Abstract
Adipose tissue contains a large numbers of stem cells. Adipose-derived stem cells (ADSC) employed in regenerative medicine. This study aimed to isolate ADSC and evaluate the safety of ADSC in mice model. Stromal vascular fraction (SVF) was collected from adipose tissue by collagenase. Then, ADSCs were isolated from SVFs by in vitro culture. ADSCs were evaluated their stemness in vitro by self-renewal potential, differentiation potential into osteoblasts, adipocytes, and chondroblasts as well as expression of some specific markers. Finally, the ADSCs were evaluated tumor formation in vivo in athymic mouse. Results showed that 100% samples of ADSCs were developed well and maintained homogeneous up to passage 10th. ADSCs were completely sterilized and could not cause tumors in athymic mouse. These initial results showed that ADSCs were safety for stem cell therapy.
Introduction
Fat tissue is often a problem in women or obese patients. However, it can be an extremely valuable cell source in regenerative medicine. Recent studies have shown that subcutaneous fat can provide large numbers of stem cells, as it is easy to obtain Wang and Dai, 2010. Collection of abdominal subcutaneous adipose tissue samples is relatively simple. For clinicians, using aspiration or minor surgery techniques saves time when patients to go to a hospital. These are also minimally invasive procedures for the patient, and a large amount of tissue can still be acquired using these techniques. Stem cell isolation from adipose tissue is not too complicated. Stem cell “crawling out” can be controlled by the enzymatic digestion of lipoaspirate by using collagenase in order to obtain a single-cell suspension of SVF cells or tissue culture. However, the effect of each method on the isolation of stem cells is different. Depending on the purpose and usage, each method has its own advantages. Specifically, if there is not much adipose tissue when patients need a large amount of stem cells, a cell-proliferating culture is an appropriate choice. In other cases, fresh stem cells are more beneficial. Collaboration between clinicians and researchers could save time and reduce costs for patients. In this study, we focused on expanding stem cells by in vitrocultures. The average yield of SVF cells was 1×105 to 2×106 cells per milliliter of fat tissue, where ADSCs formed approximately 10% of the total SVF cells Van Pham et al., 2013. Adipose tissue would therefore be a great revenue advantage compared to other stem cell sources. ADSCs, similar to other mesenchymal stem cells, possess characteristics of differentiation into bone, cartilage, fat, muscle and other tissues of the same origin Van Pham et al., 2013. ADSCs are also capable of secreting multiple factors, including: platelet-derived growth factor (PDGF), epidermal growth factor (EGF), basic fibroblast growth factor (FGF), angiogenic factors, and others Moon et al.,2012, which stimulate repair, replacing and regenerating damaged tissues.
As society develops, the number of types of diseases is increasing; the severity of these diseases is further increasing the demand for preventive and curative medicine. Extensive basic research and several clinical studies have also been conducted towards using mesenchymal stem cells to treat diseases. In particular, determining the characteristics and evaluating the safety of ADSCs has attracted attention. Despite their capacity for proliferation and differentiation, the use of ADSCs has been considered in treatment. An ADSC is a type of cell that has undergone culture in vitro; therefore criteria for safety, such as mutation capacity, in vivo carcinogenesis, and microorganism infection must be strictly controlled. Quality control standards for ADSCs, similar to those for biologicals, are necessary, whereby mandatory testing standards, such as the sterility and endotoxin tests for cultured cells should be performed. This is a part of good manufacturing practice (GMP) standards in accordance with European regulations for biologicals and pharmaceuticals. On the other hand, finding correlations between genes and cancer stem cells is a target research area that has attracted the attention of many researchers. In Vietnam, this area is developed not only in the laboratory but also in hospitals.
Construction is the standard procedure to determine the characteristics of ADSCs and has been proven safe in cells. It is the primary basis for managers and clinicians to gain easy and fast access to stem cell therapy for treatment.
Materials-methods
ADSC culture
SVF was collected using an ADSC extraction kit (Geneworld, HCMC, Vietnam) according to the manufacturer’s guidelines. Briefly, mouse abdominal adipose tissue was finely cut, and washed with Washing buffer solution 1 and Washing buffer solution 2. Super Extract was then added to the lipoaspirate to enzymatically resolve connective tissue, incubated for 30 min at 37°C, and then centrifuged for 10 min at 2500 rpm to collect the pellet. Finally, the pellet was washed with Washing buffer 3 by centrifugation at 3000 rpm for 5 min to collect the SVF cells. The SVF cells were cultured using MSCCult kit medium (Geneworld Ltd., Vietnam) and incubated at 37°C, 5% CO2 for 5 days to select the ADSCs. ADSC candidates at 70-80% confluency were subcultured using 0.25% trypsin/EDTA. The medium was re-freshed every 2 days. After three passages, the ADSC candidates were collected and used in subsequent experiments.
Differentiation into functional cells
To assess their ability to differentiate into adipose cells, ADSCs were induced in differential medium consisting of DMEM/F12 supplemented with 0.5 μM dexamethasone, 50 μM indomethacin, 1.5 μg/ml insulin, and 0.5 μM IBMX. Lipid droplet formation was observed under phase-contrast microscopy after 7 to 10 days. To confirm the differentiation into adipocytes, 0.35% Oil Red O solution was used. Fat cells turn red when stained with Oil red dye.
To confirm the osteogenic differentiation potential, ADSCs were induced in DMEM/F12 medium supplemented with 10% FBS, 1% antibiotic-antimycotic 100×, 100 nM dexamethasone, 10 mM beta-glycerol, 10 μM ascorbic acid, 20.8 mg/ml L-leucine, and 100 ng/ml LLysine. After 24 days, the cells were fixed with 4% paraformaldehyde and stained using 2% alizarin Red. All reagents were purchased from Sigma Aldrich (St. Louis, MO).
Expression of cell surface markers
Cell surface protein expression was analysed by flow cytometry using FACSCalibur (BD Bioscience). Cells were stained with anti-mouse CD14, CD34, CD44, CD45, CD90, and CD105 antibodies, and incubated in the dark at room temperature for 30 min. The cells were then washed with FACS Fluid solution and resuspended in 300 μl FACS Fluid solution at 4-8°C. At least 10,000 events were analyzed for each sample by CellQuest Pro software.
Cell proliferation assays
Cell proliferation was assessed using Roche xCELLigence System. Cells were loaded in 96-well E-plates at a density of 5000 cells/ml for 72h. The cell doubling time growth curve was analyzed using the Real-Time Cell Analyzer (RTCA).
Oct4 and Nanog gene expression
Total RNA was extracted using easy-BLUE™ Total RNA Extraction Kit (Intron) according to the manufacturer’s instructions. One microgram of RNA was reverse transcribed using PCR Master Mix 2× kit (Fermentas). The amplification process was performed with an initial denaturation at 94°C for 3 min, followed by 35 cycles of denaturation at 94°C, annealing at 59°C, and extension at 72°C, where each step lasted for 30 s. A final extension step was carried out at 72°C for 5 min and the sample was kept at 4°C. The primers used were as follows:
Oct4
Forward: 5′- ACATGAAAGCCCTGCAGAAG -3′
Reverse: 5′- AGATGGTGGTCTGGCTGAAC -3′
Nanog
Forward: 5′- AGGGTCTGCTACTGAGATGCTCTG -3′
Reverse: 5′- CAACCACTGGTTTTTCTGCCACCG -3′
GAPDH
Forward: 5′- CCCTTCATTGACCTCAACTA -3′
Reverse: 5′- CCAAAGTTGTCATGGATGAC -3′
The PCR products were separated by electrophoresis on 1.5% agarose gel (Sigma-Adrich, Louis St, MO) for 30 min and stained with ethidium bromide (Sigma- Adrich, Louis St, MO). The images were recorded using UV-Vis. 4T1 cells and fibroblasts (Fibroblast) were used as positive and negative controls.
Microbiological contaminants
The sterility testing of the cells was performed according to the guidelines of Vietnam Pharmacopoeia’s standards. The process summary is as follows: the cell suspension was passed through a 0.45 μm pore-sized sterile membrane filter, and then the membrane was washed with a dilute solvent (containing 0.1% peptone, 0.85% NaCl, 1% polysorbate). The membrane was then cut into two parts. To determine the bacterial content, one of the membrane filters was transferred to tubes containing soya bean liquid and incubated at 30–35°C. For the determination of fungal contamination, the other membrane filter was transferred to tubes containing thioglycolate liquid and incubated at 20–25°C for 4 days. Filtration and examination were performed under aseptic conditions. Positive controls were strains of Saccharomyces cerevisiae ATCC 2601 and Bacillus subtilis ATCC 6633. The negative control was sterile distilled water.
Tumor-forming ability in athymic nude mice of ASCs
ADSCs were injected into athymic mouse breast at the concentrations of 105, 106 and 107 cells in mice at three positions, respectively. 4T1 cells were used as positive controls and were injected at the site of ADSCs. Both ADSCs and 4T1 cells were injected into the mouse. Tumor formation was evaluated for the first 30 days. The experiment was repeated 3 times.
Safety of cell transplantation into animal models
ADSCs were transplanted into immunodeficient mice at a concentration of 106 cells/100 μL PBS. Lethal effects of cells on mice were evaluated for 6 months post-transplant.
Results-Discussion
Characteristics of ADSCs
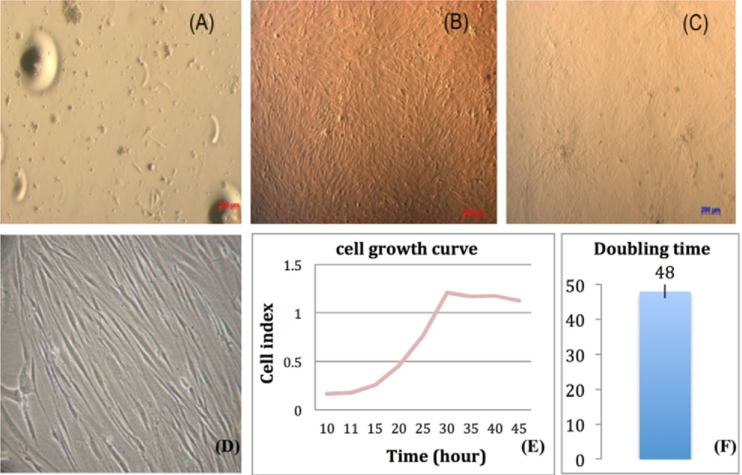
After 24 h of culture, the cells began to attach to and spread across the plate surface ( Figure 1A ). Cells reached 70-80% confluence after 5-7 days. Cell morphology changed to spindle-shaped and fibroblast-like ( Figure 1D ); the cells were relatively homogeneous by the 3rd passage ( Figure 1B ), the conditions of which were maintained until the 10thpassage ( Figure 1C ). ADSCs with adhesion and “stem” properties were retained when the medium was changed, whereas non-adherent and differentiated cells were removed. The percentage of selected cells continued to increase with each passage. In this study, cell populations became more homogeneous after 3 passages.
The results of growth curve analysis showed that the cells were in the log phase for 20-40 h ( Figure 1E ), and the doubling time of the ADSCs was 48 ± 2 h ( Figure 1F ). This result is similar to other published studies with a doubling time of 36 to 70 h Clarke et al.,2006.
Expression of cell surface markers
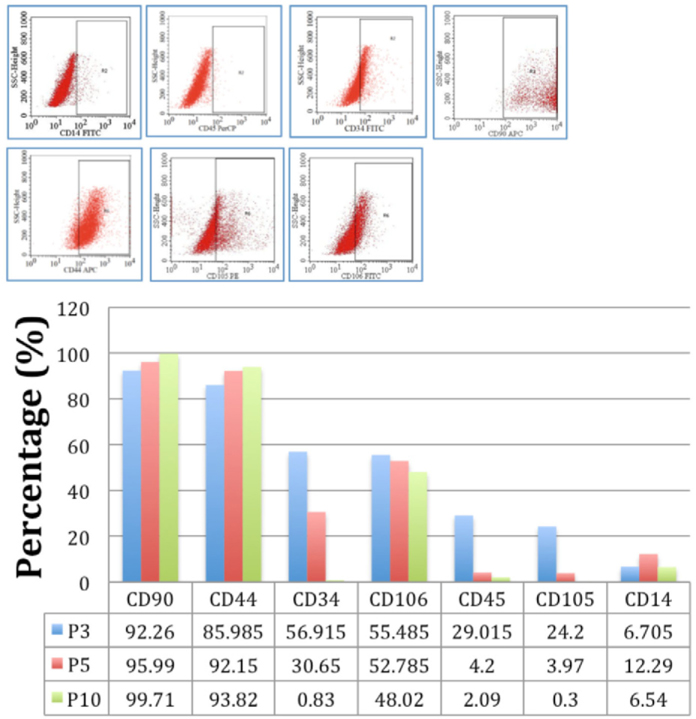
Flow cytometry analysis showed that at passage 3, the ADSCs were negative for CD14 (1.21%) and CD45 (0.24%), and were positive for CD34 (89.95%), CD44 (99.67%), CD90 (95.71%), and CD105 (80.5%) ( Figure 2A ). CD14 and CD45 are markers for mature hematopoietic cells and are not expressed in mesenchymal stem cell lines Moon et al., 2012. On the other hand, CD44, CD90, and CD105 are markers representing the adhesion of cells, an inherent characteristic of the mesenchymal cell line L, 2008. CD34 is normally expressed on hematopoietic stem cells; however, it has recently been considered a controversial hallmark for these cells. Although initially CD34 was not considered a marker of MSCs, a large number of research groups have demonstrated that ADSCs express different levels of CD34 Clarke et al., 2006Puissant et al., 2005. Expanded adipose SVF cells show strong expression of CD34; however, CD34 expression was reduced during in vitro culture. In this study, the average percentage of CD34+ cells was 30.68% at passage 5 and 0.83% at passage 10, which is in accordance with results of Boquest et al., 2005. Similarly, the expression of CD14, CD45, CD105, and CD106 also reduced during culture, whereas the expression of CD44 and CD90 increased ( Figure 2B ).
ADSCs can be differentiated into mature adipocytes and osteoblasts
The cell shape was changed when ADSCs were cultured in differential medium. After 8 days, adiposedifferentiated induced cells had shrunk and fat droplets were formatted ( Figure 3A ) and stained red with Oil Red O solution ( Figure 3B ), confirming the differentiation ability of ADSCs to functional cells. Control cultures presented no signs of mineralization ( Figure 3C ).
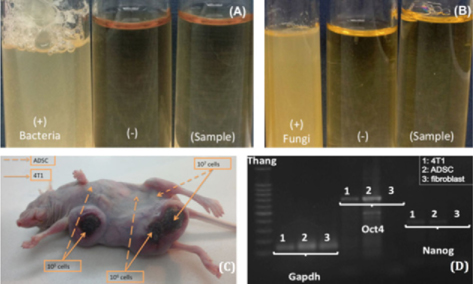
Safety of ADSCs
Sterility testing results, according to Vietnam Pharmacopoeia IV standards, showed that bacterial ( Figure 4A ) and fungal ( Figure 4B ) growth was not found in the test sample (ADSC population). For positive control samples (DC+), the culture medium was completely opaque due to the growth of bacteria, similar to the test sample and the negative controls. Microorganism infection can be clearly observed, due to sudden increases in turbidity and a color change in the culture medium Cobo et al., 2005. The cells can survive for a short time and daily observations of culture medium can determine any infection. The use of ADSCs for regenerative medicine is increasing because of their advantageous characteristics; however, for stem cell transplantation, standards are needed. In addition to the microorganisms in the host such as HIV, HBV, and HCV, it is important to control other infection sources from the external environment, such as bacteria and fungi. Nowadays, sterility testing is a part of good manufacturing practice (GMP) standards to ensure the safety of creating a clean cell source for clinical transplantation L, 2008. In this study, the cell culture process was to ensure that the cells were microbial contamination free.
The carcinogenic effect of transplanted cells is another safety indicator that is currently of interest. For the three different injected cell concentrations used —105, 106, and 107 cells per athymic mouse breast—the ADSCs did not show any ability to generate tumors. None of the ADSC-transplanted mouse breasts at all cell dosesdeveloped tumors, whereas 4T1 cells strongly expressed. After day 7, all breasts of 4T1 transplanted mice at all cell doses were tumorigenic. The tumor size grew rapidly and the mice were sacrificed on the 30th day ( Figure 4C ). Both stem cells and cancer cells possess unlimited proliferation characteristics Kondo, 2007; therefore, we focused on answering the question of whether stem cells, like cancer cells, can cause cancer in vivo. However, numerous studies have demonstrated that stem cells have the ability to control their own proliferation in the host body, whereas cancer cells do not have this ability. When stem cells were grafted into the host, they tended to migrate to the location where they originated or to the injured tissue. Here, they proliferate in sufficient quantity and differentiate to replace the damaged cells.
The regeneration stops when the healing process is complete L, 2008López-Sáez JF1, 1998. As a result, the nutrition, living space, and oxygen at the area where cancer cells resided is restricted, leading to decreasing host cell numbers. This decrease in functional cell numbers in the host body causes impairment in the function of the organ, which eventually ceases to function. In this study, only the cancer stem cell transplanted area was severely deformed by the formation of large tumors, which was contrary to what was found in the ADSC transplanted area. Thus, it was shown that ADSCs have no impact on uncontrollable proliferation when transplanted into the host body, indicating that the ADSCs do not cause cancer.
To determine if injection of both ADSCs and 4T1 cells caused the death of the mice, we performed injection of only ADSCs and evaluated its lethal effect on mice. We also assessed the expression of several 4T1 cell genes and compared to them to those in ADSCs. The results showed that, although ADSCs expressed Nanog and Oct4 genes similar to 4T1 cells ( Figure 4D ), 6 months after ADSC transplantation, all the mice remained healthy ( Figure 5 ). Oct4 is expressed in cancer stem cell like-cells, and together with Nanog, plays a vital role in tumor growth Zhang J, 2010 and control of the cancer stem cell fate during cancer development 0. However, these genes are also expressed in embryonic stem cells, and are often used as a marker for the properties of cell self-renewal and pluripotency Kondo, 2007. In this study, although cancer cell genes were expressed in ADSCs, no tumor formation or lethality in the mice was observed; therefore, Nanog and Oct4 expression should not be used as an indicator to evaluate the carcinogenic properties of ADSCs. Thus, the survival and absence of tumor formation in ADSC-transplanted mice for an extended period proved the complete safety of ADSC transplantation in vivo.
Conclusion
ADSCs strongly proliferate with a doubling time of 48 ± 2 h, during which time, the cell populations became increasingly homogeneous. ADSCs at passage 3 were positive for the markers CD34, CD44, CD90, and CD105, and were negative for hematopoietic markers CD14 and CD45. Expression of CD14, CD34, CD105, and CD106 in cells was decreased and expression of CD44 and CD90 cells was increased during in vitroculture. Moreover, ADSCs expressed some embryonic stem cell genes that are also present on cancer cells, such as Sox2 and Nanog. ADSCs were capable of differentiation into adipocytes and osteoblasts. ADSCs isolated according to this process were not the cause of tumor formation and were non-lethal and completely sterile.
References
-
A.C.
Boquest.
Isolation and Transcription Profiling of Purified Uncultured Human Stromal Stem Cells: Alteration of Gene Expression after In Vitro Cell Culture. Molecular Biology of the Cell.
2005;
16
:
1131-1141
.
-
M.F.
Clarke,
J.E.
Dick,
P.B.
Dirks,
C.J.
Eaves,
C.H.M.
Jamieson,
D.L.
Jones,
J.
Visvader,
I.L.
Weissman,
G.M.
Wahl.
Cancer Stem Cells-Perspectives on Current Status and Future Directions: AACR Workshop on Cancer Stem Cells. Cancer Research.
2006;
66
:
9339-9344
.
-
F.
Cobo,
G.N.
Stacey,
C.
Hunt,
C.
Cabrera,
A.
Nieto,
R.
Montes,
J.L.
Cortés,
P.
Catalina,
A.
Barnie,
Á.
Concha.
Microbiological control in stem cell banks: approaches to standardisation. Appl Microbiol Biotechnol.
2005;
68
:
456-466
.
-
T.
Kondo.
Stem cell-like cancer cells in cancer cell lines. Inflammation and Regeneration.
2007;
27
:
506-511
.
-
S.
L.
Clinical grade production of Mesenchymal Stem cells. 2008;
18
:
S3-S10
.
-
d.l.T.C.
López-Sáez JF1,
Giménez-Martín G
Pincheira J.
Cell proliferation and cancer. Histol Histopathol.
1998;
13(4)
:
1197-1214
.
-
K.M.
Moon,
Y.-H.
Park,
J.S.
Lee,
Y.-B.
Chae,
M.-M.
Kim,
D.- S.
Kim,
B.-W.
Kim,
S.-W.
Nam,
J.-H.
Lee.
The Effect of Secretory Factors of Adipose-Derived Stem Cells on Human Keratinocytes. IJMS.
2012;
13
:
1239-1257
.
-
B.
Puissant,
C.
Barreau,
P.
Bourin,
C.
Clavel,
J.
Corre,
C.
Bousquet,
C.
Taureau,
B.
Cousin,
M.
Abbal,
P.
Laharrague.
Immunomodulatory effect of human adipose tissue-derived adult stem cells: comparison with bone marrow mesenchymal stem cells. British Journal of Haematology.
2005;
129
:
118-129
.
-
P.
Van Pham,
K.H.-T.
Bui,
D.
Ngo,
N.
Vu,
N.
Truong,
N.L.- C.
Phan,
D.
Le,
T.
Duong,
T.
Nguyen,
V.
Le.
Activated platelet-rich plasma improves adipose-derived stem cell transplantation efficiency in injured articular cartilage. Stem Cell Research & Therapy.
2013;
4
:
91
.
-
X.
Wang,
J.
Dai.
Isoforms of OCT4 Contribute to the Confusing Diversity in Stem Cell Biology. STEM CELLS.
2010
.
-
W.X.
Zhang J,
B
Chen.
The human pluripotency gene NANOG/NANOGP8 is expressed in gastric cancer and associated with tumor development. Oncol Lett.
2010;
1
:
457-463
.
Comments
Downloads
Article Details
Volume & Issue : Vol 2 No 9 (2015)
Page No.: 359-365
Published on: 2015-09-13
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 6000 times
- Download PDF downloaded - 1846 times
- View Article downloaded - 5 times
 Biomedpress
Biomedpress