A pilot study of comorbidities in patients with Rheumatoid Arthritis at a tertiary care hospital in Northeast India
Abstract
On an average, rheumatoid arthritis is associated with one or more comorbid conditions and these comorbidities are associated with various risk factors and medications use in patients with RA. The aim of this study was to assess comorbidities in patients with RA at a tertiary care hospital of Northeast India. This cross sectional study was conducted for 8 months from August 2014 to April 2015. The data was collected from medicine (unit-III) outpatient department of Gauhati Medical College and Hospital, Guwahati, Northeast India. Fifty one RA patients were found during study period. Patient’s socio-demographic characteristics, comorbidities, risk factors for comorbidities, laboratory investigations, and past & current medications use were collected during their visit to hospital. DAS28 scale was used to assess the disease activity in RA patients. Descriptive statistics were used. Non-normally distributed continuous variables are presented in median and interquartile range. The median age of RA patients was 45(IQR;15). The disease activity was found high (DAS-ESR>5.1) in 34 (66.67%) patients. The median DAS28 score was 5.64(IQR;1.44). Majority of the patients with RA were anaemic (n=34, 66.67%) followed by infection (n=7, 13.73%), thyroid disease (n=5, 9.80%), renal disease (n=4, 7.84%), osteoporosis (n=3, 5.88%), cardiovascular disease (n=3, 5.88%), lung disease (n=3, 5.88%), and vasculitis (n=1, 1.96%). The commonly reported risk factor was hypertension (19.61%) followed by diabetes (n=5, 9.80%), dyslipidemia (n=4, 7.84%), smoking (n=4, 7.84%), family history of CVD (n=2, 3.92%), and alcohol intake (n=1, 1.96%). Among DMARDS, methotrexate (92.16%) was the most commonly prescribed drug followed by hydroxychloroquine (74.51%) and sulfasalazine (27.45%). Anaemia was the most common comorbid condition found in RA patients. Disease activity was found high in anaemic patients with RA.
Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disease that primarily involves the joints. Rheumatoid arthritis can also affect non-articular muscular structures such as tendons, ligaments, and fascia. World-wide the prevalence of RA varies between 0.5% - 1%. In India, the prevalence of RA is 0.75% Malaviya et al.,1993. Usually, diagnosis of RA patients is done by clinical features (signs and symptoms), laboratory investigations and radiographic findings. The clinical features of this disease involve symmetrical arthralgia and swelling in the small joints of hands, feet and wrists. It also includes soft tissue swelling around the joints with morning stiffness.
The disease activity reflects the burden of inflammation and aid in decision making in the treatment of patients with RA. The main goal of the therapy is to achieve remission, and this could be achieved by assessing disease activity in routine clinical practice Shah A, 2012. The disease activity score in 28 joints (DAS28) scale is commonly used tool for the assessment of disease activity in RA patients. As per this scale, RA patients were scored for the 28-joint count (tender/swollen), global health assessment (GH) was done using visual analog scale (VAS), and ESR was performed using Westergren’s method, in mm/first hour. This scale describes the disease activity regarding low, moderate, high, and has remission criteria. It consists of a continuous index arange from 0 to 9.4, in which low disease activity is defined as ≤3.2; moderate disease activity is considered between >3.2 to ≤5.1, and high disease activity is defined as >5.1. A commonly used cutoff point for remission in DAS28 is <2.6 Anderson et al.,2012.
The chronic inflammation affects various organ systems of the body and is responsible for a number of comorbidities with RA Dougados et al., 2014. It has been reported that the patients with RA mostly suffer from at least one or more comorbid conditions Al- Bishri et al., 2013. Cardiovascular disease (CVD), infections, osteoporosis, lung disease, thyroid disease and malignancy are common comorbid conditions found in patients with RA. These comorbidities reduce lifespan in RA patients Al-Bishri et al.,2013Dougados et al., 2014. The risk factors like hypertension, diabetes, dyslipidemia, smoking and alcohol intake are also predisposed to the development of comorbidities in patients with RA Kirui et al., 2013. The medications used to treat RA are also responsible for the development of various comorbidities in RA patients Al-Bishri et al.,2013. Therefore, the objectives of this study were to assess the comorbidities in patients with RA on disease activity, risk factors, and medication use.
Subjects and Methods
This cross-sectional study was conducted for eight months from August 2014 to April 2015. The prior permission from institutional ethical committee of Gauhati Medical College and Hospital (GMCH) was obtained to conduct this pilot study. The data was collected from medicine outpatients department (OPD) unit-III of GMCH, Guwahati, Northeast India. In our study, those patients who were diagnosed by American College of Rheumatology criteria-2010 Aletaha et al., 2010 were considered. Adult patients with age ≥ 18 of either gender were included in this study. Pregnant and breastfeeding women were excluded. The data comprised of the patient’s socio-demographic characteristics, comorbidities, risk factors for comorbidities, laboratory test results, and the past & current medications use. Data on medications were collected in predesigned reporting form during the study period.
The disease activity was assessed by using DAS28 scale Fleischmann et al., 2014. Clinical assessment was performed by resident doctors at OPD under the supervision of rheumatologist who were not involved in treatment decisions. DAS28 score was calculated by using the following formula:
DAS28= 0.56√TJC + 0.28√SJC + 0.70 (ln ESR) + 0.014 (GH), where TJC is the Tender Joint Count, SJC is the Swollen Joint Count, ESR is the Erythrocyte Sedimentation Rate, and GH is the Global Health on VAS Scale (0–100 mm).
Descriptive statistics were used for data analysis. Median and interquartile range (IQR) for non-normally distributed continuous variables was calculated.
Results
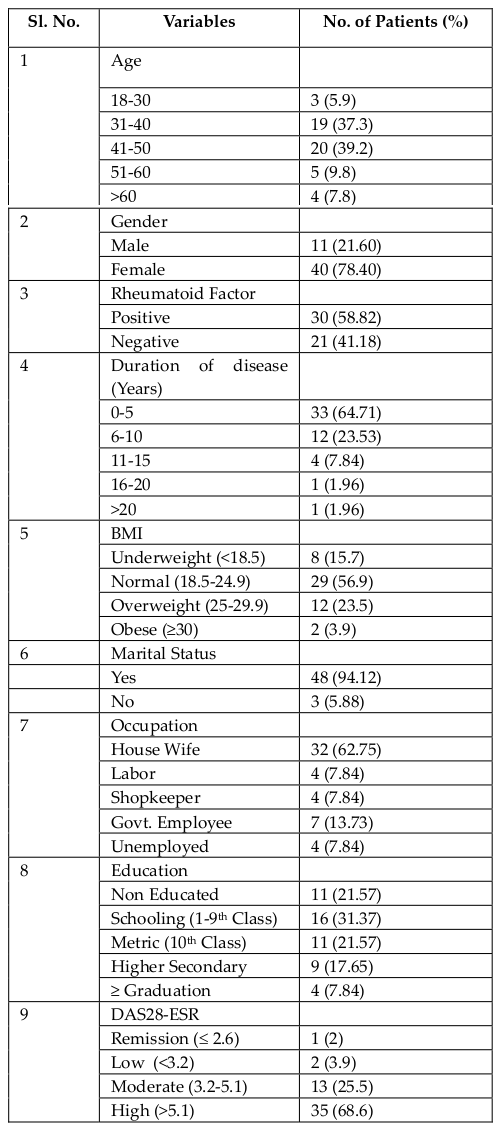
Socio-demographic characteristics
In this pilot study, 51 RA patients were enrolled. Out of these, 40 (78.40%) patients were female, and 11 (21.60%) were male. Most of the patients were in the age group of 41-50 years ( Table 1 ). The age of patients with RA varied significantly. The median age of RA patients was 45(IQR;15). Rheumatoid factor (RF) wasfound positive in 30 (58.82%) patients. In this study, the presence of anti-CCP antibody was checked in 37 RA patients, and it was found in 25 RA patients. The disease duration in most of the patients with RA (64.71%) was less than five years ( Table 1 ). Body mass index (BMI) in RA patients was also estimated in this study. Twenty-nine (56.9%) patients were found with normal BMI (18.5-24.9) while 12 (23.5%) patients were with high BMI (25-29.9) ( Table 1 ).
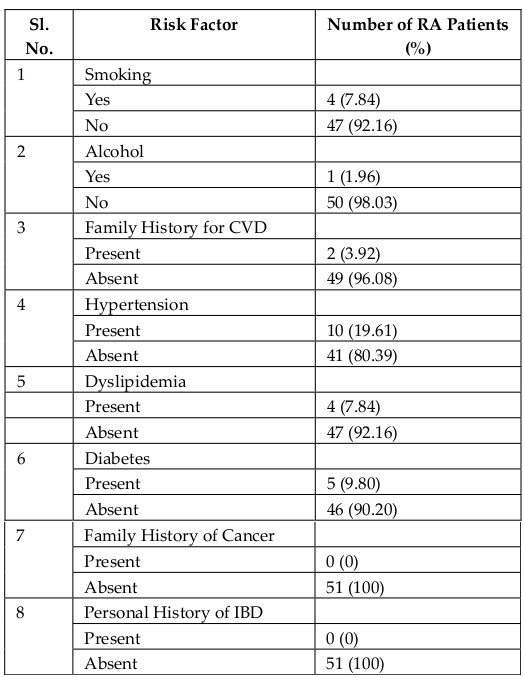
Comorbidities and their risk factors
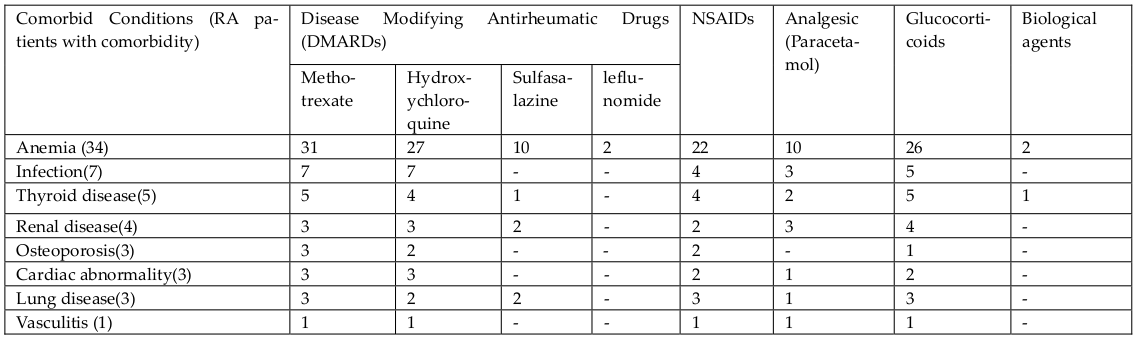
Total 60 comorbidities with RA were reported from 51 patients. Anemia (n=34, 66.67%) was the leading comorbidity followed by infection (n=7, 13.73%), thyroid disease (n=5, 9.80%), renal disease (n=4, 7.84%), osteoporosis (n=3, 5.88%), cardiovascular disease (n=3, 5.88%), lung disease (n=3, 5.88%), and vasculitis (n=1, 1.96%) ( Table 2 ). Out of 34 RA patients with anaemia, 29 (56.86%) RA patients were female while 5 (9.80%) RA patients were male. Among risk factors, 10 (19.61%) RA patients were found to have hypertension followed by diabetes (n=5, 9.80%), dyslipidemia (n=4, 7.84%), smoking (n = 4, 7.84%), family history of CVD (n=2, 3.92%) and alcohol intake (n=1, 1.96%) ( Table 3 ).
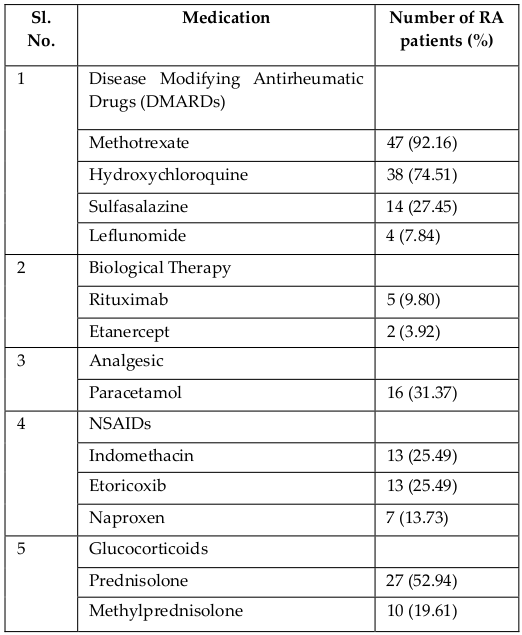
Medication use
Most of the RA patients were receiving diseasemodifying antirheumatic drugs (DMARDs) and glucocorticoids ( Table 4 ). Among DMARDs, methotrexate was prescribed to 47(92.16%) RA patients followed by 38(74.51%) patients were on hydroxychloroquine, 14(27.45%) patients were on sulfasalazine and 4(7.84%) patients were taking leflunomide. Among glucocorticoids, 27(52.94%) patients were taking prednisolone while 10(19.61%) patients were on methylprednisolone. Most of the anaemic patients with RA had received DMARDs and glucocorticoids ( Table 5 ).
Disease activity based on DAS28 score
The disease activity was found high (DAS-ESR > 5.1) in 35 RA patients (68.6%) ( Table 1 ). Among comorbidities, disease activity was found high in anaemic patients with RA. The median DAS28 score was 5.64(IQR;1.44).
Discussion
RF is one of the useful tools in the diagnosis of patients with RA Bishri et al., 2013. In our study, more than half of the patients (58.82%) had positive RF while Anti-CCP antibody was present in half of the total RA patients.
In clinical practice, there is the general consideration that RA should be controlled as completely as possible. In daily practice, DAS28 scale could be used to determine and evaluate the status and course of disease activity in RA patients. In our study, most of the RA patients were anaemic, and disease activity was also high in these patients. Similarly, in the study of Moller et al. Disease activity was also high in anaemic patients with RA Möller et al., 2013. In this study most of the female RA patients were anaemic. This condition may pre-exist in female patients before the disease was diagnosed. Thus, the causality between disease activity and comorbidities was not performed due to lack of past medical history of patients with RA.
Patients with RA are at high risk of bacterial, tubercular, fungal and other opportunistic infections Michaud and Wolfe, 2007. In our study, mainly respiratory tract infection (RTI), tuberculosis, urinary tract infection (UTI), fungal infection and periodontitis were found in RA patients. As reported, the incidence of UTI in female patients with RA is high Mowat et al., 1970 whereas in our study only 1 case of UTI was found in an older female with RA. Studies have also reported that older age patients and females are mostly associated with osteoporosis in patients with RA Al-Bishri et al., 2013Kelly et al., 2013. In our study, most of the RA patients were of upper middle age and three female patients were found with osteoporosis. Moreover, studies have showed the significant association between RA and thyroid disease Al-Bishri et al., 2013Mosli and Attar, 2014. In this study, five female patients were with thyroid disease.
Heart disease remains a major problem in patients with RA. In this study, 3 RA patients were with cardiovascular abnormality. Out of these, two patients were with ST segment abnormality and one patient was with left anterior hemiblock. Among risk factors, hypertension was commonly reported in RA patients in this study. Therefore, early referral to a cardiologist for appropriate evaluation and treatment can provide the best chance of optimizing outcomes.
The use of glucocorticoids, DMARDs, NSAIDs, and biological agents are commonly associated with a number of comorbidities in patients with RA Al-Bishri et al., 2013. The glucocorticoids use in patients with RA are commonly associated with the development of hypertension, hyperglycemia, infection, and osteoporosis Panoulas et al., 2008 whereas NSAIDs use are mostly associated with risk of hypertension, gastrointestinal bleeding, nephropathy, nephritis and anaemia Al-Bishri et al., 2013Kelly et al., 2013. However, in this study, most of the RA patients were anaemic and received methotrexate, hydroxychloroquine, glucocorticoid, and NSAIDs.
This study has some potential limitations. The sample size was small. The study was cross-sectional, and therefore, causality among disease activity, comorbidities and medication use was not performed. Beside this, generalisability is another limitation. However, his study provides useful observations regarding disease activity, comorbidities and medication use in RA patients. Rheumatologists should consider comorbidities as an important aspect of therapeutic management in RA patients.
Conclusion
RA patients may have one or more comorbid conditions. Anaemia is a most common comorbid condition in RA patients. There is also a need of further research to establish a definite correlation between comorbidities and disease activity in RA patients.
Abbreviations
RA: Rheumatoid Arthritis
GMCH: Gauhati Medical College and Hospital
DAS28: Disease Activity Score in 28 joints
CVD: Cardiovascular diseases
GH: Global Health assessment
VAS: Visual Analog Scale
TJC: Tender Joint Count
SJC: Swollen Joint Count
ESR: Erythrocyte Sedimentation Rate
BMI: Body Mass Index
DMARDs: Disease Modifying Antirheumatic Drugs
RTI: Respiratory tract infection
UTI: Urinary tract infection
MI: Myocardial infarction
IHD: Ischemic heart disease
CCF: Congestive cardiac failure
CVD: Cardiovascular diseases
CBC: Complete blood count
LFT: liver function test
References
-
J.
Al-Bishri,
S.
Attar,
N.
Bassuni,
Y.
Al-Nofaiey,
H.
Qutbuddeen,
S.
Al- Harthi,
S.
Subahi.
Comorbidity profile among patients with rheumatoid arthritis and the impact on prescriptions trend. Clinical medicine insights Arthritis and musculoskeletal disorders.
2013;
6
:
11
.
-
D.
Aletaha,
T.
Neogi,
A.J.
Silman,
J.
Funovits,
D.T.
Felson,
C.O.
Bingham,
N.S.
Birnbaum,
G.R.
Burmester,
V.P.
Bykerk,
M.D.
Cohen.
2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis & Rheumatism.
2010;
62
:
2569-2581
.
-
J.
Anderson,
L.
Caplan,
J.
Yazdany,
M.L.
Robbins,
T.
Neogi,
K.
Michaud,
K.G.
Saag,
J.R.
O’dell,
S.
Kazi.
Rheumatoid arthritis disease activity measures: American College of Rheumatology recommendations for use in clinical practice. Arthritis care & research.
2012;
64
:
640-647
.
-
M.
Dougados,
M.
Soubrier,
A.
Antunez,
P.
Balint,
A.
Balsa,
M.H.
Buch,
G.
Casado,
J.
Detert,
B.
El-Zorkany,
P.
Emery.
Prevalence of comorbidities in rheumatoid arthritis and evaluation of their monitoring: results of an international, cross-sectional study (COMORA). Annals of the rheumatic diseases.
2014;
73
:
62-68
.
-
R.
Fleischmann,
D.
van der Heijde,
A.S.
Koenig,
R.
Pedersen,
A.
Szumski,
L.
Marshall,
E.
Bananis.
How much does Disease Activity Score in 28 joints ESR and CRP calculations underestimate disease activity compared with the Simplified Disease Activity Index?. Annals of the rheumatic diseases.
2014;
annrheumdis-2013-204920
.
-
C.
Kelly,
S.
Malik,
J.
Barnes,
H.
Gertig,
J.
Hamilton.
Identification and treatment of comorbidity in patients with rheumatoid arthritis. International Journal of Clinical Rheumatology.
2013;
8
:
557-568
.
-
F.
Kirui,
G.
Oyoo,
E.
Ogola,
E.
Amayo.
Cardiovascular risk factors in patients with Rheumatoid Arthritis at Kenyatta National Hospital. African Journal of Rheumatology.
2013;
1
:
15-22
.
-
A.
Malaviya,
S.
Kapoor,
R.
Singh,
A.
Kumar,
I.
Pande.
Prevalence of rheumatoid arthritis in the adult Indian population. Rheumatology international.
1993;
13
:
131-134
.
-
K.
Michaud,
F.
Wolfe.
Comorbidities in rheumatoid arthritis. Best practice & research Clinical rheumatology.
2007;
21
:
885-906
.
-
B.
Möller,
A.
Scherer,
F.
Förger,
P.M.
Villiger,
A.
Finckh.
Anaemia may add information to standardised disease activity assessment to predict radiographic damage in rheumatoid arthritis: a prospective cohort study. Annals of the rheumatic diseases.
2013;
annrheumdis-2012-202709
.
-
H.H.
Mosli,
S.M.
Attar.
Prevalence and Patterns of Thyroid Dysfunction in Patients with Rheumatoid Arthritis. Open Endocrinology Journal.
2014;
7
:
1-5
.
-
A.
Mowat,
T.
Hothersall,
J.
Gould.
Urinary tract infection in patients with rheumatoid arthritis. Annals of the rheumatic diseases.
1970;
29
:
143-148
.
-
V.F.
Panoulas,
K.M.
Douglas,
A.
Stavropoulos-Kalinoglou,
G.S.
Metsios,
P.
Nightingale,
M.
Kita,
M.
Elisaf,
G.
Kitas.
Longterm exposure to medium-dose glucocorticoid therapy associates with hypertension in patients with rheumatoid arthritis. Rheumatology.
2008;
47
:
72-75
.
-
C.E.
Shah A.
Harrison’s Principles of Internal Medicine, 18th edn. New York: McGraw-Hill.
2012
.
Comments

Downloads
Article Details
Volume & Issue : Vol 3 No 01 (2016)
Page No.: 454-459
Published on: 2016-01-26
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6580 times
- Download PDF downloaded - 1742 times
- View Article downloaded - 4 times
 Biomedpress
Biomedpress