Abstract
Background: Blood pressure (BP) monitoring is an important aspect in the treatment of arterial hypertension (AH), namely the morning BP increase which is associated with an increased risk of cardiovascular and cerebrovascular incidents as well as sudden death. The study herein revealed clinical and functional predictors which decrease the morning BP rise in the case of optimal antihypertensive therapy with telmisartan, based on results of daily blood pressure monitoring (DBPM).
Methods: A single-center open-label study in parallel groups was conducted. The study included 50 patients with AH who had previously received antihypertensive therapy but did not achieve a reduction in BP according to DBPM. Telmisartan (40 - 80 mg per day) was added to the treatment regimen of all patients. All patients underwent a general clinical examination, measurement of glucose and creatinine levels, assessment of lipid profile, ECG recording in 12 leads, echocardiography (EchoCG), and DBPM before treatment and after 12 weeks of treatment. Statistical data analyses were performed.
Results: Twelve-week antihypertensive telmisartan-based therapy led to a decrease in mean systolic blood pressure (SBP) from 134.3 ± 5.0 to 126.2 ± 4.3 mm Hg (p = 0.008), and a decrease in mean diastolic blood pressure (DBP) from 79.8 ± 1.5 to 73.0 ± 1.4 mm Hg (p < 0.001). There was a decrease in the index of variability of DBP from 22.4 ± 2.8 to 16 ± 2.4 mm Hg (p < 0.001), and a decrease in the daily index of SBP from 15.7 ± 4.7 to 13.1 ± 4.7 mm Hg (p = 0.014). In the study, a connection was found between the decrease of the average morning index and the following indicators: presence of left ventricular (LV) hypertrophy on ECG, final diastolic size of the LV over 6.0 cm, LV ejection fraction below 52.3%, total cholesterol level over 5.5 mmol/L, LDL level greater than 3.3 mmol/L, and triglyceride level greater than 2.0 mmol/L.
Conclusion: These values could be used as predictors of a decrease in the morning index during 12-week telmisartan therapy.
Introduction
It is well-known that blood pressure (BP) level has daily fluctuations in both healthy individuals and patients with varying degrees of arterial hypertension (AH). The daily BP profile is influenced by a large number of exogenous and endogenous factors, the most powerful of which are the hypothalamic-pituitary-adrenal systems, renin-angiotensin-aldosterone systems, autonomic regulation, renal hemodynamics, endothelial and vasoactive peptides, emotional stress, physical activity, sleep patterns, and behavioral reactions1, 2.
In most people, BP rises rapidly after waking up in the morning and at the start of daily activity. BP has two main peaks — in the morning and afternoon. There is a decrease in BP during the night by 10-20% compared to the average values of systolic blood pressure (SBP) and diastolic blood pressure (DBP) in the active period1. Monitoring of morning BP rise is an important aspect in the treatment of AH and prevention of cardiovascular complications. Uncontrolled morning BP is a sign of inadequate antihypertensive therapy, insufficient dosage of drugs, or use of short-acting drugs, and is detected in the majority of patients (from 17 to 60%) treated for hypertension, according to various studies2.
At the same time, morning BP rise is associated with an increased risk (by 40%) of cardiovascular and cerebrovascular problems, and sudden death3, 4. Recent studies indicate other adverse effects of morning hypertension. Gong S. et al. established an association between morning BP increase and subclinical target organ damage, namely left ventricular myocardial mass increase, left atrial dilatation and thickening of the intima-media carotid artery complex; these changes did not depend on other BP indicators according to daily BP monitoring5.
In patients with newly diagnosed AH who did not receive treatment, the relationship between BP variability and early systolic dysfunction of the left ventricle (LV) was found, even in cases with preserved LV ejection fraction (EF)6.
Therapy of AH should include long-acting drugs and diligent monitoring to assess the impact on morning BP and patient prognosis. It is known that angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers, calcium antagonists, diuretics and, in some cases, beta-blockers are traditionally used in the treatment of AH.
There are data on the effect of angiotensin receptor blockers on morning BP. One of the drugs in this group is telmisartan. This drug provides long-term and selective blockade of angiotensin-1 receptors, without affecting other types of receptors and has a high lipophilicity, which promotes penetration into tissues3.
Another advantage of telmisartan over other angiotensin receptor blockers is the long elimination half-life, which leads to a decrease in BP for 24 hours or more, allowing the drug to be used to treat patients with morning BP surge3. It is known that compared to valsartan, telmisartan shows a higher ability to control the average daily BP and average night BP, as well as morning BP7. Studies of the efficacy of ACE inhibitors, in particular ramipril and telmisartan, have indicated a significantly greater decrease in mean SBP and morning SBP in the telmisartan group and its good tolerability8, 9, 10.
Despite the large number of studies of telmisartan, including randomized clinical trials, data on the predictors of reduction of morning BP surge are insufficient. Currently, there are no recommendations for the correction of morning hypertension, probably due to limited information about the predictive factors.
The goal of this study was to identify and establish clinical, functional and anamnestic parameters that lead to a decrease in morning BP, as determined by daily blood pressure monitoring (DBPM), in the case of optimal antihypertensive therapy based on telmisartan.
Materials — M ethods
Study design: a single-center open-label study. The study included 50 patients with AH who had previously received antihypertensive therapy but did not achieve BP control according to DBPM (Figure 1). Telmisartan (40 - 80 mg per day) was added to the treatment regimen of all patients. All patients underwent a general clinical examination, glucose and creatinine level determination, lipid profile assessment, ECG recording in 12 leads, echocardiography (EchoCG), and DBPM before treatment and after 12 weeks of treatment.
Inclusion criteria were as follows: essential AH stage I-III, administration of a combination antihypertensive therapy without BP control according to DBPM, age over 30 years, and signed informed consent to participate in the study.
Exclusion criteria were as follows: secondary AH, acute myocardial infarction (MI), acute cerebrovascular accident, myocardial revascularization (coronary artery stenting or coronary artery bypass grafting) for 3 months, heart failure (HF) III-IV class, valvular diseases in need of surgical correction, and decompensation of chronic diseases of internal organs (e.g. endocrine diseases, obstructive respiratory diseases, chronic diseases of gastrointestinal, and urinary system).
Office BP was measured using an automatic device OMRON 705-IT (OMRON, Japan). DBPM was performed on an automatic device DiaCard 03500 (Solveig, JSC Kyiv, Ukraine), with BP measurement every 15 minutes during the day and every 30 minutes at night (from 23:00 to 07:00). We analyzed the average values of 24-h ambulatory SBP and DBP, SBP and DBP during the period of activity (daytime) and nighttime, pulse BP, variability of daytime SBP and DBP, variability of nighttime SBP and DBP, maximum SBP and DBP in the morning (06.00-11.00), morning surge of SBP and DBP, morning index of SBP and DBP, as well as average value, magnitude and speed of morning surge of SBP and DBP.
EchoCG was performed on a Logiq-500 (GE, Boston, MA, USA) according to a standard protocol for determining the size of the heart chambers in the parasternal and apical positions along the long and short axes. Measurement of end-systolic size (ESS), end-diastolic size (EDS) of the left and right ventricles, end-diastolic volume (EDV) and end-systolic volume (ESV) of LV, LV and EF, evaluation of LV diastolic function, and degree of valvular insufficiency were performed. The movement of interventricular septum (IVS) in M- and B-modes was visually determined.
The size of the atriums, the thickness of the posterior wall of the LV in diastole (TPVLVd), the thickness of the interventricular septum of the LV in diastole (TIVSd), and LV myocardial mass index (LVMMI) were determined. LV hypertrophy was diagnosed in the presence of LVMMI >115 g/m2 for men and 95 g/m2 for women. The glomerular filtration rate was calculated according to the recommendations of the National Kidney Foundation (NKF) using the formula CKD-EPI (2009).
Statistical analyses of the results were performed on a personal computer using a software package for processing biological and medical information in the system, "Statistica 7.0" (Statsoft.Inc., Tulsa, OK, USA). Indicators that reflect the frequency of the sign in the sample are presented in %; quantitative indicators are given as "mean ± standard error of the mean value” (M ± m) and the interquartile range between the 25th and 75th percentiles. The results of the comparisons were considered reliable if the error probability (p) < 0.05. For quantitative indicators, for normal distribution of indicators for statistical analysis, parametric methods (Student's t-test for 2 dependent or independent variables (samples) were used; if the indicator had an abnormal distribution, non-parametric statistics were used (Mann-Whitney U-test and Wilcoxon test). A comparison of sign frequencies between groups was performed using the χ2 criterion. A nonparametric Spearman correlation analysis was performed to determine the presence and strength of the relationship between quantitative and qualitative parameters, and a discriminant step-by-step analysis was performed to determine predictors.
Ethical principles: all procedures in the study was performed in accordance with the 1964 Declaration of Helsinki. The study was approved by the local ethics committee of Communal Non-profit enterprise, Vinnytsia Regional Clinical Treatment-Diagnostics Center of Cardiovascular Pathology”, Ukraine (Protocol № 130, 05.07.2017). All patients provided written informed consent for participation in the study.
Results
A total of 50 patients were included in the study. There were 23 men (mean age of 62.4 ± 1.75 years), and 27 women (mean age of 60.1 ± 2.7 years) (p = 0.22).
Patients included in the study had AH of various degrees, in particular AH of 1st degree was diagnosed in 3 people (6%), 2nd degree — in 18 (36%), and 3rd degree — in 29 (58%). The average duration of the disease was 15.5 ± 2 years, without significant differences between men and women (Table 1).
| Characteristic | All patients, n = 50 | Men, n = 23 | Women, n = 27 | Р |
|---|---|---|---|---|
| Average age, years | 62.4 ± 1.7562.5 (54;69) | 60.1 ± 2.757.5 (54;68) | 64.4 ± 2.2366 (58;71) | 0.22 |
| AH 1st degree, abs, % | 3 (6%) | 0 (0) | 3 (6.2%) | 0.87 |
| AH 2nd degree, abs,% | 18 (36%) | 8 (34.8 %) | 10 (37%) | 0.75 |
| AH 3rd degree, abs,% | 29 (58%) | 15 (65.2%) | 14 (51.8%) | 0.39 |
| Average duration of AH, years | 15.5 ± 210 (7;23) | 13.2 ± 2.710 (5;15) | 17.5 ± 2.914.5 (8,5;23) | 0.28 |
| DM, abs,% | 23 (46%) | 9 (39.1%) | 14 (51.8%) | 0.43 |
| CHD, abs,% | 30 (60%) | 16 (69.6%) | 14 (60.9%) | 0.46 |
| MI, abs,% | 13 (26%) | 7 (30.4%) | 6 (22.2%) | 0.36 |
| Carotid atherosclerosis, abs,% | 22 (44%) | 8 (34.8%) | 14 (51.8%) | 0.17 |
| Obliterating atherosclerosis of the vessels of the lower extremities, abs,% | 12 (24 %) | 6 (26%) | 6 (22.2%) | 0.67 |
| Cerebrovascular diseases, abs,% | 7 (14%) | 4 (17.4%) | 3 (11.1%) | 0.47 |
| CKD, abs,% | 27 (54%) | 9 (39.1%) | 18 (66.7%) | 0.054 |
| Obesity, abs,% | 29 (68%) | 14 (60.8%) | 15 (55.5%) | 0.86 |
| Chronic pulmonary diseases, abs,% | 14 (28%) | 9 (39.1%) | 5 (18.5%) | 0.10 |
| Body mass index, kg/m2 | 32.3 ± 132 (29;37) | 32.2 ± 1.432 (28;36) | 32.5 ± 1.734 (29;38) | 0.86 |
| Number of patients with hypercholesterolemia, abs, % | 37 (74%) | 17 (73.9%) | 20 (74.1%) | 0.23 |
| Number of patients with dyslipidemia,abs,% | 46 (92%) | 21 (91.3%) | 25 (92.6%) | 0.85 |
| Number of smokers, abs,% | 16 (32%) | 11 (47.8%) | 5 (18.5%) | 0.0064 |
| Burdened history of AH, abs,% | 20 (40%) | 10 (43.5%) | 10 (37%) | 0.34 |
| Number of patients with left ventricular hypertrophy, abs,% | 46 (92%) | 22 (95.6%) | 24 (88.9%) | 0.67 |
The majority of patients had concomitant pathology, most often coronary heart disease (CHD) in 30 (60%) people, including a history of MI in 13 (26%). Diabetes mellitus (DM) was diagnosed in 23 (46%) people, chronic kidney disease (CKD) in 27 (54%), carotid atherosclerosis in 22 (44%), and chronic pulmonary diseases in 14 (28%), without significant differences in men and women.
The majority of subjects had signs of lipid metabolism disorders, namely in 46 (92%) patients, with signs of dyslipidemia in 37 (74%) and hypertriglyceridemia in 29 (68%). Obesity of various degrees was observed.
After 12 weeks of antihypertensive therapy based on telmisartan, a significant positive dynamic of BP was established (Figure 2). A decrease in mean 24-h SBP from (134.3 ± 5.0) to (126.2 ± 4.3) mm Hg was found (-5.4 mm Hg in average, p = 0.008). A decrease in mean 24-h DBP from (79.8 ± 1.5) to (73.0 ± 1.4) mm Hg was observed (-6.9 mm Hg in average, p < 0.001). Significant dynamics were observed in the decrease of the index of variability of DBP — from (22.4 ± 2.8) to (16.0 ± 2.4) mm Hg (p < 0.001) — and in the daily index of SBP — from (15.7 ± 4.7) to (13.1 ± 4.7) mm Hg (p = 0.014).
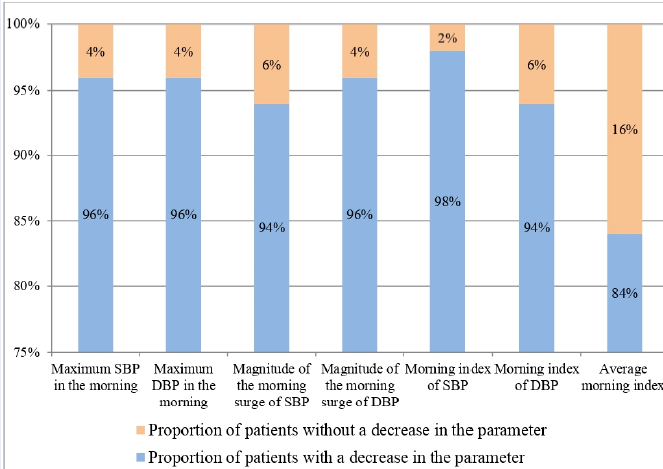
To determine the effect of telmisartan therapy on morning BP, we analyzed changes in BP from 6.00. to 11.00 with the calculation of the magnitude and speed of the morning BP surge and the morning index. Significant dynamics were found in the values of the maximum morning SBP — decrease from (177.0 ± 3.7) to (153.9 ± 2.4) mm Hg (-23.1 mm Hg in average, p < 0.001). For the maximum morning DBP, there was a decrease from (102.3 ± 2.7) to (85.1 ± 1.6) mm Hg (-17.2 mm Hg in average, p < 0.001). It was determined that the majority of patients had a decrease of each of these indicators in the dynamics (Figure 3). Particularly, a decrease in the maximum morning SBP and DBP was found in 96% of patients, a decrease in the morning surge magnitude (MSM) of SBP was observed in 94%, a decrease in MSM DBP was seen in 96%, a decrease in the morning SBP index in 98%, a decrease in morning DBP index in 94%, and a decrease in the average morning index in 84% of patients.
Since it was found that 8 (16%) patients did not have reductions of the mean morning index, further analysis of anamnestic, clinical and functional parameters of these individuals (group I) compared with patients with positive dynamics of the mean morning index (group II) was performed (Table 2). Some trends were identified. In particular, in group II there were more men — 47.6% compared to group I (37.5%). Patients were slightly older — on average (64.3 ± 2.8) years compared to (57.4 ± 3.2) in group I. In group II, there were more people with AH of 3st degree (61.9%) and the duration of AH was 15.5 ± 4.5 years, while in group I the corresponding values were 37.5% and 9.1 ± 4.1, respectively (p > 0.05).
It should be noted that there was a high frequency of comorbid pathology in group II: 64.3% of patients had CHD, 28.6% had MI in anamnesis, 47.6% had DM, and 33.3% had chronic obstructive pulmonary disease (COPD). However, in group I, the share of patients with concomitant diseases was slightly lower: 37.5% of people had CHD, 12.5% had MI, and 37.5% had DM. In addition, in group II, 61.9% of patients were obese while in group I, there were only 37.5% of such patients (p = 0.11).
Patients with a decrease in the morning index, according to EchoCG, tended to have lower detectable LVEF – (51.6 ± 2.8)% compared to (56.1 ± 1.9)% in the group where the decrease of morning index did not occur (p = 0.14). In general, in 22 (52.4%) people in group II, a reduced LVEF was diagnosed, while among the examined patients of the other group, there were only 2 people (25%) with reduced LVEF. No significant difference in the size of the left chambers of the heart was found: the size of the left atrium was (38.3 ± 1.4) cm in group I versus (38.2 ± 1.8) cm in group II (p = 0.97), the ESS of LV was (3.3 ± 0.9) cm in group I versus (3.4 ± 0.8) cm in group II (p = 0.81), and the EDS of the LV was (5.9 ± 1.2) cm versus (6.1 ± 1.0) cm, respectively (p = 0.52).
To determine the factors that have the greatest impact on the changes of the mean morning index of patients receiving telmisartan therapy, we performed a discriminant analysis with step-by-step inclusion of signs (Table 3).
The connection between the decrease in the average morning index and each of the following was established: the presence of LV hypertrophy on ECG (Wilks' Lambda = 0.65, p = 0.016), LV EDS over 6.0 cm (Wilks' Lambda = 0.65, p = 0.017), LVEF below 52.3% (Wilks 'Lambda = 0.61, p = 0.045), total cholesterol level over 5.5 mmol/l (Wilks' Lambda = 0.69, p = 0.005), LDL level over 3.3 mmol/l (Wilks 'Lambda = 0.63, p = 0.024), and triglyceride level above 2.0 mmol/l (Wilks' Lambda = 0.62, p = 0.035). Therefore, these parameters can be identified as predictors of the decrease in the morning index during 12 weeks of telmisartan therapy.
After discriminant and correlation analysis, no association of the decrease in the morning index with anamnestic data, sex and age characteristics, the presence of concomitant pathology and the stage of AH was found.
| Characteristic | All patients, n=50 | Group І, n=8 | Group ІІ, n=42 | P |
|---|---|---|---|---|
| Men, abs, % | 23 (46%) | 3 (37.5%) | 20 (47.6%) | 0.18 |
| Women, abs, % | 27 (54%) | 5 (62.5%) | 22 (52.4%) | 0.18 |
| Average age, years | 62.4 ± 1.7562.5 (54;69) | 57.4 ± 3.257 (48;71) | 64.3 ± 2.864.5 (55;69) | 0.12 |
| H 1st degree, abs,% | 3 (6%) | 1 (12.5%) | 2 (4.7%) | 0.39 |
| H 2nd degree, abs, % | 18 (36%) | 4 (50%) | 14 (33.3%) | 0.37 |
| H 3rd degree, abs, % | 29 (58%) | 3 (37.5%) | 26 (61.9%) | 0.19 |
| Average duration of AH, years | 15.5 ± 210 (7;23) | 9.1 ± 4.19 (6;14) | 15.5 ± 4.515.2 (7;17) | 0.07 |
| DM, abs, % | 23 (46%) | 3 (37.5%) | 20 (47.6%) | 0.67 |
| CHD, abs, % | 30 (60%) | 3 (37.5%) | 27 (64.3%) | 0.21 |
| MI, abs, % | 13 (26%) | 1 (12.5%) | 12 (28.6%) | 0.18 |
| Carotid atherosclerosis, abs,% | 22 (44%) | 3 (37.5%) | 19 (45.2%) | 0.67 |
| Obliterating atherosclerosis of the vessels of the lower extremities, abs,% | 12 (24 %) | 0 | 12 (28.6%) | 0.08 |
| Stroke, abs, % | 7 (14%) | 0 | 7 (16.7%) | 0.11 |
| CKD, abs, % | 27 (54%) | 4 (50%) | 23 (54.7%) | 0.054 |
| Obesity, abs, % | 29 (68%) | 3 (37.5%) | 26 (61.9%) | 0.11 |
| COPD, abs, % | 14 (28%) | 0 | 14 (33.3%) | 0.06 |
| Body mass index, kg/m2 | 32.3 ± 132 (29;37) | 29.5 ± 2.228 (26;35) | 32.2 ± 1.432 (28;36) | 0.76 |
| Creatinine, mkmol/l | 103.5 ± 2.3107 (90;115) | 101.2 ± 3.5101 (93;115) | 99.7 ± 4.2100 (89;115) | 0.79 |
| Glucose, mmol/l | 6.2 ± 0.266.1 (5;6,9) | 5.7 ± 0.495.8 (5;6,4) | 6.0 ± 0.526.1 (5;6,6) | 0.54 |
| Total cholesterol, mmol/l | 5.7 ± 0.275.6 (4.7;6.5) | 5.4 ± 0.455.4 (5.4;6.2) | 5.6 ± 0.385.5 (4.2;6,0) | 0.57 |
| LDL, mmol/l | 3.1 ± 0.212.9 (2.3;3.6) | 3.1 ± 0.183.2 (2.4;3.5) | 3.4 ± 0.43.4 (2.5;3.8) | 0.28 |
| HDL, mmol/l | 1.3 ± 0.121.2 (1.14;1.6) | 1.2 ± 0.181.2 (0.9;1.9) | 1.3 ± 0.151.3 (1.1;1.8) | 0.54 |
| Triglycerides, mmol/l | 2 ± 0.271.67 (1.2;2.1) | 1.9 ± 0.392.0 (1.3;2.4) | 2.0 ± 0.152.1 (1.3;2.3) | 0.47 |
| GFR, ml/kg/1,73m2 | 60.7 ± 3.358 (48;67) | 60.5 ± 2.860 (51;79) | 61.4 ± 4.262 (48;77) | 0.34 |
| Number of patients with hypercholesterolemia, abs, % | 37 (74%) | 6 (75%) | 31 (73.8%) | 0.23 |
| Number of patients with hypertriglyceridemia, abs,% | 20 (40%) | 3 (37.5%) | 17 (40.5%) | 0.34 |
| Number of patients with dyslipidemia, abs,% | 46 (92%) | 8 (100%) | 38 (90.5%) | 0.85 |
| Number of smokers, abs,% | 16 (32%) | 3 (37.5%) | 13 (30.9%) | 0.34 |
| Burdened history of AH, abs,% | 20 (40%) | 1 (12.5%) | 19 (45.2%) | 0.09 |
| Number of patients with AF, abs,% | 22 (44%) | 4 (50%) | 18 (42.8%) | 0.87 |
| Number of patients with LV hypertrophy, abs,% | 46 (92%) | 7 (87.5%) | 39 (92.8%) | 0.79 |
| Heart failure (HF) with preserved LVEF (over 50%), abs,% | 26 (52%) | 6 (75%) | 20 (47.6%) | 0.15 |
| HF with reduced LVEF (over 50%), abs,% | 24 (48%) | 2 (25%) | 22 (52.4%) | 0.15 |
| LA, mm | 38.3 ± 1.5 | 38.3 ± 1.4 | 38.2 ± 1.3 | 0.97 |
| EDS LV, sm | 6.06 ± 1.0 | 5.9 ± 1.2 | 6.1 ± 1.0 | 0.52 |
| ESS LV, sm | 3.37 ± 0.79 | 3.3 ± 0.9 | 3.4 ± 0.8 | 0.81 |
| EDV LV, sm | 144.6 ± 4.1 | 143.9 ± 4.2 | 144.7 ± 5.2 | 0.91 |
| ESV LV, ml | 83.9 ± 4.1 | 85.7 ± 4.8 | 83.5 ± 4.6 | 0.84 |
| LVEF, % | 52.4 ± 1.12 | 56.1 ± 1.9 | 51.6 ± 2.8 | 0.14 |
| Parameter | Wilks' - Lambda | р-value | Critical level of indicator |
| LV hypertrophy (ECG) | 0.652 | 0.016 | 1 (presence of sign) |
| EDS of LV, sm | 0.651 | 0.017 | 6.0 |
| LVEF, % | 0.615 | 0.045 | 52.3 |
| Total cholesterol, mmol/l | 0.697 | 0.005 | 5.5 |
| LDL, mmol/l | 0.638 | 0.024 | 3.3 |
| Triglycerides, mmol/l | 0.624 | 0.035 | 2.0 |
Discussion
This study herein, which was performed in 50 patients with different degrees of AH, showed high efficacy of telmisartan in antihypertensive therapy regimens. Moreover, the important findings of this study are the clinical, functional and laboratory characteristics which predict the morning response to telmisartan treatment.
Telmisartan-based hypotensive therapy significantly reduced 24-h SBP and DBP, index of variability of DBP, and daily index of SBP. The changes in morning indicators of BP, namely maximum morning SBP and maximum morning DBP, were significant in previously treated patients who switched to 40-80 mg telmisartan.
Previous studies have shown that telmisartan alone or in combination with other medications reduced SBP and DBP in uncontrolled treated and untreated patients and helped to achieve the target BP. Lacourcière Y. et al. after a 14-week study showed a decrease in SBP (-14.4 mm Hg), DBP (-11.0 mm Hg) in patients receiving 80 mg telmisartan daily in the morning8. The PRISMA study, which included more than 1,200 patients, also reported an effective reduction in BP during 14 weeks of telmisartan therapy, including a reduction in mean daily SBP (8.3 – 14.3 mm Hg) and morning SBP (8.6 – 13.9 mm Hg), depending on the daily profile of BP9. White W. B. et al. have demonstrated significant reductions in both the daytime (-11.8/-7.2 mmHg) and nighttime (-9.6/-5.7 mmHg) mean BP following telmisartan alone or in combination with the diuretic11. In the study of Parati G. et al., the authors showed that telmisartan (40 - 80 mg), with or without hydrochlorothiazide, significantly reduced the mean morning ambulatory BP (-8.2/-4.9 mm Hg), daytime ambulatory BP (-8.0/-4.7 mm Hg), and 24-h ambulatory BP (-7.9/-4.7 mm Hg) in previously untreated and in treated patients12. This study was most similar to ours because it did not contain the washout phase. Our data about BP-lowering levels are similar to those of other telmisartan efficacy studies. According to our results, the reduction of 24-h ambulatory BP was (-5.4/-6.9 mm Hg); all patients were previously treated.
In addition to the importance of the 24-h BP levels, the prognostic value of morning BP surge is well-known. Morning BP surge induces hemodynamic stress and is a risk factor of cardiovascular events occurring in the morning. Increased morning BP surge is defined to be associated with various factors, including aging, AH, DM, alcohol intake, smoking and stress. A series of investigations have demonstrated higher all-cause and cardiovascular mortality, regardless of the presence or absence of morning hypertension2, 4, 5, 13. It was observed that there is an increased risk of stroke by 11% per each 10 mm Hg of morning BP surge increase13.
The effect of telmisartan on morning BP was previously studied. It was found that response rates of the early morning SBP/DBP were 42.6% and 88.4%, daytime ambulatory SBP/DBP response rates were 43.2% and 89.7%, and 24-h ambulatory SBP/DBP response rates were 41.4% and 94.6%12. Previous studies have revealed that the average reduction of the early morning (post-awakening) BP in the case of telmisartan-based therapy was -11.5/-7.0 mm Hg. Some distinguishing parameters were found in patients with large morning BP surges; for example, the early morning post-awakening BP decreased by an average of -17.2/-10.1 mm Hg in this group11. According to our results, there is a significant decrease of maximum morning BP by -23.1/-17.2 mm Hg in patients who switched to telmisartan. It is also interesting to note that reduction of morning SBP surge was observed in 94% of patients, reduction of morning DBP surge in 96%, and reduction of the morning index in 84% of patients.
Telmisartan-based therapy in our study was shown to be effective in BP regulation of the most difficult-to-control contingents, namely comorbid patients with CHD, DM, obesity, dyslipidemia, and long history of AH, as well as in the elderly and subjects with pronounced signs of myocardial remodeling (e.g. LV hypertrophy and reduced LV EF). Such data can be explained by the positive effects of telmisartan on endothelial function, reduction of oxidative stress, and decrease of insulin resistance in patients with DM and metabolic disorders14, 15.
Studies have shown that there is a decrease in the level of inflammatory markers (e.g. TNF-a, CRP and IL-6) during 12 weeks of telmisartan therapy in patients with CHD and DM, as well as a reduction in fasting glucose and 2 hours after meals, compared with patients who received rational antihypertensive, antiplatelet, hypoglycemic therapy without the inclusion of telmisartan15. It is also known that in patients with DM, telmisartan can inhibit the ƴ-receptor, which is activated by peroxisome proliferator and improves blood flow in the endocrine parts of the pancreas14, 15, 16. There are new laboratory data on the effects of telmisartan on oxidative stress, myocardial ischemia, and immune response. Authors have observed an increase in catalase and superoxide dismutase expression levels under telmisartan treatment, with a decrease in injury and oxidative biomarker levels, and have concluded that telmisartan reduced oxidative stress and decreased the damage of the ischemia lesion17.
The aim of our study was also to establish simple predictors of the effect of telmisartan on morning. Similar studies have been performed for antihypertensive drugs of different groups and have found different results. The study of Abdelhady A. et al. was designed to quantitatively evaluate the efficacy and tolerability of a fixed dose combination of perindopril and amlodipine. It was found that female gender was associated with greater BP control, and older age was associated with less BP control; in contradistinction to our data, DM was associated with less BP control18.
In the GENRES study, the authors assessed the antihypertensive responses to amlodipine, bisoprolol, hydrochlorothiazide or losartan with 24-h ambulatory and office measurements. They analyzed the data according to age, body mass index, tricep skin fold thickness, waist-to-hip ratio, duration of hypertension, number of previous antihypertensive drugs, number of affected parents, blood pressure (BP) levels, and profiles during placebo periods. It was found that the BP responses to bisoprolol and losartan did not vary according to the variables. Amlodipine and hydrochlorothiazide responses were positively correlated with age, placebo BP level, and lower night-time dipping on placebo19.
Canzanello V.J. et al. have conducted research to identify predictors of systolic and diastolic BP responses to the thiazide diuretic hydrochlorothiazide and ACE-inhibitor candesartan. The significant role of gender, age, ethnicity, body size, baseline BP, baseline levels of plasma renin activity, and urinary aldosterone excretion was confirmed in predicting systolic and diastolic BP responses to the thiazide diuretic hydrochlorothiazide. The results also indicated that ethnicity, gender, body weight, pretreatment levels of BP, and plasma renin activity can predict the BP response to candesartan. The authors confirmed their hypothesis that the clinical and laboratory characteristics that predict poor BP response to hydrochlorothiazide are associated with better BP response to candesartan20.
In our opinion, studies that allow for personalized antihypertensive therapy remain relevant. Such studies are required for different groups of antihypertensive medications and their combinations. Our study was limited by a number of factors. The study included patients with different cardiovascular risks, mainly with a high or very high risk of cardiovascular complications, which are important for antihypertensive therapy. In our opinion, the majority of patients with low- and moderate-risk hypertension do not seek medical help so they are not monitored for BP and selection of antihypertensive therapy. Therefore, DBPM should be introduced more widely to detect patients with uncontrolled AH. Our study did not include patients with decompensated comorbidities; thus, the impact of these diseases on BP control was not evaluated. At the same time, the group of studied patients was heterogeneous and included patients with different degrees and stages of AH as well as various comorbidities, which in our opinion, enables the results to be closer to what is observed in real clinical practice.
Conclusions
The inclusion of telmisartan in antihypertensive therapy regimens, at a dose of 40 – 80 mg, can improve the control of BP in patients with varying degrees of AH. A significant decrease in both SBP and DBP can be observed after 12 weeks of therapy. Telmisartan therapy has shown an effect on the morning BP profile, with 84% of patients seeing a decrease in the mean morning index. Factors most associated with a decrease in the morning index during telmisartan therapy are male gender, 3rd degree of AH, concomitant CHD, DM and obesity, as well as the presence of signs of LV hypertrophy on ECG, EDS of LV, total cholesterol, LDL, and triglyceride levels.
Abbreviations
ACE: angiotensin-converting enzyme
BP: blood pressure
CHD: coronary heart disease
CKD: chronic kidney disease
COPD: chronic obstructive pulmonary disease
DBP: diastolic blood pressure
DBPM: daily blood pressure monitoring
DM: diabetes mellitus
EDS: end-diastolic size
EDV: end-diastolic volume
EchoCG: echocardiography
ESS: end-systolic size
ESV: end-systolic volume
GFR: glomerular filtration rateHDL: high density lipoproteins
HF: heart failure
IVS: interventricular septum
LDL: low density lipoproteins
LV: left ventricle
LV EF: left ventricle ejection fraction
LVMMI: left ventricle myocardial mass index
MI: myocardial infarction
MSM: morning surge magnitude
SBP: systolic blood pressure
TIVSd: thickness of the interventricular septum of the LV in diastole
TPVLVd: thickness of the posterior wall of the LV in diastole
Acknowledgments
We thank all patients for their participation in the investigation, and all staff of Communal non-profit enterprise "Vinnytsia Regional Clinical Treatment-Diagnostics Center of Cardiovascular Pathology" for help in the study.
Author’s contributions
DM Rasputina L.V. conceptualized and designed the study, pvovided data collection, approved the final manuscript as submitted. PhD Didenko D.V. carried out the initial analyses, drafted the initial manuscript, approved the final manuscript as submitted. Authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
Not applicable.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study (Protocol №130, 05.07.2017). All the participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
M.H.Smolensky
R.C.Hermida
Portaluppi
F.,
Circadian mechanisms of 24-hour blood pressure regulation and patterning. Sleep Med Rev.
2017;
33
:
4-16
.
View Article PubMed Google Scholar -
Wang
J.G.,
Kario
K.,
Chen
C.H.,
Park
J.B.,
Hoshide
S.,
Huo
Y.J.,
Management of morning hypertension: a consensus statement of an Asian expert panel. Clin Hypertens (Greenwich).
2018;
20
(1)
:
39-44
.
View Article PubMed Google Scholar -
Ostroumova
O.D.,
Smoliarchuk
E.A.,
Bondarets
O.V.,
E.E. Pavleeva,
Clinical advantages of telmisartan: pharmacokinetics, pharmacodynamics, and the ability to control blood pressure during the day. Actual issues of clinical pharmacology.
2017;
13
(4)
:
550-557
.
View Article Google Scholar -
Pierdomenico
S.D.,
Pierdomenico
A.M.,
Tommaso
R.,
Coccina
F.,
Carlo
S.,
Porreca
E.,
F. Cuccurullo,
Morning blood pressure surge, dipping, and risk of coronary events in elderly treated hypertensive patients. Am J Hypertens.
2016;
29
(1)
:
39-45
.
View Article PubMed Google Scholar -
Gong
S.,
Liu
K.,
Ye
R.,
Li
J.,
Yang
C.,
Chen
X.,
Nocturnal dipping status and the association of morning blood pressure surge with subclinical target organ damage in untreated hypertensives. J ClinHypertens.
2019;
21
:
1286-1294
.
View Article PubMed Google Scholar -
Tatasciore
A.,
Zimarino
M.,
Tommasi
R.,
Renda
G.,
Schillaci
G.,
Parati
G.,
Caterina
R.,
Increased short‐term blood pressure variability is associated with early left ventricular systolic dysfunction in newly diagnosed untreated hypertensive patients. J Hypertens.
2013;
31
:
1653-1661
.
View Article PubMed Google Scholar -
Ostroumova
O.D.,
A.I. Kochetkov,
Antihypertensive and organoprotective properties of a fixed combination of telmisartan and hydrochlorothiazide. Rational Pharmacotherapy in Cardiology.
2019;
15
(4)
:
26-32
.
View Article Google Scholar -
Lacourcière
Y.,
Neutel
J.M.,
Davidai
G.,
Koval
S.,
A multicenter, 14-week study of telmisartan and ramipril in patients with mild-to-moderate hypertension using ambulatory blood pressure monitoring. Am J Hypertens.
2006;
19
(1)
:
104-112
.
View Article PubMed Google Scholar -
Gosse
P.,
Schumacher
H.,
Effect of telmisartan vs. ramipril on 'dipping' status and blood pressure variability: pooled analysis of the PRISMA studies. Hypertens Res.
2014;
37
(2)
:
151-157
.
View Article PubMed Google Scholar -
Yusuf
S.,
Teo
K.,
Anderson
C.,
Telmisartan Randomised AssessmeNt Study in ACE iN tolerant subjects with cardiovascular Disease (TRANSCEND) Investigators. Effects of the angiotensin-receptorblocker telmisartan on cardiovascular events in high-risk patients intolerant to angiotensin-convertingenzyme inhibitors: a randomised controlled trial. Lancet.
2008;
372
(9644)
:
1174-1183
.
View Article Google Scholar -
White
W.B.,
Weber
M.A.,
Davidai
G.,
Neutel
J.M.,
Bakris
G.L.,
Giles
T.,
Ambulatory blood pressure monitoring in the primary care setting: assessment of therapy on the circadian variation of blood pressure from the MICCAT-2 Trial. Blood Pressure Monitoring.
2005;
10
(3)
:
157-163
.
View Article PubMed Google Scholar -
Parati
G.,
Bilo
G.,
Redon
J.,
SURGE Steering Committee The effects of telmisartan alone or with hydrochlorothiazide on morning and 24-h ambulatory BP control: results from a practice-based study (SURGE 2). Hypertens Res.
2013;
36
(4)
:
322-327
.
View Article PubMed Google Scholar -
Bilo
G.,
Grillo
A.,
Guida
V.,
Parati
G.,
Morning blood pressure surge: pathophysiology, clinical relevance and therapeutic aspects. Integr Blood Press Control.
2018;
11
:
47-56
.
View Article PubMed Google Scholar -
Cowan
B.R.,
Young
A.A.,
Anderson
C.,
Doughty
R.N.,
Krittayaphong
R.,
Lonn
E.,
ONTARGET Investigators Left ventricular mass and volume with telmisartan, ramipril, or combination in patients with previous atherosclerotic events or with diabetes mellitus (from the ONgoingTelmisartan Alone and in Combination With Ramipril Global Endpoint Trial [ONTARGET]). Am J Cardiol.
2009;
104
:
1484-1489
.
View Article PubMed Google Scholar -
Chen
T.,
Xing
J.,
Liu
Y.,
Effects of telmisartan on vascular endothelial function, inflammation and insulin resistance in patients with coronary heart disease and diabetes mellitus. ExpTher Med.
2018;
15
(1)
:
909-913
.
View Article Google Scholar -
Toyama K, Nakamura T, Kataoka K, Yasuda O, Fukuda M, Tokutomi Y et al. Telmisartan protects against diabetic vascular complications in a mouse model of obesity and type 2 diabetes, partially through peroxisome proliferator activated receptor-γ-dependent activity. Biochem Biophys Res Commun.
2011;
410
:
508-513
.
View Article PubMed Google Scholar -
Rodríguez-Lara
S.Q.,
Trujillo-Rangel
W.A.,
Castillo-Romero
A.,
Totsuka-Sutto
S.E.,
Garcia-Cobián
T.A.,
Cardona-Muñoz
E.G.,
Effect of telmisartan in the oxidative stress components induced by ischemia reperfusion in rats. Oxid Med Cell Longev.
2019;
2019
:
1302985
.
View Article PubMed Google Scholar -
Abdelhady A, Khader S, Sinnuqrut S, Albow A. The efficacy of perindopril/amlodipine in reaching blood pressure targets: results of the CONTROL Study Clin Drug Investig. 2016;
36
(5)
:
357-366
.
View Article PubMed Google Scholar -
Hiltunen TP, Suonsyrjä T, Hannila-Handelberg T, Paavonen KJ, Miettinen HE, Strandberg T et al. Predictors of antihypertensive drug responses: initial data from a placebo-controlled, randomized, cross-over study with four antihypertensive drugs (The GENRES Study). Am J Hypertens.
2007;
20
(3)
:
311-318
.
View Article PubMed Google Scholar -
Canzanello VJ, Baranco-Pryor E, Rahbari-Oskoui F, Schwartz GL, Boerwinkle E, Turner ST, Chapman AB. Predictors of blood pressure response to the angiotensin receptor blocker candesartan in essential hypertension. Am J Hypertens.
2008;
21
(1)
:
61-66
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 7 No 9 (2020)
Page No.: 3985-3995
Published on: 2020-09-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 5603 times
- Download PDF downloaded - 1728 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress




