Abstract
Epiploic appendices are small pouches filled with projection-like fat structure adjacent to the antimesenteric side of the colon wall; they range in size from 0.5 to 5 cm and provide vascularization from small arterioles. Epiploic appendagitis is a benign condition of the epiploic appendices which leads to ischemia of the structure. Ischemia, therefore, causes localized sharp abdominal pain. Though uncommon, its symptoms can be diagnosed as acute lower abdominal pain since the symptoms could mimic diverticulitis and appendicitis. Thus, to diagnose epiploic appendagitis in this case, a CT scan was conducted to detect a fat-dense lesion of ovoid-like structure close to the colon. Given the good response to conservative management, establishing a correct diagnosis could help to minimize inappropriate invasive management.
INTRODUCTION
Epiploic appendices are small pouches filled with projection-like fat structures adjacent to the antimesenteric side of the colon wall. The appendices range from 0.5 to 5 cm and provide vascularization from small arterioles1. Epiploic appendagitis will be referred to hereafter as appendagitis. It is considered a self-limiting benign condition caused by torsion or thrombosis which leads to ischemia of the fat structures. Ischemia, in turn, causes localized sharp abdominal pain, especially on the lower left abdomen quadrant (in 76% of cases)2, 3. Appendagitis mostly affects male patients in their 40s to 50s1, 3. In the case of appendagitis, it is often overlooked or misdiagnosed since the acute lower abdominal pain symptoms associated with it can mimic diverticulitis and appendicitis.
Appendagitis shows clinical signs of localized peritoneal inflammation with specific imaging findings of localized fat density with ovoid-like structures close to the colon when imaged by computed tomography (CT)4. Herein, we report three men with abdominal pain who were diagnosed with appendagitis. Given the rarity of cases of appendagitis and that its symptoms often mimic symptoms of diverticulitis and appendicitis5, it is important to consider appendagitis as one of the possible diagnoses for abdominal pain to minimize unnecessary invasive management.
CASE PRESENTATION
Patient 1
A 48-year-old male complaining of pain in the right lower quadrant abdomen which started 24 hours prior was admitted to the Emergency department. On the admission day, he had a sharp pain which arose suddenly and was localized. He was hemodynamically stable and had a body mass index (BMI) of 31 kg/m2. However, this patient had no fever. On examination, his cardiorespiratory test was normal, but he had tenderness in his right lower quadrant abdomen. Blood tests showed mild leukocytosis (10.3 x 103/mm3). He had no history of surgery nor intake of medications.
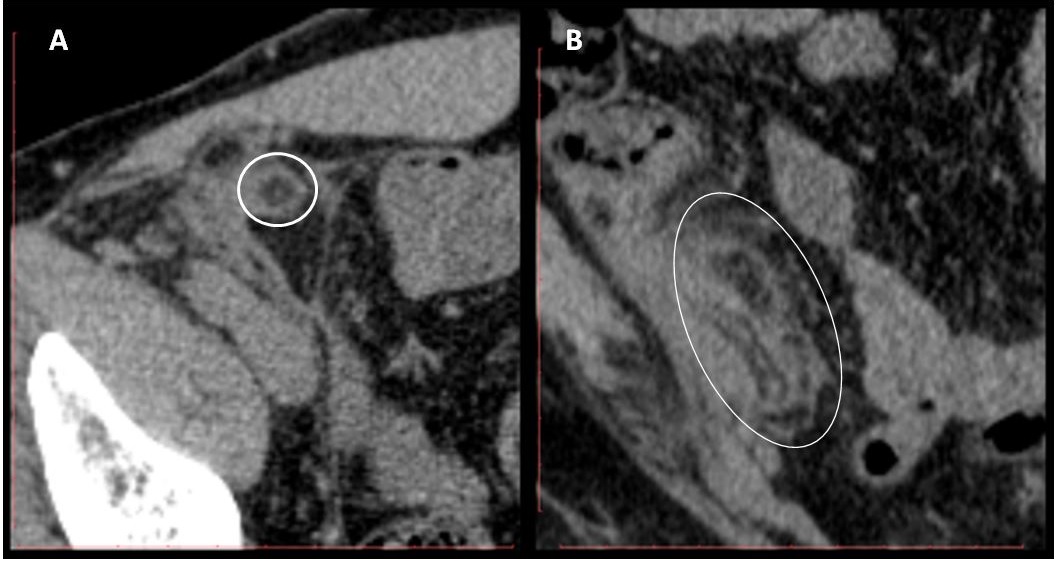
The patient was suspected as having appendicitis and was then referred to the Radiology department for CT scan. The scan revealed pericaecal lesion with fat attenuation and hyperattenuating rim, measuring 1.11 x 0.81 x 3 cm. There was also fat stranding observed adjacent to the lesion and multiple lymphadenopathies mesenterial to the right lower quadrant (RLQ). However, the appendix was normal, and the rest of the evaluation was unremarkable (Figure 1). Therefore, the patient was diagnosed as having epiploic appendagitis.
The patient was given conservative treatment with bed rest and non-steroid anti-inflammatory drugs (NSAIDs). His symptoms were relieved, and he was discharged 2 days later with good condition.
Patient 2
A healthy 35-year-old male came to the internal medicine practice with a 72-hour history of left iliac fossa pain. The sharp pain occurred suddenly. Prior to it, the patient had never experienced radiating pain, nor experienced symptoms or pain in the bowel or genitourinary areas. He had no history of fever or abdominal trauma. He felt uncomfortable during the examination. His condition was apyrexial, was hemodynamically stable, and with a body mass index of 23.87 kg/m2.
The examination of cardiorespiratory functions showed normal sign. However, his abdomen showed signs of local tenderness in the left iliac fossa. Blood tests showed no sign of elevated inflammatory markers. The symptoms were not adequate enough to establish a diagnosis so a CT scan of the patient’s abdomen was conducted.
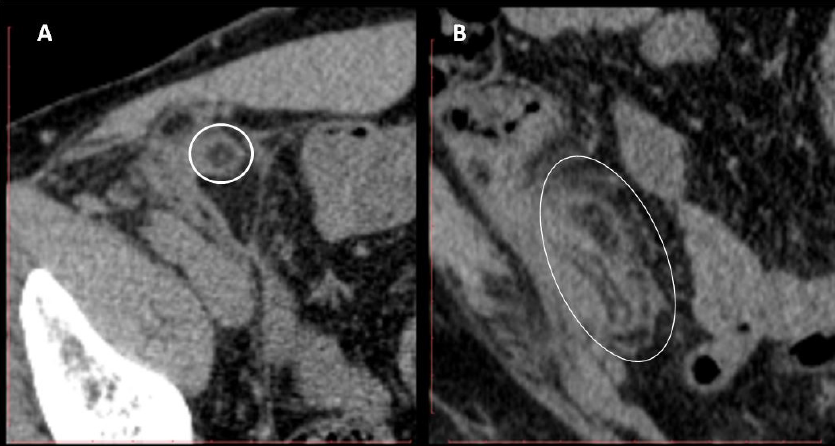
The result showed that there was an ovoid-like structure of fat attenuation. The high-attenuation of fat showed in the rim, which appeared from the anterior wall of the descending colon, was encircled by mesenteric fat stranding that was inflamed, but had no bowel wall thickening (Figure 2). The patient was admitted to the surgical ward and treated with symptomatic medication, NSAIDs and antibiotics. The patient was in good condition and his symptoms were completely resolved after the 3rd day of hospital admission.
Patient 3
A 40-year-old male exhibited pain for 3 days in the left lower quadrant abdomen. No nausea, vomiting or change in bowel habits were indicated. The vital signs of the patient were in the normal range; his body mass index was 20.5 kg/m2. However, physical examination showed tenderness and guarding in the left lower quadrant abdomen. Complete blood count showed a mild leukocytosis (10.5 x 103 /mm3).
The patient was referred to the Radiology department with a concern for diverticulitis. Non-enhanced abdominal CT scan showed a fat density lesion with ovoid-like structure (with surrounding inflammation), measuring about 1.7 x 3 x 3.16 cm which abutted the sigmoid colon (Figure 3). This feature was suggestive of epiploic appendagitis. The appendix was normal and the rest of the study was unremarkable. The patient received some symptomatic medication and antibiotics for home care.
DISCUSSION
Epiploic appendices are subserous lobulated fat structures adjacent to the external surface of taenia coli, approximately 50 – 100 in number, found predominantly on the anterior and posterolateral surfaces6. They vary in dimension and amount, based on ethnicity and metabolic conditions, such as obesity and metabolic syndromes7. Each structure is fed by two arterioles and one venule within vascular stalks attached to the colon. These structures are commonly found on the sigmoid colon (57%), cecum (26%), ascending colon (9%), transverse colon (6%), and descending colon (2%)7, 8. These explain the pathophysiology of left lower quadrant abdominal pain experienced by patients, as was observed in these patients.
The terminal blood supply within stalks make appendices vulnerable to ischemic complications due to torsion or minor thrombosis7, 9. Ischemia leads to an inflammatory state of the appendices known as primary appendagitis epiploicae. The secondary ones are commonly caused by post-operative adhesion, inflammatory processes from surrounding structures (such as diverticulitis, appendicitis, Crohn’s ileitis, and pelvic inflammatory disease), extensive abdomen muscle training, and weight loss7, 10. We did not find any risk factors in our patients so we concluded all of them as having primary appendagitis.
Appendagitis has been reported in 2 — 7% of patients initially diagnosed with acute diverticulitis and in 0.3 — 1% of patients with suspected acute appendicitis11. This is consistent with observations of our first and third patients. On admission, the first patient was suspected as having acute appendicitis while the third patient was suspected as having diverticulitis.
Epiploic appendices are not well-developed during growth periods and, therefore, the majority of cases develop during the fourth decade, predominantly among males7. Nevertheless, some publications have reported cases of younger age, from childhood age to older age (beyond 80 years old), especially in obese patients11, 12, 13. This kind of epidemiologic characteristic could be found in our patients. They were in their fourth decade in terms of age, but they did not have any risk factors such as obesity and metabolic syndromes.
The characteristic clinical findings are sudden acute abdominal pain that is worsened with movement. The pain is localized, non-migratory, and commonly found on the lower abdominal quadrant. Fever, nausea, vomiting, anorexia, and change of bowel habit are rarely found. In physical examination, it is possible to find local abdominal guarding. In addition, it has been reported that there can be slightly elevated leukocytes and C-reactive protein (CRP) level; the former was found in our first and third patients as a natural response to the inflammatory process7, 10, 14.
Radiologic imaging, especially CT scanning as the modality of choice, plays an important role in establishing diagnosis of appendagitis. Normal appearance of appendices could not be found in the CT scans, but there were specific findings in the inflamed appendices. The most common and pathogenic findings, as observed in all of the 3 patients, was a fat-dense ovoid-like structure close to the colon. The structure was about 1.5-3.5 cm in diameter with thin high-density showing in the rim (1-3 mm thick), known as the hyperattenuating ring sign15, 16. Although the hyperattenuating ring sign is pathognomonic, absence of this finding does not eliminate possibility of diagnosis. It looks more prominent than the thickening of the adjacent colon wall, due to reactivity to the inflammation process, and helps differentiate appendagitis from diverticulitis, appendicitis, and acute cholecystitis17.
Other modalities such as ultrasonography (US) and magnetic resonance imaging (MRI), although rarely used, could give useful information regarding diagnosis. Experienced ultrasonographers can find a non-compressible hyperechoic oval lesion adjacent to the colon located near pain localization18. On MRI findings, there was a fat-intensity ovoid structure with central hypointense dot and peripheral T1W1, as well as a central hyperintense dot and peripheral T2W fat suppression with rim enhancement on contrast7.
For the past 20 years, it has already been established that most appendagitis cases have a good response to conservative treatments and NSAID regiment, as was observed in our patients. Surgical treatment has usually been only performed for cases complicated with intussusception, abscess, and obstruction13, 19. Conservative treatment could minimize surgery and anesthesia complications, and could reduce the length of stay and cost of treatment20.
Appendagitis must be detected earlier so that the condition does not worsen in the patients. In this study, all of the 3 patients had early-stage appendagitis which was confirmed by CT scan. Earlier detection of appendagitis recovered our patients immediately and minimized inappropriate invasive management like surgery.
CONCLUSION
The signs and symptoms of epiploic appendagitis are not specific and, therefore, clinical diagnosis of this disease has barely been established. Radiologic modalities could provide additional information for clinicians. The possibility of appendagitis as a diagnosis should be applied to each patient who presents with non-specific abdominal pain. Although as a disease it is rare, the proper clinical diagnosis of epiploic appendagitis could eliminate unnecessary surgical and invasive treatments for the patients since appendagitis responds well to conservative management.
ABBREVIATIONS
CT: Computed Tomography
CRP: C-reactive protein
US: Ultrasonography
MRI: Magnetic Resonance Imaging
ACKNOWLEDGMENTS
None.
AUTHORS’ CONTRIBUTIONS
Literature search, Clinical studies, Data acquisition, Data analysis, Manuscript preparation: Ronny. The author read and approved the final manuscript.
FUNDING
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
CONSENT FOR PUBLICATION
Not applicable.
COMPETING INTEREST
The author declares that has no conflicts of interest.
References
-
Ozturk M, Aslan S, Saglam D, Bekci T, Bilgici MC. Epiploic Appendagitis as a Rare Cause of Acute Abdomen in the Pediatric Population: Report of Three Cases. Eurasian J Med.
2018;
50
(1)
:
56-58
.
View Article PubMed Google Scholar -
Almuhanna AF, Alghamdi ZM, Alshammari E. Acute epiploic appendagitis: A rare cause of acute abdomen and a diagnostic dilemma. J Family Community Med.
2016;
23
(1)
:
48-50
.
View Article PubMed Google Scholar -
Goh VL, Rudolph CD. Epiploic Appendagitis. J Ped Gastroenter and Nutrition.
2011;
53
(1)
:
1
.
View Article PubMed Google Scholar -
Coulier B, Ramboux A. Spontaneous Hemoperitoneum from Bleeding of a Pedunculated Epiploic Appendage. J Belg Soc Radiol.
2018;
102
(1)
:
36
.
View Article PubMed Google Scholar -
Giambelluca D, Cannella R, Caruana G, Salvaggio L, Grassedonio E, Galia M, et al. CT imaging findings of epiploic appendagitis: an unusual cause of abdominal pain. Insights Imaging.
2019;
10
(1)
:
26
.
-
Patel NB, Wenzke DR. Evaluating the Patient with Right Lower Quadrant Pain. Radiol Clin North Am.
2015;
53
(6)
:
1159-1170
.
View Article Google Scholar -
Martinez CAR, Palma RT, Silveira JPP, Sato DT, Rodrigues MR, Resende JHCd, et al. Primary epiploic appendagitis. J of Coloproctology.
2013;
33
(3)
:
161-166
.
View Article Google Scholar -
Sand M, Gelos M, Bechara FG, Sand D, Wiese TH, Steinstraesser L, et al. Epiploic appendagitis--clinical characteristics of an uncommon surgical diagnosis. BMC Surg.
2007;
7
:
11
.
View Article PubMed Google Scholar -
Akay S, Yilmaz C, Selek E, Erkan N. Torsion of Epiploic Appendages: An Overlooked Cause of Acute Abdomen. J Emergency Med.
2012;
42
(3)
:
309-310
.
View Article PubMed Google Scholar -
Lorente C, Hearne CB, Taboada J. Recurrent epiploic appendagitis mimicking appendicitis and cholecystitis. Proceedings (Baylor University Medical Center).
2017;
30
(1)
:
44-46
.
View Article PubMed Google Scholar -
Schnedl WJ, Krause R, Tafeit E, Tillich M, Lipp RW, Wallner-Liebmann SJ. Insights into epiploic appendagitis. Nat Rev Gastroenterol Hepatol.
2011;
8
(1)
:
45-49
.
View Article PubMed Google Scholar -
Nugent JP, Ouellette HA, O'Leary DP, Khosa F, Nicolaou S, McLaughlin PD. Epiploic appendagitis: 7-year experience and relationship with visceral obesity. Abdom Radiol (NY).
2018;
43
(7)
:
1552-1557
.
View Article PubMed Google Scholar -
Issa IA, Berjaoui M-T, Hamdan WS. Primary epiploic appendagitis: from A to Z. Intern med case reports J.
2010;
3
:
67-69
.
View Article PubMed Google Scholar -
Schnedl WJ, Krause R, Wallner-Liebmann SJ, Tafeit E, Mangge H, Tillich M. Primary epiploic appendagitis and successful outpatient management. Med Sci Monit.
2012;
18
(6)
:
CS48-CS51
.
View Article PubMed Google Scholar -
Singh AK, Gervais DA, Hahn PF, Rhea J, Mueller PR. CT Appearance of Acute Appendagitis. American J Roentgenology.
2004;
183
(5)
:
1303-1307
.
View Article PubMed Google Scholar -
Neeraj N, Radha S, Anshuman K, N S. Primary Epiploic Appendagitis: Solving the Puzzle of a Benign Acute Abdomen. Open Access J of Surg.
2018;
8
(2)
:
555731
.
-
Uehara R, Isomoto H, Yamaguchi N, Ohnita K, Fujita F, Ichikawa T, et al. Epiploic appendagitis in a 27-year-old man. Med Sci Monit.
2011;
17
(10)
:
CS113-CS115
.
View Article PubMed Google Scholar -
Choi YU, Choi PW, Park YH, Kim JI, Heo TG, Park JH, et al. Clinical characteristics of primary epiploic appendagitis. J of the Korean Soc of Coloproctology.
2011;
27
(3)
:
114-121
.
View Article PubMed Google Scholar -
Erkan G, Gezen C, Bilgin SS. A Rare Cause of Abdominal Pain: Primary Epiploic Appendagitis (PEA). J Clin Anal Med.
2016;
7
(4)
:
567-569
.
View Article Google Scholar -
Clement Z. Atypical Presentations of Epiploic Appendagitis: Early Diagnosis and Non-Operative Management is the Optimal Therapy. Gastroenterology Res.
2012;
5
(2)
:
79-81
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 7 No 10 (2020)
Page No.: 4066-4070
Published on: 2020-10-31
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 7491 times
- Download PDF downloaded - 1872 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress