Abstract
Recurrent respiratory papillomatosis is a chronic disease caused by the human papillomavirus and can affect both children and adults. Although it is a benign disease, papilloma growth can cause severe, sometimes life-threatening airway obstruction. We report the case of a 28-year-old male patient who was admitted to the hospital with a fever and prolonged cough. A computed tomography (CT) scan showed solid and cavitated nodules in his right lung and solid nodules on his vocal cords. Bronchoscopy demonstrated polypoid lesions on his vocal cords. Histopathological study of the lesions confirmed a diagnosis of respiratory papillomatosis.
Introduction
Airway papillomatosis is caused by the human papillomavirus (HPV), of which subtypes 6 and 11 account for the highest rates of disease1. Airway papillomatosis is characterized by the proliferation of benign squamous papillae in the respiratory tract2. Papillomas can develop at any site in the airway but are most common in the larynx and vocal cords, with rare diffuse involvement in the lungs. Incidence rates vary widely across countries; in the United States, 4.3 per 100,000 infants and 1.8 per 100,000 adults are affected3. Disease onset can begin in childhood due to maternal genital HPV infection or adulthood after sexual intercourse. Prognosis varies with age of onset, but the disease tend to be more severe and has a higher recurrence rate in children than adults1.
Currently, there is no cure for airway papillomatosis4. Surgery is the most important treatment modality because it limits disease progression and preserves normal anatomical structure. Other treatment methods include photoangiolytic laser therapy, HPV vaccines, photodynamic therapy, and targeted therapy. The treatment chosen depends on many factors, such as the size, number, and location of papillae; the extent of disease spread; and the age and general condition of the patient.
Case report
A 28-year-old male presented to the hospital with a fever and persistent cough. The patient had a history of general health, with dysphonia since childhood. He had been experiencing a productive cough with hemoptysis for one month and a fever for two days. At the time of admission, the patient’s vital signs were stable (heart rate: 72 BPM, blood pressure: 120/70 mmHg, temperature: 38°C [low-grade fever]). The patient was not anemic and had no dyspnea, enlarged lymph nodes, subcutaneous bleeding, abdominal pain, or jaundice. The patient’s abdomen was soft with no enlargement of the liver or spleen. Pulmonary examination revealed dysphonia, symmetric chest movement with breathing, and reduced apical alveolar murmur with faint rales on percussion. No other abnormalities were detected. Further, the patient had never been infected with COVID-19 and was unvaccinated.
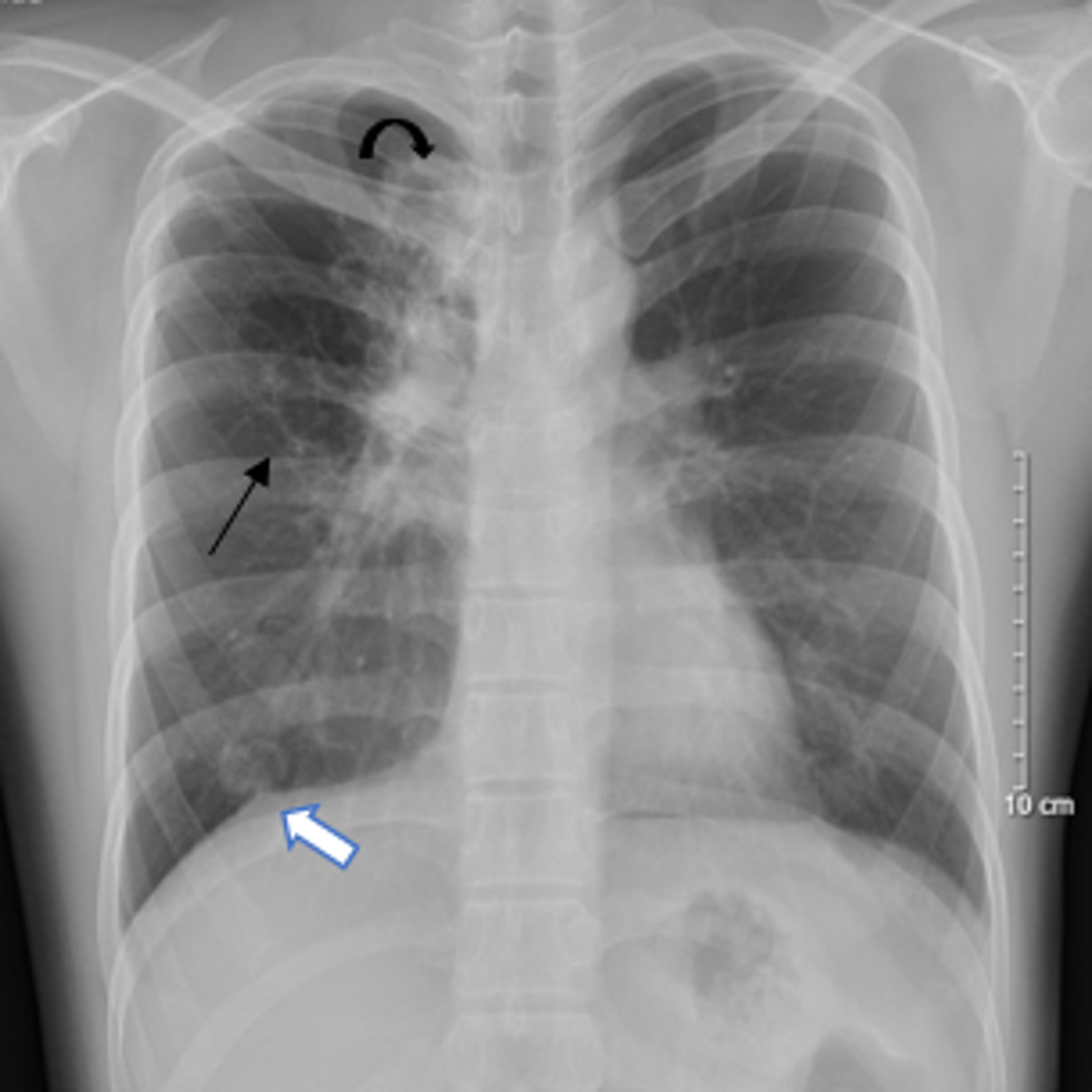
Blood and biochemical tests showed inflammation with a white blood cell count of 10.14 g/L (normal range: 4 – 10 g/L), neutrophil content of 76.4% (normal range: 40 — 60%), and high-sensitivity C-reactive protein concentration of 19.17 mg/dL (normal range: < 10 mg/dL). Liver enzymes were slightly elevated (aspartate transaminase: 86 U/L [normal range: 8 – 33 U/L]; alanine transaminase: 128 U/L [normal range: 8 – 40 U/L]). Total urinalysis showed no abnormalities. Chest radiographs revealed opacities with unclear boundaries in the apex and base of the right lung and a large air cyst measuring 39 mm x 51 mm in the upper lobe (Figure 1). The left lung field was evenly lit. The mediastinum was balanced.
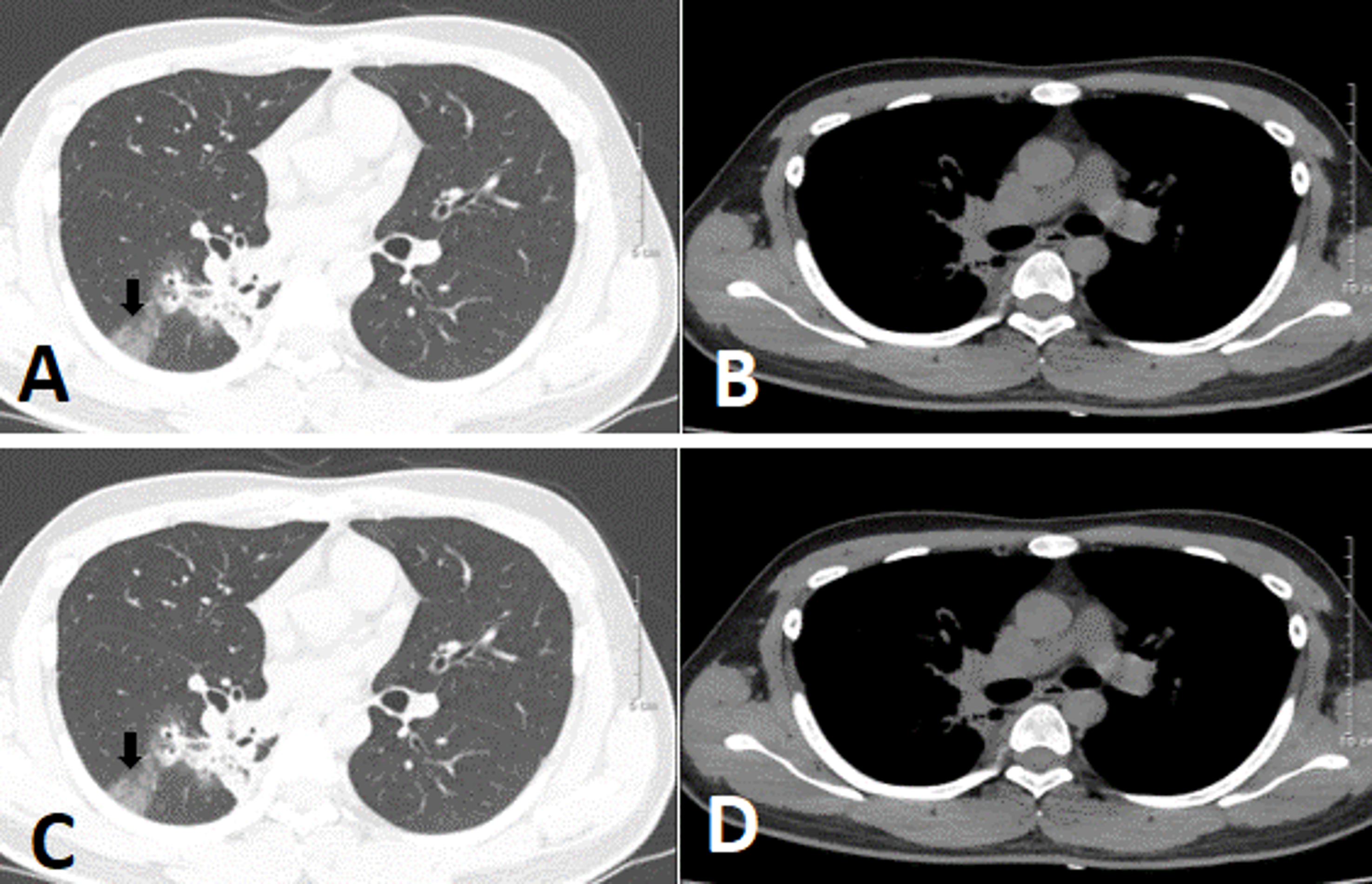
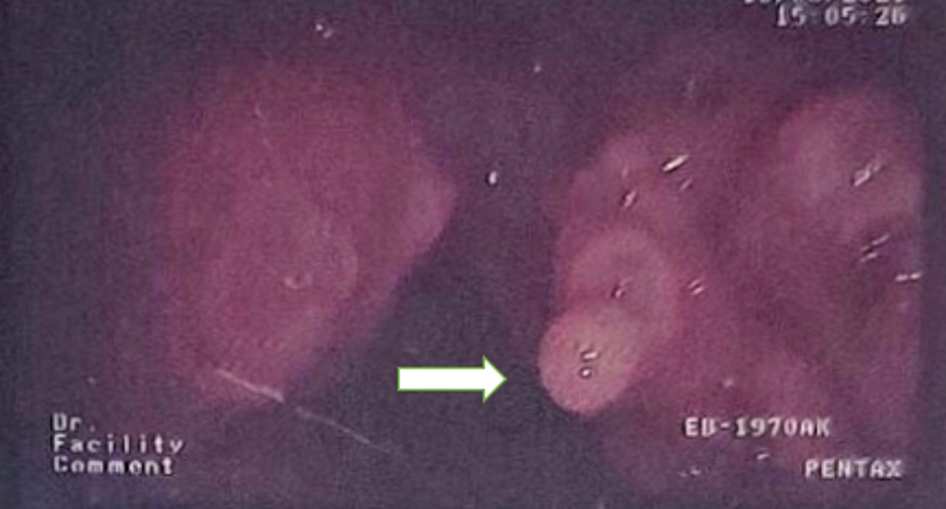
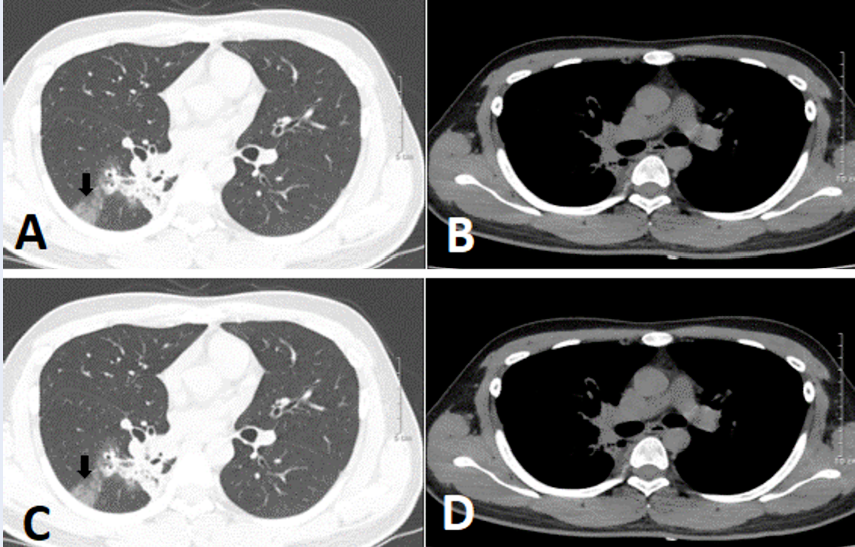
Seven days post-admission, a chest computed tomography (CT) scan with contrast showed that the right lung had cystic lesion with mild and irregular wall thickening scattered throughout the right lung field. The largest lesion was 42 mm in diameter and communicated with neighboring bronchial branches, thickened fibrous interstitial tissue, and adjacent parenchyma. There were also multiple solid nodules; the largest at the apex was 19 mm x 15 mm. The lung parenchyma of the lower lobe exhibited opacified ground glass lesions. The left lung also had abnormal nodular masses, but no enlarged lymph node or mediastinal masses (Figure 2). In addition, the patient’s bilateral vocal cords and vocal folds were increased in size, with soft nodular tissue protruding into the lumen and causing laryngeal stenosis in this region; the narrowest point was 4 mm in diameter (Figure 3). CT imaging suggested the presence of an airway papilloma. Accordingly, bronchoscopy showed the position of a hypopharynx-larynx polypoid lesion on the patient’s bilateral vocal cords and adhesions on the vocal cord anterior margin (Figure 4).
The patient was evaluated for tuberculosis (TB), fungal and bacterial infection , and malignancy. All tests were negative, including the TB test, and no bacteria or fungi were detected in bronchial fluid specimens. Histopathology of the vocal cord lesions showed no malignant cells and suggested a papilloma. The patient’s final diagnosis was airway papillomatosis with laryngeal and bronchial tree involvement. The patient was treated conservatively and symptomatically with the antibiotic moxifloxacin (400 mg due to clinical, radiological, and laboratory manifestations of a respiratory tract infection) and the mucolytic bromhexine (8 mg) for two weeks with follow-up every six months.
Discussion
Airway papillomatosis, characterized by the development of papillomas in the respiratory tract, is a disease caused by HPV. There are more than 200 subtypes of HPV, but subtypes 6 and 11 account for 90% of cases1. Subtypes 16, 18, 31, and 33 are also associated with pathology but at a lower rate5. Subtypes 16 and 18 constitute high-risk infections and are associated with the potential for malignant transformation to squamous cell carcinoma4. Recurrent respiratory papillomatosis can affect individuals of all ages, but most commonly affects children from 2 – 4 years of age and adults 20 – 40 years of age6. Airway papillomatosis in children is more common and more aggressive than in adults. The age of onset of our patient is not known; he experienced dysphonia since childhood but his pulmonary symptoms occurred one month before hospital admission. There is no difference in the incidence of airway papillomatosis between males and females6.
The most common respiratory site of papilloma formation are the larynx and vocal cords; lesions occur less frequently in the lower trachea, bronchi, and lungs. Other sites that may be involved include the oropharynx, nasopharynx, nose, and oral cavity4. Common clinical symptoms include dysphonia and prolonged cough less common are stridor and dyspnea7. In general, clinical signs are often nonspecific and require confirmation by other testing methods such as CT, endoscopic biopsy, or HPV DNA tests.
CT plays an important role in the diagnosis and characterization of lesions. The most common features include nodular thickening of the trachea and main bronchi solid nodules in the lung parenchyma cavitated nodules and masses air trapping and occasionally, pleural effusion7. In addition, the tracheal wall may appear irregular due to fibrosis or the presence of papilloma. Bronchiectasis or obstructive atelectasis may also occur. In cases of malignant transformation, regional lymph nodes can be seen8. Bronchoscopy is a critical tool that allows clinicians to view central airway lesions and collect specimens for pathology. A definitive diagnosis of airway papillomatosis is made on histopathology. Microscopically, papillomas consist of non-keratinized stratified squamous epithelium over a fibrovascular core9.
Currently, there is no cure for airway papillomatosis but surgical resection is the most important treatment modality. The goal of surgery is to remove as many papillomas as possible without damaging normal anatomical structures, thereby ensuring airway clearance and preserving vocal function4. Adjuvant therapy is indicated when surgery is not effective. Adjuvant treatments include antiviral drugs such as acyclovir and cidofovir, interferon, photodynamic therapy, and gene therapy.
Our patient was admitted to the hospital with a persistent cough and fever, and laboratory tests indicated the presence of inflammation. A CT scan revealed bilateral vocal cord and lung lesions consistent with airway papillomatosis. As a result, we performed otolaryngoscopy and bronchoscopy. Although we did not conduct an HPV DNA test, the patient’s final diagnosis was airway papillomatosis. Treatment was conservative and consisted of symptomatic treatment with periodic re-examination.
Conclusion
Airway papillomatosis is a chronic disease caused by the human papillomavirus (HPV) and manifests as a benign proliferation of squamous papillae in the airways. Although it is a benign disease, its clinical presentation can be severe, especially in young children. Treatment is challenging and there are no cures. Thus, to reduce the risk of recurrence and spread of lesions throughout the airways, early, correct diagnosis and careful treatment selection are required.
Abbreviations
None.
Acknowledgments
None.
Author’s contributions
Le VD and Ma MH: Case file retrieval and case summary preparation. Nguyen NC, Thieu-Thi TM, and Nguyen MD: preparation of manuscript and editing. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. Our institution does not require ethical approval for reporting individual cases or case series. Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Fusconi
M.,
Grasso
M.,
Greco
A.,
Gallo
A.,
Campo
F.,
Remacle
M.,
Recurrent respiratory papillomatosis by HPV: review of the literature and update on the use of cidofovir. Acta Otorhinolaryngologica Italica.
2014;
34
(6)
:
375-81
.
PubMed Google Scholar -
Seedat
R.Y.,
Juvenile-Onset Recurrent Respiratory Papillomatosis Diagnosis and Management - A Developing Country Review. Pediatric Health, Medicine and Therapeutics.
2020;
11
:
39-46
.
View Article PubMed Google Scholar -
Derkay
C.S.,
Wiatrak
B.,
Recurrent respiratory papillomatosis: a review. The Laryngoscope.
2008;
118
(7)
:
1236-47
.
View Article PubMed Google Scholar -
Ouda
A.M.,
Elsabagh
A.A.,
Elmakaty
I.M.,
Gupta
I.,
Vranic
S.,
Al-Thawadi
H.,
HPV and Recurrent Respiratory Papillomatosis: A Brief Review. Life (Basel, Switzerland).
2021;
11
(11)
:
1279
.
View Article PubMed Google Scholar -
Venkatesan
N.N.,
Pine
H.S.,
Underbrink
M.P.,
Recurrent respiratory papillomatosis. Otolaryngol Clin North Am.
2012;
45
(3)
:
671-694
.
View Article PubMed Google Scholar -
Perdana
R.F.,
Management of two cases of tracheobronchial management of two cases of tracheobronchial papillomatosis at tertiary hospital in Indonesia: A case report. International Journal of Surgery Case Reports.
2021;
83
:
106054
.
View Article PubMed Google Scholar -
Fortes
H.R.,
Ranke
F.M.,
Escuissato
D.L.,
Araujo Neto
C.A.,
Zanetti
G.,
Hochhegger
B.,
Laryngotracheobronchial papillomatosis: chest CT findings. Jornal Brasileiro de Pneumologia.
2017;
43
(4)
:
259-63
.
View Article PubMed Google Scholar -
Valdivia Padilla
A.,
Tellez-Garcia
E.,
Grosu
H.,
A Case of Recurrent Respiratory Papillomatosis With Lung Involvement and Malignant Transformation. Cureus.
2022;
14
(4)
:
e24370
.
View Article PubMed Google Scholar -
Zhang
Z.,
Chang
M.,
Moreta-Sainz
L.M.,
Case Report: Pulmonary Papillomatosis in a Patient Presenting with Cough and Hemoptysis. The Permanente Journal.
2015;
19
(3)
:
e125-7
.
View Article PubMed Google Scholar
Comments
Article Details
Volume & Issue : Vol 9 No 12 (2022)
Page No.: 5450-5454
Published on: 2022-12-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 4949 times
- PDF downloaded - 1134 times
- XML downloaded - 0 times
 Biomedpress
Biomedpress