive quantitative determination (Cu/ZnSOD) by enzyme immunoassay on a Uniplan-PICON enzyme immunoassay analyzer. The principle of the method is based on the interaction of monoclonal antibodies specific to Cu/ZnSOD adsorbed in the wells of the plate with samples in the presence of horseradish peroxidase.
Statistical Procedure
The number of patients available for each group during the study period was limited. To assess the type of distribution of features, the Shapiro-Wilk criterion was used. The values are represented as M ± σ, where M is the sample mean and σ is the sample standard deviation. In cases of normal distribution, the Student's T-test was used to compare the averages. In the case of distributions that do not correspond to the normal law, the nonparametric Mann-Whitney U-test was used. The differences were considered statistically significant at p < 0.05, where p is the probability of a first–kind error when testing the null hypothesis. Data processing and graphical representation were carried out using the computer program Statistica 8.0.
Results
After treatment, in the main group, as early as 3 days after cryodestruction of verrucous leukoplakia lesions, patients noted the disappearance of the pain syndrome. Despite all patients being advised to avoid irritating and hard food in the postoperative period, this was in fact in most cases the cause of intense pain sensations. Pain syndrome averaged 1.00 ± 0.13 points, which was statistically significantly lower than the figure in the study group (1.77 ± 0.11). On the 5th day, the index was 0.56 ± 0.13, which was two times lower than in the comparison group. The same tendency was seen during all periods of observation, and on the 14th day, no pain syndrome was reported in the control group (Table 1).
| Groups | 3 days | 5 days | 7 days | 10 days | 14 days |
|---|---|---|---|---|---|
| Main group (n = 17) | 1.00 ± 0.13* | 0.56 ± 0.13* | 0.13 ± 0.09* | 0.06 ± 0.11* | 0.0 ± 0.0* |
| Comparison group (n = 16) | 1.77 ± 0.11 | 1.06 ± 0.16 | 0.41 ± 0.12 | 0.34 ± 0.13 | 0.13 ± 0.13 |
| Groups | 3 days | 5 days | 7 days | 10 days | 14 days |
|---|---|---|---|---|---|
| Main group (n = 17) | 1.75 ± 0.12* | 0.88 ± 0.16* | 0.50 ± 0.13* | 0.21 ± 0.11* | 0.0 ± 0.0* |
| Comparison group (n = 16) | 2.30 ± 0.17 | 1.65 ± 0.17 | 0.82 ± 0.18 | 0.76 ± 0.13 | 0.0 ± 0.0 |
| Groups | 3 days | 5 days | 7 days | 10 days | 14 days |
|---|---|---|---|---|---|
| Main group (n = 17) | 1.00 ± 0.00 | 1.00 ± 0.00 | 0.68 ± 0.13* | 0.33 ± 0.11* | 0.06 ± 0.06* |
| Comparison group (n = 16) | 1.00 ± 0.00 | 1.00 ± 0.00 | 0.82 ± 0.09 | 0.76 ± 0.13 | 0.18 ± 0.13 |
| Groups | Before surgery | 1 day | 3 days | 5 days | 7 days | 10 days |
|---|---|---|---|---|---|---|
| Main group (n = 17) | 17.6 ± 0.2 | 51.9 ± 0.1 | 59.3 ± 0.1 | 59.6 ± 0.1 | 50.8 ± 0.2 | 49.4 ± 0.1 |
| Comparison group (n = 16) | 17.1 ± 0.2 | 32.1 ± 0.1* | 31.0 ± 0.1* | 41.6 ± 0.1* | 28.7 ± 0.1* | 22.4 ± 0.1* |
Analysis of the mucosa condition around the surgical intervention zone, as well as the characteristics of the surrounding tissue edema, also confirmed the advantages of using ozonized oil after verrucous leukoplakia cryodestruction. On the 3rd to 5th days of follow-up, most patients in the main group showed moderate and mild hyperemia of the mucous membrane around the operative site, with no cyanosis of the wound edges (Figure 2, Figure 3).
The research index on the 3rd day in the main group averaged 1.75 ± 0.12 points, scoring 0.88 ± 0.16 points on the 5th day. That score was statistically significantly lower than in the same period of observation in the comparison group (Table 2).
The clinical effectiveness criteria covered wound surface cleansing and the intensity of the processes of wound granulation and epithelization, reflecting the intensity of the regeneration processes. The highest rate of epithelization was noted in the main group. On the 10th day, a full regeneration was registered in the majority of patients: the researched index was 0.33 ± 0.11 points (Figure 4, Figure 5).
In the control group, at the same stage of observation, the degree of epithelization was 0.76 ± 0.13, indicating incomplete epithelization in the majority of patients (Table 3).
The analysis of the dynamics of the total score, assessing all clinical parameters, revealed differences during the wound healing process when using the suggested method. Thus, on the 3rd day, it was 6.12 points in the main group, and was statistically significantly lower than the total index of the comparison group by almost 30%. On the 5th day, the studied index in the main group was also lower than in the comparison group (3.88 and 6.72 points respectively). One week later, there was a significant decrease in the total index in the main group (0.88 points), while in the comparison group it decreased to only 3.88 points. At the next stages of observation, the cumulative index in the main group was close to zero, while in the comparison group, it reached 2.62 points on the 10th day and 0.44 points on the 14th day.
The baseline value of SOD activity in the patients of the two groups was similar on average (Table 4). We found that from the first day, in the main group of patients, there was a significant increase in the salivary SOD activity, which remained on the 10th day. The maximum SOD activity was detected on the 5th day after surgery. At the same time, the comparison group showed a decrease in the activity of SOD at all stages of the study compared to the main group (p < 0.05) (Table 4).
Discussion
Ozone therapy is a type of physiotherapeutic treatment in alternative medicine involving the use of ozone for therapeutic and preventive measures.
According to our data, the use of ozone therapy in the postoperative period allows for the shortest duration of pain syndrome, as well as purification, granulation and epithelization of the wound surface, and improvement of mucous membrane condition in the surgical intervention zone due to the positive effects of ozonated olive oil.
It is now well documented that ozonated oil has prolonged disinfectant and stimulating effects that are achieved through the interaction of ozone with organic components of cells, with the formation of several secondary products such as lipid peroxides and fatty acid ozonides14. Further, topical application of ozonated olive oil leads to a slow release of ozone in tissues and promotes rapid healing of oral mucosa17. It was found that ozonated oil has an antimicrobial effect against multiresistant strains of microorganisms, such as Staphylococcus aureus and Candida fungi13. Moreover, acceleration of regeneration is associated with anti-hypoxic action and the ability to stimulate the production of growth factors, which leads to acceleration of angiogenesis and differentiation of epithelial cells18. The mechanism of the antibacterial action of ozone occurs through the selective destruction of the bacterial cell membrane by single-atomic oxygen. In addition, the ozone molecule has a much smaller size compared to the molecule of any known antiseptic drug and therefore a better penetrating ability, which is a great advantage for acting on oral microorganisms organized into plaque or biofilm16. Cryodestruction, as a serious exposure, causes activation of oxidative stress (OS) in the damaged tissues. The initiation and maintenance of the inflammatory process can be carried out through numerous chemical mediators, among which a great importance is attached to reactive oxygen species (ROS), which, in particular, include superoxide anion, hydroxyl radical, and hydrogen peroxide13. It has been shown that OS in saliva is an etiological and pathophysiological factor of periodontal and oral cavity diseases19. Protection against the damaging effects of ROS in the organism is provided by the combined action of a number of factors limiting their action – namely antioxidant systems, including enzymatic reactions of reactive oxygen metabolites utilization. The occurrence of disorders in this system can lead to an imbalance of pro- and antioxidant processes, an increase in the production of ROS and the manifestation of their toxic effect on tissue structural elements13. OS is manifested by the fact that ROS destroy proteoglycans of periodontal soft tissues as well as collagen type 1 proline chains, significantly changing fibroblast functions (adhesion and proliferation)20. The excessive production of ROS by neutrophils and fibroblasts in periodontal tissues activates NF-κb and triggers a signaling cascade that activates osteoclasts, leading to inflammation21. Besides, ROS cause imbalance in the system of matrix metalloproteinases and their inhibitors, leading to degradation of periodontal tissues22. The greatest importance in the processes of enzymic inactivation of ROS is given to the reactions catalyzed by SOD, glutathione peroxidase, and glutathione reductase. In this vein, SOD is a ubiquitous enzyme involved in oxygen metabolism in cells and protects these cells from direct and indirect free radical damage mediated by reactions of oxygen transformation. SOD catalyzes the recombination reaction of superoxide anions. Blood SOD activity is identical to the function of the enzyme in saliva23. Changes in antioxidant activity and salivary SOD enzyme reflect the state of the oral cavity on treatment24. A reduction in the inflammatory response after therapy resulted in an improved antioxidant profile in gingival fluid and saliva22. Levels of OS in saliva decreased when salivary SOD activity increased25. We observed an increase in oral SOD activity in the postoperative period when using ozonated oil more significantly than the adaptive increase during cryodestruction. Application during the postoperative period in the complex treatment of ozonated olive oil solution causes a decrease in the level of OS in saliva due to the persistent and long-term increase in the activity of salivary SOD. This accelerates the reparation processes, improves the wound healing process, and reduces the healing time of the oral mucosa (confirmed by morphological study) compared to traditional methods of treatment.
Conclusions
The study showed superior results over the course of the disease in patients treated with cryodestruction combined with ozone therapy — the earliest disappearance of pain, reduction of edema, hyperemia, and the onset of complete epithelization. In addition, a persistent increase in superoxide dismutase activity in the oral fluid of patients with leukoplakia was noted, which we postulate may accelerate the processes of wound surface reparation. This indicates a higher effectiveness of the proposed method of postoperative management of cryotherapy in patients with verrucous leukoplakia using local ozone therapy compared to traditional local anti-inflammatory treatment.
Abbreviations
AOD: antioxidant defense, OS: oxidative stress, PUFAs: polyunsaturated fatty acids, SOD: superoxide dismutase
Acknowledgments
None.
Author’s contributions
Marina A. Darenskaya, Svetlana I. Tokmakova, Olga V. Bondarenko: research concept, design, article writing; Kseniia V. Ziablitskaia, Yuliya V. Lunitsyna, Evgeniy V. Mokrenko, Ivan S. Goncharov, Tatyana A. Gaidarova, Oleg V. Klyushnikov, Maria I. Suslikova, Larisa R. Kolesnikova, Kseniia A. Darenskaya, Yulia O. Sinyova: collection of clinical material, statistical data processing, article writing. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Ethical principles were observed in accordance with the Helsinki Declaration of the World Medical Association (1964, ed. 2013)). The institutional review board approved the study, and all participants provided written informed consent. Ethics Committee (Local Committee on Biomedical Ethics of Altai State Medical University (Barnaul, Russia) approved the research (No. 10 dated December 6, 2014).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Bewley
A.F.,
Farwell
D.G.,
Oral leukoplakia and oral cavity squamous cell carcinoma. Clinics in Dermatology.
2017;
35
(5)
:
461-7
.
View Article PubMed Google Scholar -
Deliverska
E.G.,
Petkova
M.,
Management of oral leukoplakia-analysis of the literature. Journal of IMAB-Annual Proceeding Scientific Papers.
2017;
23
(1)
:
1495-504
.
View Article Google Scholar -
Yanik
E.L.,
Katki
H.A.,
Silverberg
M.J.,
Manos
M.M.,
Engels
E.A.,
Chaturvedi
A.K.,
Leukoplakia, Oral Cavity Cancer Risk, and Cancer Survival in the U.S. Elderly. Cancer Prevention Research (Philadelphia, Pa.).
2015;
8
(9)
:
857-63
.
View Article PubMed Google Scholar -
van der Waal
I.,
Oral leukoplakia, the ongoing discussion on definition and terminology. Medicina Oral, Patologia Oral y Cirugia Bucal.
2015;
20
(6)
:
e685-92
.
View Article PubMed Google Scholar -
Al-Hashimi
I.,
lAl-Hashimi. Editorial: Advances in the Diagnosis and Management of Oral Diseases'. The Open Pathology Journal.
2011;
5
(l)
:
l-2
.
View Article Google Scholar -
Kamilov
K.H.,
Kadyrbayeva
A.,
Aripova
D.,
Fazilbekova
A.,
Oral leukoplakia: clinic, diagnosis, treatment. Medicine and innovations.
2021;
1
(2)
:
44-49
.
-
Gandara-Vila
P.,
Pérez-Sayans
M.,
Suárez-Peñaranda
J.M.,
Gallas-Torreira
M.,
Somoza-Martín
J.,
Reboiras-López
M.D.,
Survival study of leukoplakia malignant transformation in a region of northern Spain. Medicina Oral, Patologia Oral y Cirugia Bucal.
2018;
23
(4)
:
e413-20
.
View Article PubMed Google Scholar -
Nogueira
P.T.,
Remigio
M.M.,
de Queiroz
A.M.,
da Silva
A.A.,
Filho
J.R.,
Cryosurgery as an Option for the Treatment of Vascular Lesions of the Oral Cavity. Case Reports in Otolaryngology.
2017;
2017
:
8529016
.
View Article PubMed Google Scholar -
Hwang
M.J.,
Yang
Y.J.,
Lee
Y.P.,
Chiang
C.P.,
Cryotherapy is effective for treatment of oral verrucous hyperplasia - Case report. Journal of Dental Sciences.
2021;
16
(3)
:
1025-6
.
View Article PubMed Google Scholar -
Hassan
S.A.,
Bhateja
S.,
Arora
G.,
Prathyusha
F.,
Cryo surgery in dentistry. IP Journal of Surgery and Allied Sciences..
2020;
2
(3)
:
67-71
.
View Article Google Scholar -
Tamar
B.,
Oral leukoplakia as a precancerous lesion and prevention of its malignization. European journal of biomedical and life sciences.
2019;
3
:
3-6
.
-
Klyushnikova
M.O.,
Klyushnikova
O.N.,
The use of medical ozone in the clinic of therapeutic dentistry. Questions. Hypotheses. Answers: science of the XXI century. Krasnodar. Publisher: Sole proprietor Akelyan NS. 2014;220-242.. 2014
.
-
Stübinger
S.,
Sader
R.,
Filippi
A.,
The use of ozone in dentistry and maxillofacial surgery: a review. Quintessence International.
2006;
37
(5)
:
353-9
.
PubMed Google Scholar -
Guinesi
A.S.,
Andolfatto
C.,
Bonetti Filho
I.,
Cardoso
A.A.,
Passaretti Filho
J.,
Farac
R.V.,
Ozonized oils: a qualitative and quantitative analysis. Brazilian Dental Journal.
2011;
22
(1)
:
37-40
.
View Article PubMed Google Scholar -
Tokmakova
S.I.,
Bondarenko
O.V.,
Ulko
N.V.,
Method of treating oral proliferative verrucous leukoplakia. Patent RU 2564432C1..
.
-
Zyablitskaya
K.V.,
Vorobyova
E.N.,
Tokmakova
S.I.,
Sharlaeva
E.A.,
Sokolova
G.G.,
Batanina
I.A.,
Bondarenko
O.V.,
Ozone therapy in complex treatment of leukoplakia of oral mucosa. Medical alphabet.
2018;
2
(339)
:
11-15
.
-
Valacchi
G.,
Lim
Y.,
Belmonte
G.,
Miracco
C.,
Zanardi
I.,
Bocci
V.,
Ozonated sesame oil enhances cutaneous wound healing in SKH1 mice. Wound Repair and Regeneration.
2011;
19
(1)
:
107-15
.
View Article PubMed Google Scholar -
Travagli
V.,
Zanardi
I.,
Valacchi
G.,
Bocci
V.,
Ozone and ozonated oils in skin diseases: a review. Mediators of Inflammation.
2010;
2010
:
610418
.
View Article PubMed Google Scholar -
Dahiya
P.,
Kamal
R.,
Gupta
R.,
Bhardwaj
R.,
Chaudhary
K.,
Kaur
S.,
Reactive oxygen species in periodontitis. Journal of Indian Society of Periodontology.
2013;
17
(4)
:
411-6
.
View Article PubMed Google Scholar -
Rittié
L.,
Monboisse
J.C.,
Gorisse
M.C.,
Gillery
P.,
Malondialdehyde binding to proteins dramatically alters fibroblast functions. Journal of Cellular Physiology.
2002;
191
(2)
:
227-36
.
View Article PubMed Google Scholar -
Cannizzo
E.S.,
Clement
C.C.,
Sahu
R.,
Follo
C.,
Santambrogio
L.,
Oxidative stress, inflamm-aging and immunosenescence. Journal of Proteomics.
2011;
74
(11)
:
2313-23
.
View Article PubMed Google Scholar -
Wang
J.,
Schipper
H.M.,
Velly
A.M.,
Mohit
S.,
Gornitsky
M.,
Salivary biomarkers of oxidative stress: A critical review. Free Radical Biology & Medicine.
2015;
85
:
95-104
.
View Article PubMed Google Scholar -
Novakovic
N.,
Todorovic
T.,
Rakic
M.,
Milinkovic
I.,
Dozic
I.,
Jankovic
S.,
Salivary antioxidants as periodontal biomarkers in evaluation of tissue status and treatment outcome. Journal of Periodontal Research.
2014;
49
(1)
:
129-36
.
View Article PubMed Google Scholar -
Wei
D.,
Zhang
X.L.,
Wang
Y.Z.,
Yang
C.X.,
Chen
G.,
Lipid peroxidation levels, total oxidant status and superoxide dismutase in serum, saliva and gingival crevicular fluid in chronic periodontitis patients before and after periodontal therapy. Australian Dental Journal.
2010;
55
(1)
:
70-8
.
View Article PubMed Google Scholar -
Silva
P.V.,
Troiano
J.A.,
Nakamune
A.C.,
Pessan
J.P.,
Antoniali
C.,
Increased activity of the antioxidants systems modulate the oxidative stress in saliva of toddlers with early childhood caries. Archives of Oral Biology.
2016;
70
:
62-6
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 10 No 1 (2023)
Page No.: 5491-5499
Published on: 2023-01-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4777 times
- PDF downloaded - 1254 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress






