Abstract
Pain is a common aftereffect following a dental treatment, especially extractions. Hence, the main aim of the study was to compare the effect of pre-operative and post-operative analgesic usage on post-operative pain management following dental treatment. Moreover, the efficacies of three types of painkillers (Paracetamol, Ibuprofen and Mefenamic Acid) in pain relief were also evaluated. Volunteers (n = 120) who were undergoing extraction participated in this study and were randomly divided into two groups. One group consisting of 60 participants were given pre- and post-operative analgesics while another group (n = 60) received post-operative analgesics only. A visual scale was used to record pain from zero to 56 hours post-operatively at 8-hour intervals. The results showed that patients who were taking analgesics pre-operatively experienced significantly (p = 0.0045) less pain compared to those who had taken post-operative analgesics only However, a lower cumulative number of moderate and severe experiences of post-extraction pain was recorded for the pre- and post-operative analgesic treatment groups as compared to the postoperative only analgesic treatment group; no significant differences were observed. Moreover, no significant differences were observed among the analgesics used in this study as well. On the basis of these results, we conclude that preoperative analgesic usage has a positive impact on postextraction acute pain management.
INTRODUCTION
Pain increases the anxiety and suffering from patients. However, it helps clinicians to assess the condition, differentiate the causes, diagnose the root cause, and treat the cause at a much earlier stage, thereby preventing more severe problems for the patients1. Various methods have been followed to relieve pain either conservatively or post-operatively. Pain relief improves clinic outcomes2.
Up to now, several studies have been conducted to ascertain the role of pre- and/or post-operative analgesic usage on the regulation of post-operative oral pain. Hutchinson et al., in their study, showed that use of pre-operative piroxicam (40 mg) reduced doses of paracetamol in the first 24 h following recovery from anesthesia, while no opioid analgesia was required after surgical removal of lower third molars under general anesthesia3. Pre-operative single oral dose of valdecoxib also showed well-tolerated and effective analgesic effects on post-operative bunionectomy pain4. In another study, vicoprofen was reported as an effective post-operative analgesic medication in the management of acute post-operative dental pain5. The effects of pre- and post-operative ibuprofen in preventing post-operative pain has been acknowledged by several researchers6.
In the case of other surgeries, such as abdominal and thoracic surgeries, there have also been demonstrated advantages of pre-operatively administered analgesics7. However, Nagatsuka et al. did not observe pre-emptive effects from the combination of pre-operative diclofenac, butorphanol and lidocaine in the post-anesthesia care unit8. In another study, significant difference in pain control using pre-operative naproxen sodium was not observed9.
Management of pain in dentistry is challenging for both the patient and the clinician. Pain response results from the inflammatory reactions caused by tissue distortion10. Dental procedures involving teeth are generally painless unless it involves the pulp. Disturbance of the adjacent soft tissues and periodontal structures stimulates pain as well. Tooth extraction is one of the common procedure which produces inflammation and pain11. In dentistry, analgesics are prescribed to relieve acute pain, post-operative pain and chronic pain, and sometimes to control adjunctive intraoperative pain. However, there is no established protocol for its control. Though several studies have been conducted to investigate the efficacy of different types of analgesics administered pre-operatively, no study has attempted to analyze the efficacy of different analgesics, namely Paracetamol, Ibuprofen and Mefenamic Acid, in post-extraction pain management. Hence, this study aims to compare the efficacy of analgesics, such as Paracetamol, Ibuprofen and Mefenamic Acid, given pre-operatively and post-operatively in controlling post-extraction pain.
MATERIALS AND METHODS
Analgesics used
The following routinely prescribed oral analgesics were used for this study: Paracetamol (500 mg tablet), Ibuprofen (400 mg tablet) and Mefenamic Acid (500 mg tablet). Drugs were administered to patients three times a day (t.i.d).
Inclusion and exclusion criteria
This study was conducted in the Dental Clinic, Faculty of Dentistry, MAHSA University (Malaysia). The inclusion criteria for selection of the subjects included: adult age (over 18 years of age), patients indicated for extraction under local anesthesia, patients indicated for extraction under local anesthesia with adrenaline of maximum two cartridges, with no other medical complaints, and with no known contraindications for the above-mentioned drugs. On the other hand, pediatric patients, medically-compromised patients, patients with history of active peptic ulcer or ulcerative colitis, and those with history of bronchial asthma with any allergy to the above-mentioned drugs were excluded from the study.
Study design
Following provision of a signed consent form from each subject, a total of 120 subjects were enrolled in the study. Subjects were randomly divided into two main groups (group A and group B), and each group consisted of three subgroups (A1, A2 and A3, and B1, B2 and B3, respectively). Sixty participants from each group were equally divided into three subgroups (n = 20). Group A patients received analgesics both pre-operatively and post-operatively. Group B patients received drugs post-operatively only. Subgroups 1, 2 and 3 were prescribed Paracetamol, Ibuprofen and Mefenamic Acid, respectively. Visual Analog Scale (VAS) was used to evaluate the patients’ post-extraction pain until 56 hours at every 8-hour interval (Table 1). Evaluation of pain just after extraction was considered ‘0’ hour.
| Pain severity | Scale |
| No Pain | 0 |
| Mild Pain | 1-3 |
| Moderate Pain | 4-6 |
| Severe Pain | 7-9 |
| Worst Pain | 10 |
Data analysis
Data were analyzed using Pearson chi–squared ( χ2) test (SPSS version 22) and the significance level was set at p < 0.05.
RESULTS AND DISCUSSION
Among the patients who received analgesics pre-operatively (Group A), 26 reported no post-extraction pain at ‘0’ hour while only 3 reported severe pain. However, in Group B which received analgesics post-operatively only, 10 patients recorded no pain while 5 developed severe pain (Table 2). Further analysis showed a significant difference (p = 0.0045) between pre- and post-operatively treated groups in post-extraction pain control at ‘0 hour’.
| Pain Scale | Group A | Group B |
| 0 No Pain | 26 | 10 |
| 1-3 Mild Pain | 20 | 20 |
| 4-6 Moderate Pain | 11 | 25 |
| 7-9 Severe Pain | 3 | 5 |
| 10 Worst Pain | 0 | 0 |
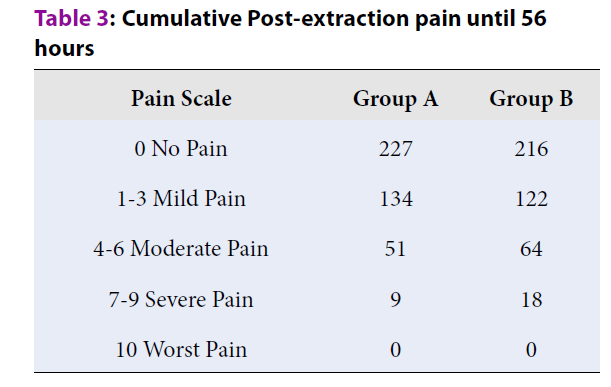
From cumulative and periodical evaluation of post-extraction pain until 56 hours, it was observed that the total number of times pain was reported by patients of Group A was lower than that of Group B. Only for 9 times did patients of Group A report severe pain, which was reported 18 times for Group B (Table 3). However, no significant difference (p = 0.151) was observed between pre- and post-operatively treated cohorts with respect to post-extraction pain control out til 56 hours.
| Pain Scale | Group A | Group B |
| 0 No Pain | 227 | 216 |
| 1-3 Mild Pain | 134 | 122 |
| 4-6 Moderate Pain | 51 | 64 |
| 7-9 Severe Pain | 9 | 18 |
| 10 Worst Pain | 0 | 0 |
Among the three medications taken in this study to evaluate pain reduction efficiency, patients with severe post-operation pain due to severe inflammatory conditions responded well with Mefenamic Acid, and followed by Ibuprofen; the lowest response was observed for aracetamol administration (Table 4).
| Scale | Group A | Group B | ||||
| A1 | A2 | A3 | B1 | B2 | B3 | |
| 0 No Pain | 9 | 8 | 9 | 3 | 4 | 3 |
| 1-3 Mild Pain | 6 | 7 | 7 | 6 | 7 | 7 |
| 4-6 Moderate Pain | 4 | 3 | 4 | 10 | 7 | 8 |
| 7-9 Severe Pain | 1 | 2 | 0 | 1 | 2 | 2 |
| 10 Worst Pain | 0 | 0 | 0 | 0 | 0 | 0 |
Post-operative pain alters or sometimes halts the normal activities of the patient, and increases suffering and anxiety. It disturbs the homeostasis of the endocrine and circulatory systems. Moreover, post-operative pain negatively influences the wound healing process12, 13. Hence, reliable and fast-onset analgesia is highly needed. This study was designed to test the currently popular belief that pre-operative measures are helpful in the prevention or modification of post-operative pain.
Even though several studies have been done on various aspects of pain management, pain remains the most sensitive and predominant issue from both the doctors’ and patients’ point of view. Many studies have been conducted on understanding the management of post-operative pain by various means of pre-operative methods, collectively referred to as pre-emptive analgesia. Prescribing analgesics to patients prior to dental treatment has proven to provide better pain control than post-operatively in many studies. In this study, we have also observed that analgesics used prior to teeth extraction have better effects on post-extraction pain control.
Immediately after any surgery, central sensitization induces excitability in the central nervous system14. In the head and neck region, inhibition of central sensitization is limited. In contrast, various post-surgical noxious inflammatory stimuli may continuously stimulate local nociceptors and induce peripheral sensitization14, which may increase the excitability of dorsal horn neurons and eventually could cause central sensitization15. Following establishment of central sensitization, patients respond poorly to analgesics16. The surgeries that are linked to the strong post-surgical inflammatory reactions usually cause sensitized severe post-operative pain. Hence, the concept of pre-emptive analgesia is introduced to prevent central sensitization before surgery to help minimize post-operative pain17.
Several randomized control studies have shown the post-operative pain inhibitory potential of pre-operative non-steroidal anti-inflammatory drugs (NSAIDs) in tooth removal. In this study, we have also observed significantly less experience of acute pain following extraction in those patients who took analgesics pre-operatively. This could be because of the inhibition of central sensitization that results from tissue damage during removal of the impacted tooth and the inhibition of peripheral sensitization that results from inflammation following tooth removal. In this study, only a few patients developed severe pain in the pre-operative group which could be due to secondary infections in patients not following the instructions or maintaining poor oral hygiene.
Conclusions
Post-operative pain is a common complication following extraction. In our study, patients prescribed with analgesics prior to dental treatment reportedly experienced lower pain level post-treatment as compared to patients prescribed only post-operatively. The types of analgesics in our study, namely Paracetamol, Ibuprofen and Mefenamic Acid, affect the post- operative pain differently. Though there were no significant differences in efficacy among the analgesics used in this study, Ibuprofen and Mefenamic Acid showed better anti-inflammatory properties compared to Paracetamol and, thus, in reducing pain levels post-operatively as well.
On the basis of the results of this study, we can conclude that in dental extraction cases, use of pre-operative analgesics may help to attenuate central sensitization while post-operative peripheral sensitization could be inhibited by administering post-operative analgesics. Moreover, this preventive analgesia method could be most effective method in controlling post-operative pain in other dental surgeries as well. Hence, for dental extractions and minor oral surgical procedures, analgesics should be given pre-operatively to mitigate post-operative pain and to reduce post-operative pain medication dosage requirement, thereby supporting a better healing process.
Abbreviations
COX: Cyclooxygenase
CNS: Central Nervous System
H0: Null hypotheses
H1: Alternative hypotheses
NSAIDs: Non-steroidal anti- inflammatory drugs
PCM: Paracetamol
Post-op: Post-operative
Pre-op: Pre-operative
t.i.d.: ter in die, three times daily
Acknowledgments
The authors would like to thank the Staff Nurses from Oral and Maxillofacial Surgery Department, supporting staffs from dental clinic and all year 5 students of 2017-2018 batch, Faculty of Dentistry, MAHSA University; and all supporting staffs from MAHSA Dental Clinic, Jalan Dang Wangi for their support in this study.
Author’s contributions
GPK conceptualized and designed the work. CSL, GEW, LWS and NFKL carried out the experiment. GPK and NH conducted formal analysis. GPK, CSL, GEW, LWS, NFKL and NH prepared the original draft. GPK and NH reviewed and edited the drafts. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The basic clinical data used to support the findings of this study are included within the article. The data used to support the findings of this study are restricted in order to protect patients privacy, but available from the corresponding author upon request. (To contact Dr. G. Padmanabha Kumar drgpk1@gmail.com)
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
-
Häuser
W.,
Perrot
S.,
Sommer
C.,
Shir
Y.,
Fitzcharles
M.A.,
Diagnostic confounders of chronic widespread pain: not always fibromyalgia. Pain reports.
2017;
2
(3)
:
e598-e
.
View Article PubMed Google Scholar -
Galicia-Castillo
M.,
Opioids for persistent pain in older adults. Cleve Clin J Med.
2016;
83
(6)
:
443-451
.
View Article PubMed Google Scholar -
Hutchison
G.L.,
Crofts
S.L.,
Gray
I.G.,
Preoperative piroxicam for postoperative analgesia in dental surgery. Br J Anaesth.
1990;
65
(4)
:
500-503
.
View Article PubMed Google Scholar -
Desjardins
P.J.,
Shu
V.S.,
Recker
D.P.,
Verburg
K.M.,
Woolf
C.J.,
A single preoperative oral dose of valdecoxib, a new cyclooxygenase-2 specific inhibitor, relieves post-oral surgery or bunionectomy pain. Anesthesiology.
2002;
97
(3)
:
565-573
.
View Article PubMed Google Scholar -
Ziccardi
V.B.,
Desjardins
P.J.,
Daly-DeJoy
E.,
Seng
G.F.,
Single-dose vicoprofen compared with acetaminophen with codeine and placebo in patients with acute postoperative pain after third molar extractions. J Oral Maxillofac Surg.
2000;
58
(6)
:
622-628
.
View Article Google Scholar -
Pozzi
A.,
Gallelli
L.,
Pain management for dentists: the role of ibuprofen. Annali di stomatologia.
2011;
2
(3-4 Suppl)
:
3-24
.
-
Dahl
J.B.,
Møiniche
S.,
Pre-emptive analgesia. Br Med Bull. 2004;
71
(1)
:
13-27
.
View Article PubMed Google Scholar -
Nagatsuka
C.,
Ichinohe
T.,
Kaneko
Y.,
Preemptive effects of a combination of preoperative diclofenac, butorphanol, and lidocaine on postoperative pain management following orthognathic surgery. Anesth Prog.
2000;
47
(4)
:
119-124
.
-
Sisk
A.L.,
Grover
B.J.,
A comparison of preoperative and postoperative naproxen sodium for suppression of postoperative pain. J Oral Maxillofac Surg.
1990;
48
(7)
:
674-678
.
View Article Google Scholar -
Chen
L.,
Deng
H.,
Cui
H.,
Fang
J.,
Zuo
Z.,
Deng
J.,
Inflammatory responses and inflammation-associated diseases in organs. Oncotarget.
2017;
9
(6)
:
7204-7218
.
View Article PubMed Google Scholar -
Renton
T.,
Dental (Odontogenic) Pain. Reviews in pain. 2011;
5
(1)
:
2-7
.
View Article PubMed Google Scholar -
Chapman
C.R.,
Tuckett
R.P.,
Song
C.W.,
Pain and stress in a systems perspective: reciprocal neural, endocrine, and immune interactions. The journal of pain : official journal of the American Pain Society.
2008;
9
(2)
:
122-145
.
View Article PubMed Google Scholar -
Pogatzki-Zahn
E.M.,
Segelcke
D.,
Schug
S.A.,
Postoperative pain-from mechanisms to treatment. Pain reports.
2017;
2
(2)
:
e588-e
.
View Article PubMed Google Scholar -
Latremoliere
A.,
Woolf
C.J.,
Central sensitization: a generator of pain hypersensitivity by central neural plasticity. The journal of pain : official journal of the American Pain Society.
2009;
10
(9)
:
895-926
.
View Article PubMed Google Scholar -
Yamaguchi
A.,
Sano
K.,
Effectiveness of preemptive analgesia on postoperative pain following third molar surgery: Review of literatures. Japanese Dental Science Review.
2013;
49
(4)
:
131-138
.
View Article Google Scholar -
Woolf
C.J.,
Chong
M.S.,
Preemptive analgesia-treating postoperative pain by preventing the establishment of central sensitization. Anesth Analg.
1993;
77
(2)
:
362-379
.
View Article PubMed Google Scholar -
Hurley
R.W.,
Enneking
F.K.,
Chapter 27 - Preemptive and preventive analgesia. In: Benzon HT, Raja SN, Liu SS, Fishman SM, Cohen SP, Hurley RW, et al., editors. Essentials of Pain Medicine (Third Edition). Saint Louis: W.B. Saunders.
2011;
:
200-205
.
View Article Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 7 No 5 (2020)
Page No.: 3794-3798
Published on: 2020-05-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 11756 times
- Download PDF downloaded - 2504 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress


