Prevalence and Associated Risk Factors of Intestinal Parasitic Infection among Underfive Children in University of Gondar Hospital, Gondar, Northwest Ethiopia
Abstract
Background: Intestinal parasitic infection is a serious health problem in developing countries mainly in children, whichleads to child mortality and morbidity. Objective: To assess the prevalence and associated risk factors of intestinal parasitic infection among underfive children in UoG Hospital.
Methodology: A cross-sectional study was conducted from May 2015 to June 2015, A total of 277 children were selected by using systematic random sampling technique. Direct wet mount and formol-ether concentration technique was used for identification of IP; also, an interview-based questioner was prepared to assess the socio-demographic status (of parents and children) and associated risk factors of those under five children.
Result: A total of 277 children [(148 (53.4%) females and 129 (46.6%) males] aged 1 year to 5 years was examined for intestinal parasitic infections. The overall prevalence of this study was 25 (9.02%) when examined by wet mount and48 (17.3%) when examined by formol-ether concentration technique. Five (1.8 %) children were infected by multiple parasites in concentration technique. Both intestinal helminthes (84%, 81.1%) and protozoan parasites (16%, 18.9%) were detected in microscopic examination with wet mount and formol-ether concentration techniques respectively. Eight species of intestinal parasites were identified. Of those, the predominant were Ascaris lumbricoides (52%, 35.8%), Hymenolepis nana (20%, 24.5%) and cyst of Giardia lamblia (12%, 9.4%) when examined by wet mount and formol-ether concentration techniques respectively. The least prevalent were Strongyloides stercoralis (1.9%).There was statistically observed association for the prevalence of IP with age, hand washing habit of parents and shortening of fingernails habit of parents.
Conclusion: The result of this study indicated that helminthic infection is more predominant than protozoan infection. Children who come from parents who had no hand washing habit and had no shortening fingernails habit were more affected by IP; therefore, Personal hygiene of parents of underfive children must be improved.
Introduction
Parasites are organisms living temporarily in or on other organisms (host Adem M,2006. The transmission to humans of some helminthes, protozoa and microsporidia is via the fecal-oral route, through direct contact with infected persons, zoonotic transmission, or by ingestion of contaminated food or water Xiao, 2010. When the water/soil is contaminated, the resilient infective forms (eggs, cysts, spores) of the pathogenic organisms can be transported to vegetables, fruit, hands, tools, handles doors, currency, etc. Nyarango et al., 2008. The hot and humid climate, high population density, poor conditions of hygiene and the presence of insects as vectors or merely as mechanic carriers of parasites, limited economic resources and some social cultural habits (food and others) promote the transmission of parasites Adeoye et al.,2007.
Parasitic infections in children are an important public health issue, particularly in developing countries. World-wide, 3.5 billion people are affected by intestinal parasites, and 450 million people, mostly children, present clinical symptoms Arani et al., 2008. It has been estimated that Ascaris lumbricoides, hookworm and Trichuris trichiura infect 1,450 million, 1,300 million and 1,050 million people worldwide, respectively. While Schistosomiasis affects over 200 million people Committee, 2002. Entamoeba histolytica and Giardia lamblia are also estimated to infect about 60 million and 200 million people worldwide, respectively Murray PR, 2002. More recently, the emerging microsporidia, especially Enterocytozoon bieneusi species has often been described as a frequent human pathogenic microorganism causing gastrointestinal infections and/or disseminated pathology, according to the species involved Lobo et al., 2012.
Like other developing countries, the prevalence of intestinal parasites is widely spread in Ethiopia. Among the common intestinal protozoan parasites Giardia, Cryptosporidium, and helminthes such as Ascarisare widely distributed Berhane,2005, where there is overcrowding, poor environmental sanitation, limited economic resources and personal hygienic practice are predisposing factors. Most of intestinal parasites are more severs in children than adults, which is associated with malnutrition, growth retardation, and poor care for children. The case is worth in underfive year children because of poor maternal hygiene, play habitats of children, in the house in close proximity to one another that create an appropriate for the transmission and spread of the disease Birhane, 2007.
Different Cross sectional study conducted elsewhere reported that the prevalence of common intestinal protozoan and helminths parasites were high. For instance, a study in Cuba reported that 104 children Giardia duodenalis was the most common parasites found, ( 54.8%) followed by Ascaris lumbricoides (6.7%), the most predominant from transmitted Helminths (STH) infections. Only 1.9% cases were infected by Entamoeba histolytica/dispar complex Cañete et al., 2012. In Pakistan, the overall prevalence of the IPIs was 52.8%, about 43% of samples contained a single parasite, and 10% contained multiple parasites. Giardia lamblia, (28.9%) and Ascaris lumbricoides(16.5%) was reported as being the most common Intestinal Parasites. In 13.9% of the Ascaris positive samples (5 out of 36) co-infection with Giardiawas also observed and this association was statistically significant Mehraj et al., 2008. In Portugal, prevalence of Intestinal Parasitic infection among children aged 0-5 years was 7.8%, and was similar among genders (6.9% in boys and 6.5% in girls Julio et al., 2012. In Nairobi, Kenya, 25.6% were positive for at least one intestinal parasite, with the common parasites, Entamoeba histolytica, 36.7%, and Giardia lamblia, 16% Mbae et al., 2013.
Another cross sectional study in Ethiopia reported that children were found to be infected with one or more intestinal parasites, 85.1% in Wondo Genet Nyantekyi et al.,2011, (36.52% and 23.47% from diarrheal children and out of non diarrheal children) in Yergalem Hospital Firdu et al., 2014, 24.3% in wonji G/hiwot et al., 2014, and 27.5% in Addis Ababa Adamu et al., 2006. A relatively high prevalence of Schistsoma mansoni was reported from Wondo Genet, 37.2%, Nyantekyi et al., 2011 and wonji, 8.8% G/hiwot et al., 2014. E. histolytica/dispar revealed higher infection in males (10.81% and 5.4%, resp.) than in females (7.32% and 2.43%, resp.); where as G. lamblia infection was higher in females (29.27%) than in males (8.11%) Firdu et al.,2014. Most of the previous studies conducted in Ethiopia have focused on the prevalence and distribution of intestinal parasitic infections mainly among schoolchildren. Only few studies have been reported the magnitude of intestinal parasitic infections among under-five children Legesse and Erko, 2005. Intestinal parasitic infection is one of the reasons for under five children mortality and morbidity, it is worse in developing countrieslike Ethiopia. Furthermore, there is limited information on the basic awareness of communities about the cause, transmission, and infection prevention in Ethiopia. Therefore, the aim of this study was to assess the prevalence and associated risk factors of intestinal parasitic infection among underfive children.
Material and methods
Study area
A cross sectional study was conducted in UoG Hospital from May 2015 to June 2015 among under five children, Gondar town, the town is found in Amhara region, North West Ethiopia 748 km far from Addis Ababa, the capital of Ethiopia and 182 km from BahirDar, central city of Amhara regional state. University of Gondar Hospital was established in 1954 in the regime of Emperor Hale Seliasse in collaboration with WHO, UNICEF & USAID to control malaria epidemic, which was occurred in Koladoba town. The hospitalgives almost all health & health related services and has four OPD and two pediatric wards. All under five year children who were attained at UoG Hospital and suspect with IP were study population.
Sample size and sampling technique
Sample size was determined using single population proportion formula: “P” was taken as 50% n=(Za/2)2.P(1−P)/_d2 Where; n=the required sample size, P=proportion of pediatric patients from the total patient (will be 0.5), a=level of confidence, z=degree of accuracy at 95%=1.96, d=margin of error=0.05. Accordingly, after correction the minimum sample size (n) was found to be 277 preschool children. Systematic random sampling technique was used to select the study population.
Data collection and laboratory method
Socio demographic Data and other information were obtained using questionnaires and each parent was interviewed in local language using interview. The stool specimens were collected by using leak proof containers from under five children and microscopic examination was performed as soon as the specimen was collected.
Wet mount microscopic examination and formol-ether concentration techniques were used to detect parasites and ligoul’s iodine was used for cyst identification. The stool specimen was examined for the presence of ova, larvae, trophozoite, and cyst of IP.
Data analysis and interpretation
The data was processed and analyzed using SPSS (Version 20) computer software program. Study findings were explained in words and tables. Proportions for categorical variables were compared using chi-square test. In all cases P-value less than 0.05 was taken as statistically significant.
Ethical consideration
Approval was secured first from the ethical clearance committee of school of biomedical and laboratory science, university of Gondar. Then a written letter from the school was obtained and submitted to chief executive officer of UoG Hospital and department of pediatrics, before verbal consent was obtained from each parents or guardian to conduct interview and collect specimen from underfive children, the objective of the study was explained. As much as possible those patients who had parasites were referred to the duty physicians in order to get appropriate anti parasitic drugs.
Results
Socio demographic characteristics
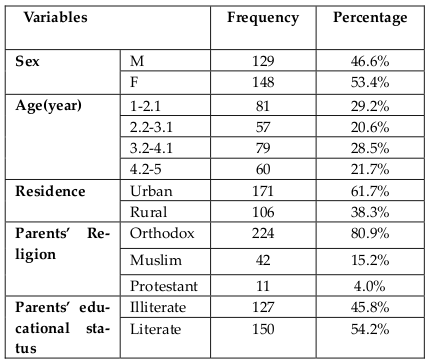
In the present study, a total of 277 under five children [(148 (53.4%) females and 129 (46.6%) males] aged 1 year to 5 years were examined for intestinal parasitic infections. From those children parents include in the study 150 (54.2%) were literate while 127 (45.8%) were illiterate ( Table 1 ).
Prevalence of IP infection
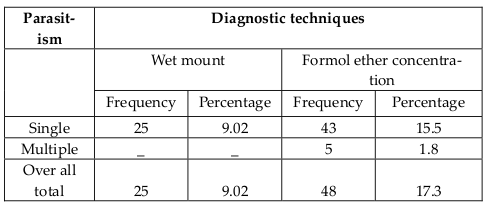
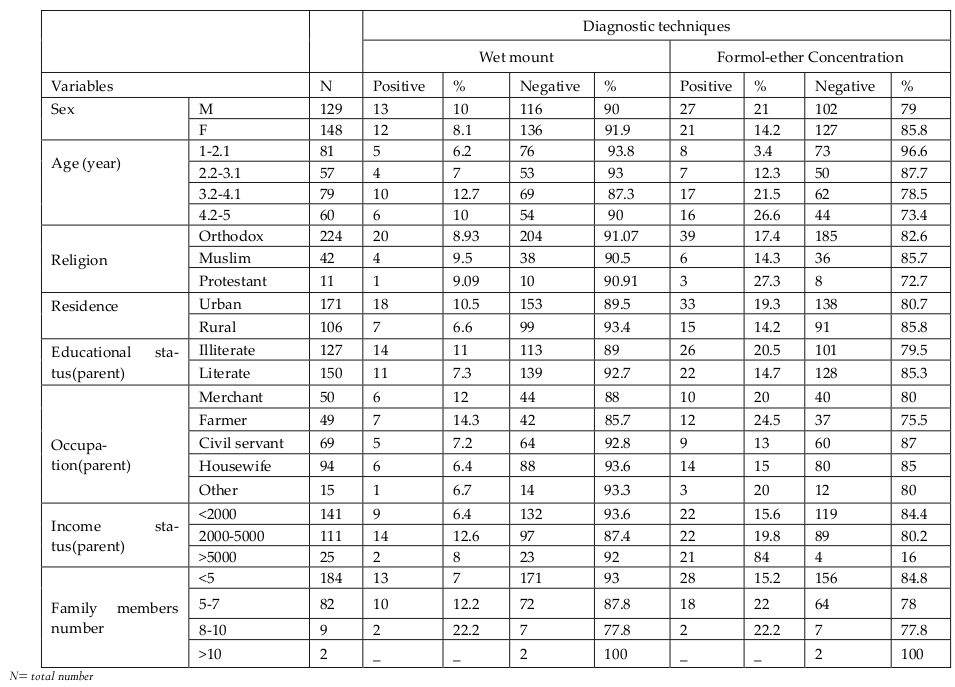
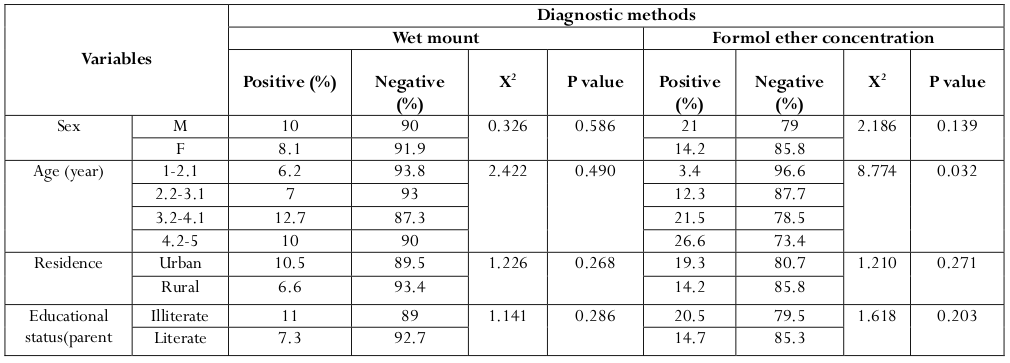
As indicated in Table 2 , the overall prevalence rate with one or more intestinal parasite was 25 (9.02%) when examined by wet mount and 48 (17.3%) when examined by formol-ether concentration technique. No Mixed infection was seen in wet mount but in formol-ether concentration technique, 5 (1.8 %) children were infected by multiple parasites. The prevalence was higher in male 27 (21%) than female 21 (14.2%) by formol-ether concentration technique and children who come from illiterate family were more infected than children from literate family. As the age increase, the prevalence was higher. At age one it was 1 (3.4 %) and at age four it become 17 (21.5 %) when examined by formol ether concentration techniques ( Table 3 ).
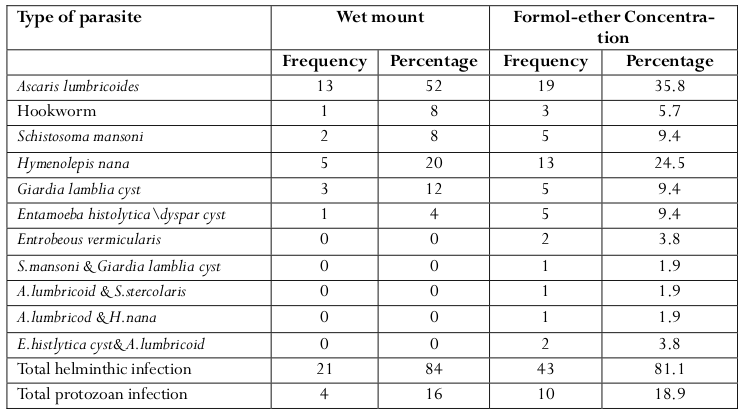
Both intestinal helminthes (84%) by wet mount, (81.1%) by formol-ether concentration and protozoan parasites (16%) by wet mount and (18.9%) by formol ether concentration techniques were detected in microscopic examination. In this study, eight species of intestinal parasites were found. Out of these (examined by fomolether concentration) the predominant were Ascaris lumbricoides 19 (35.8%), Hymenolepis nana 13 (24.5%) and cyst of Giardia lamblia5 (9.4%), the least prevalent was-Strongyloides stercoralis 1(1.9%) ( Table 4 ).
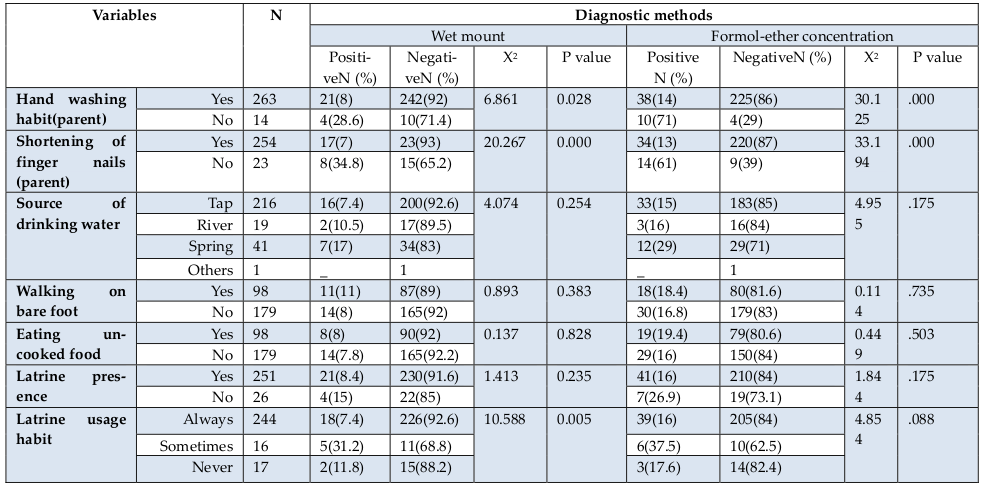
Prevalence of IP and associated risk factors
In this study no significant association was observed between the prevalence of IP by sex, (x2=2.186, p=0.139). Howevert, there was significant association with age (x2=8.774, p=0.032). However, there was statistically observed strong association between the prevalence of IP with hand washing habit of parents (x2=30.125, P=0.000), shortening of fingernail habit of children parents (x2=33.194, P=0.000) by formol-ether concentration technique. In addition, there was association between latrine usage habit and IP (x2=10.588, P=0.005) in wet mount but no association was observed in formol-ether concentration technique ( Table 5 and Table 6 ).
Discussion
In this study, the overall prevalence of one or more intestinal parasite was 17.3%. The prevalence was less than in previous studies conducted in different parts of Ethiopia namely, Wondo Genet, 85.1% (C, 2010), wonji, 24.3% G/hiwot, 2014, Yergalem Hospital, 49.5 Firdu, 2014 and Addis Ababa, 24.3%) Adamu, 2006. This study also showed low prevalence as compared with studies conducted in different parts of the world like Cuba, 58.2% Cañete, 2012, Pakistan, (52.8%) Adeoye, 2007 and Kenya (25.6%) Mbae, 2013. This difference could be due to the difference in geographical location, time of survey, diagnostic method difference and socioeconomic status.
According to the prevalence rate of each parasite species when examined by formol-ether concentration technique, Ascaris lumbricoides (35.8%) was the most predominant followed by Hymenolepis nana (24.5%) among helminthes. This finding is comparable with the study conducted in Wondo Genet (C, 2010) and Yergalem Firdu, 2014, in which Ascaris lumbricoides was most prevalent, 37.2% and 16.5% respectively. Children playing habit and the transmission way of the parasite, as this parasite is soil transmitted helminths, when children play they can easily acquire the infection. The result of Entrobeous vermicularis 2 (3.8%) was similar with study in Cuba 2 (1.9%) Cañete, 2012.
Giardia lamblia cyst and Entamoeba histolytica\dyspar cyst were highest prevalence among protozoan parasites (9.4%). This finding is supported by studies conducted in Addis Ababa (6.3%) Adamu, 2006, Pakistan (28.9%) Adeoye, 2007, Cuba (54.8%) Cañete, 2012 with prevalence of Giardia lamblia in which it was most prevalent among protozoan parasites. Entamoeba histolytica\dyspar was the least prevalent protozoan parasites inWondo Genet (0.35%) (C, 2010) and yergalem 6.09% Firdu,2014.
Considering the prevalence of Strongylodes stercoralis 1(1.9%), which was the least prevalent in our finding was also least prevalence in study conducted in Cuba 1%. Differently it was 13.2% prevalent in the study conducted in wondo Genet, Ethiopia (C, 2010). In contrast, the study conducted in Addis Ababa showed Strongylodes stercoralis was not identified Adamu, 2006. In Wondo Genet, Hymenolepis nana(4.5%) was the least prevalent (C, 2010) but in this study Hymenolepis nana was the second predominant helminthes parasite.
This study revealed that there is no significant association between sex, residence, educational status and source of drinking water for positivity of parasite but the study in Addis Ababa showed association of sex (P=0.035) with IP infection Adamu, 2006. However, there was significant association between age (x2=8.774, p=0.032) and IP infection and parents personal hygiene status (hand washing habit (x2=30.125, p=0.000) and shortening fingernails (x2=33.194, p=0.000). This showed similarity with study conducted in Pakistanin in which, there was association between hand washing habit of parents (P=0.003). Unlike this study finding there was association between parents educational status (P<0,001) and IP infection Mehraj, 2008. Similarly to this study, in Kenya statistical association between age (P<0.001) and IP infection was observed. In contrast to this study finding the study in Kenya showed association between sex (P=0.045) and IP infection Mbae, 2013.
In this study, there was difference in results between parasite detection methods (wet mount and formolether concentration techniques) according to different species of parasites. When we compare prevalence of the two methods we found that tests which were negative in wet mount become positive when examined by formol-ether concentration technique and there was 23(8.3%) difference between the prevalence of IP infection of the two techniques. This showed similarity with study conducted in Gondar, Ethiopia in which the prevalence for intestinal helminthic infection by we mount (38.4%) was increased to 57.1% by formol-ether concentration technique.
Conclusion and recommendations
The result of this study indicated that helminthic infection is highly predominant than protozoan infection, the most predominant helminth was Ascaris lumbricoid. Children at age four and males were more affected by IP.This study also demonstrate that some tests that were negative by wet mount examination become positive by formol-ether concentration technique. In the present study significant association was observed between IP infection and age, parent’s personal hygiene status (hand washing habit and shortening fingernails. The study therefore recommends improvement of personal hygiene of caregivers of under five children and for better identification of parasites, it is better to practice concentration techniques. Since some physicians treat IP suspect children clinically, we also recommend physicians to request lab tests for any IP suspected children
References
-
H.
Adamu,
T.
Endeshaw,
T.
Teka,
A.
Kifle,
B.
Petros.
The prevalence of intestinal parasites in paediatric diarrhoeal and non-diarrhoeal patients in Addis Ababa hospitals, with special emphasis on opportunistic parasitic infections and with insight into the demographic and socioeconomic factors. Ethiopian Journal of Health Development.
2006;
20
.
-
C.W.
Adem M.
Parasitology for medical laboratory students, 2nd edition edn. Addis Ababa publisher.
2006
.
-
G.O.
Adeoye,
C.O.
Osayemi,
O.
Oteniya,
S.O.
Onyemekeihia.
Epidemiological Studies of Intestinal Helminthes and Malaria among Children in Lagos, Nigeria. Pakistan J of Biological Sciences.
2007;
10
:
2208-2212
.
-
A.S.
Arani,
R.
Alaghehbandan,
L.
Akhlaghi,
M.
Shahi,
A.R.
Lari.
Prevalence of intestinal parasites in a population in south of Tehran, Iran. Revista do Instituto de Medicina Tropical de São Paulo.
2008;
50
.
-
Berhane.
Epidemiology of Health and Disease in Ethiopia. Uttar Pradesh, India: Shama Books Printing Press.
2005
.
-
Y.
Birhane.
Special report on linking reproductive health, family planning and HIV/AIDS program. 2007;
21(1)
:
1-108
.
-
R.
Cañete,
M.M.
Díaz,
R.
Avalos García,
P.M.
Laúd Martinez,
F.
Manuel Ponce.
Intestinal Parasites in Children from a Day Care Centre in Matanzas City, Cuba. PLoS One.
2012;
7
:
e5139-4
.
-
W.E.
Committee.
Prevention and control of Schistosomiasis and soil-transmitted helminthiasis. 2002;
:
1-57
.
-
T.
Firdu,
F.
Abunna,
M.
Girma.
Intestinal Protozoal Parasites in Diarrheal Children and Associated Risk Factors at Yirgalem Hospital, Ethiopia: A Case-Control Study. International Scholarly Research Notices.
2014;
2014
:
1-8
.
-
Y.
G/hiwot,
A.
Degarege,
B.
Erko.
Prevalence of Intestinal Parasitic Infections among Children under Five Years of Age with Emphasis on Schistosoma mansoni in Wonji Shoa Sugar Estate, Ethiopia. PLoS One.
2014;
9
:
e10979-3
.
-
C.
Julio,
A.
Vilares,
M.
Oleastro,
I.
Ferreira,
S.
Gomes,
L.
Monteiro,
B.
Nunes,
R.
Tenreiro,
H.
Angelo.
Prevalence and risk factors for Giardia duodenalis infection among children: A case study in Portugal. Parasites & Vectors.
2012;
5
:
2-2
.
-
M.
Legesse,
B.
Erko.
Prevalence of intestinal parasites among school children in a rural area close to the southeast of Lake Langano, Ethiopia. Ethiopian Journal of Health Development.
2005;
18
.
-
M.L.
Lobo,
L.
Xiao,
F.
Antunes,
O.
Matos.
Microsporidia as emerging pathogens and the implication for public health: A 10-year study on HIV-positive and -negative patients. International Journal for Parasitology.
2012;
42
:
197-205
.
-
C.
Mbae,
D.
Nokes,
E.
Mulinge,
J.
Nyambura,
A.
Waruru,
S.
Kariuki.
Intestinal parasitic infections in children presenting with diarrhoea in outpatient and inpatient settings in an informal settlement of Nairobi, Kenya. BMC Infect Dis.
2013;
13
:
24-3
.
-
V.
Mehraj,
J.
Hatcher,
S.
Akhtar,
G.
Rafique,
M.A.
Beg.
Prevalence and Factors Associated with Intestinal Parasitic Infection among Children in an Urban Slum of Karachi. PLoS One.
2008;
3
:
e368-0
.
-
R.K.
Murray PR,
G.S
Kobayashi.
Medical Microbiology. PfalleHA. London. Mosby.
2002
.
-
L.A.
Nyantekyi,
M.
Legesse,
M.
Belay,
K.
Tadesse,
K.
Manaye,
C.
Macias,
B.
Erko.
Intestinal parasitic infections among under-five children and maternal awareness about the infections in SheshaKekele, Wondo Genet, Southern Ethiopia. Ethiopian Journal of Health Development.
2011;
24
.
-
R.M.
Nyarango,
P.A.
Aloo,
E.W.
Kabiru,
B.O.
Nyanchongi.
The risk of pathogenic intestinal parasite infections in Kisii Municipality, Kenya. BMC Public Health.
2008;
8
:
23-7
.
-
L.
Xiao.
Molecular epidemiology of cryptosporidiosis: An update. Experimental Parasitology.
2010;
124
:
80-89
.
Comments

Downloads
Article Details
Volume & Issue : Vol 2 No 08 (2015)
Page No.: 347-353
Published on: 2015-08-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 7006 times
- Download PDF downloaded - 2303 times
- View Article downloaded - 9 times
 Biomedpress
Biomedpress