Abstract
Introduction: In the emergency department, the decisions on admission or discharge are based on clinical symptoms and physical examinations. The aim of this study is to compare the assessment of emergency physician clinical judgment accuracy with the actual amount of peak expiratory flow rate (PEFR).
Method: The present research was a cross-sectional study. In this study, 138 patients with asthma of the age of 18 to 55 years were enrolled. From admission to discharge, clinical signs and symptoms were investigated and recorded by emergency physicians and the severity of asthma was determined (mild, moderate, severe). In both stages (admission and discharge), the PEFR was measured by researcher and was compared with the severity of asthma, which are determined based on clinical symptoms and physical examination.
Results: 37.7% of patients were male and the rest were females, and the mean age of participants was 49.84 years. The number of mild, moderate and severe asthma cases was 14, 36 and 88, respectively in peak flow meter. The number of mild, moderate and severe asthma cases was 37, 32 and 69, respectively in clinical judgment. In assessment of emergency physician clinical judgment accuracy in severity of asthma in comparison with peak flowmetry, the result was the kappa value of 0.231 (P <0.001).
Conclusion: The study showed that clinical judgment of physicians in the emergency department is not a good prediction of severity of asthma.
Introduction
Asthma is a challenging disease in both hospitalized patients and outpatients. Much information exists on therapeutic intervenes, which occurred during the shift from acute phase to chronic phase of the disease. The high prevalence of the disease has created a huge burden for asthmatic patients, making life more difficult for them 1. The growing database on therapeutic interventions at the time of transition from acute to chronic phase of this disease is a rewarding step forward 2. The most important factor to reduce morbidity and mortality is the diagnosis of the acute asthma and early hospitalization of the patients. The acute asthma symptoms in initial assessment are the long and irregular checkups (as previous frequent hospitalizing, a regular dose of inspiratory beta-agonists, oral steroids, long attacks, and low or changing peak flow), clinical examinations and spirometry as the most objective instrument). Some studies name d FEV1 and PEFR as the predictive factors in discharging asthmatic patients, however, no valid document exists in this regard in emergency ward or for outpatients. Other studies stated that pulmonary performance cannot predict the patient’s relapse and recovery cycle, particularly in terms of patients with asthma. Therefore, this cannot be regarded as a definite technique. Various studies showed that the recommendations should be taken in asthmatic adults 3. The aim of this study is to assess the accuracy in clinical judgment for the severity and discharge criteria made by emergency physicians in comparison with Peak Flowmetry in patients with asthma attack.
Materials - Methods
This study is a cross-sectional study carried out at the emergency ward of Imam Reza Hospital of Mashhad from March 20th 2015 to March 20th 2016. The patients’ age was between 18 and 55 years old, and they were referred to the emergency ward for acute asthma attack. Upon entering the ward, patients were examined and assessed by a physician and their clinical symptoms such as RR, PR and O2 saturation rates, using secondary inspiratory muscles, and the rate and intensity of wheezing were recorded. Asthma severity was determined based on the symptoms and the physician's diagnosis as mild, moderate and severe. At this stage, the PEFR was measured by the researcher using the plant FERRARIS, and the asthma severity classification was performed according to the physician's opinion; which was then compared with the PEFR result. After the physician's decision for patient’s discharge, the PEFR and clinical symptoms were measured and recorded again, and the clinical criteria and correctness of the physician's judgment was compared with the PEFR.
The inclusion criteria consisted of all the patients with acute asthma attack, aged between 15 and 55 years old, asthma background prior to the visit and consent for participating the study. Exclusion criteria included patients under 15 or older than 55 years old, having frequent visits, and patients who were transferred from another hospital. Similarly, patients with COPD background or chronic bronchitis and acute asthma, who were unable to blow into the peak flow meter, were also excluded.
After completing the checklist form, the data were analyzed by SPSS16. In order to study the correlation of quantity variables, T-test and U-man-Whitney tests were used, and in case of more than two groups, one — way ANOVA and Tukey tests were used. In order to compare the data before and after treatment, paired samples t-test was used. The correlations between the data with normal and abnormal distribution were assessed using Pearson and Spearman test respectively. The P-valve< 0.05 was considered statistically significant. The level of accordance of asthma severity indicated by Peak Flowmetry and clinical judgment was assessed and validated via regression analysis. The weight K indicator was used to assess the accordance. The K indicator < 0.02 was considered as weak situation, 0.21 to 0.4 as fairly weak, and 0.41 to 0.6 as moderate, 0.61 to 0.8 as good, and higher than 0.8 as excellent.
| Variable | Type | Frequency | Percentage | PEFR | P-value | |
| Mean | SD | |||||
| Sex | Male | 52 | 37.7 | 38.3 | 13.05 | 0.207 |
| Female | 86 | 62.3 | 40.18 | 6.55 | ||
| Wheezing | Inspiratory | 0 | 0 | - | - | <0.001 |
| Expiratory | 61 | 44.2 | 44.52 | 11.93 | ||
| Inspiratory- expiratory | 77 | 55.8 | 24.59 | 2.76 | ||
| Secondary muscle use | Yes | 75 | 54.3 | 38.13 | 5.82 | 0.254 |
| No | 63 | 45.7 | 40 | 12.6 | ||
| Asthma severity based on PEFR | Mild | 14 | 10.2 | 65.1 | 9.85 | <0.001 |
| Moderate | 36 | 26 | 46.9 | 6.87 | ||
| Severe | 88 | 63.8 | 31.8 | 3.2 | ||
| Clinical decision | Mild | 37 | 26.8 | 66.12 | 12.46 | <0.001 |
| Moderate | 32 | 23.2 | 45.19 | 2.73 | ||
| Severe | 69 | 50 | 30.13 | 2.65 | ||
Results
52 patients (37.7%) were males, and 86 patients (62.3 %) were female. The mean age of the patients was 49.84 years old. The PEFR percentage comparison in both males and females (38.3% and 40.18%, respectively) using t-test did not indicate a significant difference (P=0.207). Wheezing was expiratory for 61 individuals (44.2%) and inspiratory-expiratory for 77 individuals (55.8%). The PEFR values in the group with expiratory wheezing (average of 44.53%) were significantly higher than the inspiratory-expiratory group (average of 34.59%) (P<0.001) (Table 1). Secondary inspiratory muscles were used in 54.3% of patients; however, The PEFR value was not significantly different in patients and the patients with no distress (P =0.254). The numbers of mild, moderate and severe asthma in Peal Flowmetry were 37, 32 and 69, respectively (Table 1). The mean percentages of PEFR in the mild, moderate and severe asthma indicated by Peak Flowmetry were 65.1, 46.9 and 31.8, respectively, and those in the mild, moderate and severe asthma indicated via clinical judgment of the physician were measured as 66.12, 45.19 and 30.13, respectively. In both methods, the PEFR difference was significant among the various types of asthma. Based on reference 11, a PEFR value of ≤ 40 percent indicates a severe asthma and if it is between 40 and 60 percent, asthma would be moderate, and for the values higher than 60 percent, the asthma would be classified as mild.
| Variables | Severe asthma | Moderate asthma | Mild asthma | ||||||
| Before | After | P-value* | Before | After | P-value* | Before | After | P-value* | |
| PEFR | 31.8 | 57.31 | <0.001 | 46.9 | 60.69 | <0.001 | 65.1 | 73.23 | <0.001 |
| Breathing | 30.6 | 18.23 | <0.001 | 24.6 | 15.34 | <0.001 | 19 | 15.5 | <0.001 |
| Heart rate | 117.3 | 91.68 | <0.001 | 108.7 | 78.47 | <0.001 | 75.5 | 70 | <0.001 |
| O2 saturation | 86.25 | 94.2 | <0.001 | 86.2 | 95.39 | <0.001 | 89 | 94.54 | <0.001 |
The average PEFR value of patients before performance of the study was 39.11 percent, which changed to 59.36 percent after treatment.
Regarding sex distribution and wheezing type, the difference was significant in mild, moderate and severe types of asthma (P<0.001); however, in terms of the use or absence of secondary inspiratory muscles, significant difference was not observed. Using secondary muscles was found in 52.5%, 65.2% and 50 % of patients before treatment, while no patient with inspiratory distress was found after treatment.
The rate of inspirations in the three groups was recorded as 30.6, 24.6 and 19, and the mean heart rate were 117.3, 108.7 and 75.5. Tukey test analysis showed that both numbers of inspiration and heart rate were higher in severe asthma than moderate and mild asthma (P=0.004 for comparison of heart beat in moderate and severe asthma and P<0.001 for other cases) and higher in moderate asthma than mild type (P<0.001)
The average diastolic blood pressures were 85.91, 73.4 and 75, which was significantly higher in the group with severe asthma than in moderate asthma (P= 0.007); however, in comparison of the severe and mild asthma (P= 0.074) and the moderate and mild (P=0.963) the differences were not significant.
O2 saturation was also recorded in three groups as 25, 86, 86.2 and 89, respectively. No difference was found between the severe and moderate asthmas, but it was significantly higher in the mild group than in the two other groups (P=0.015 and P=0.049, respectively, in comparison with the severe and moderate asthma).
The average PEFR percentages in the severe, moderate and mild asthmas were indicated as 31.8, 46.9 and 65.1, respectively before treatment and 57.31, 69.60 and 73.23. The PEFR values were significantly higher after treatment than those before treatment. In the three asthma groups, the number of inspirations had been reduced significantly after the treatment in comparison with before the treatment (P<0.001). The average heart rate in the three groups were 117.3, 108.7 and 75.5, respectively before the treatment, and after the treatment the values were recorded as 91.68, 78.47 and 70 respectively, which was reduced significantly using the Paired t-test (P<0.001). The O2 saturations in the three groups were found to be 86.25, 86.2 and 89, respectively before the treatment, and 94.2, 95.39 and 94.54 after the treatment, indicating significant increase in three groups following treatment (P<0.001) (Table 2).
| Clinical judgment | Asthma severity | ||
| Severe | Moderate | Mild | |
| Mild | 14 | 16 | 7 |
| Moderate | 0 | 6 | 26 |
| Severe | 0 | 14 | 55 |
Regarding the similarity rate of physicians' clinical judgment and Peak Flowmetry results in indicating the asthma severity, the Kappa test result was calculated as 0.231 (P<0.001) (Table 3).
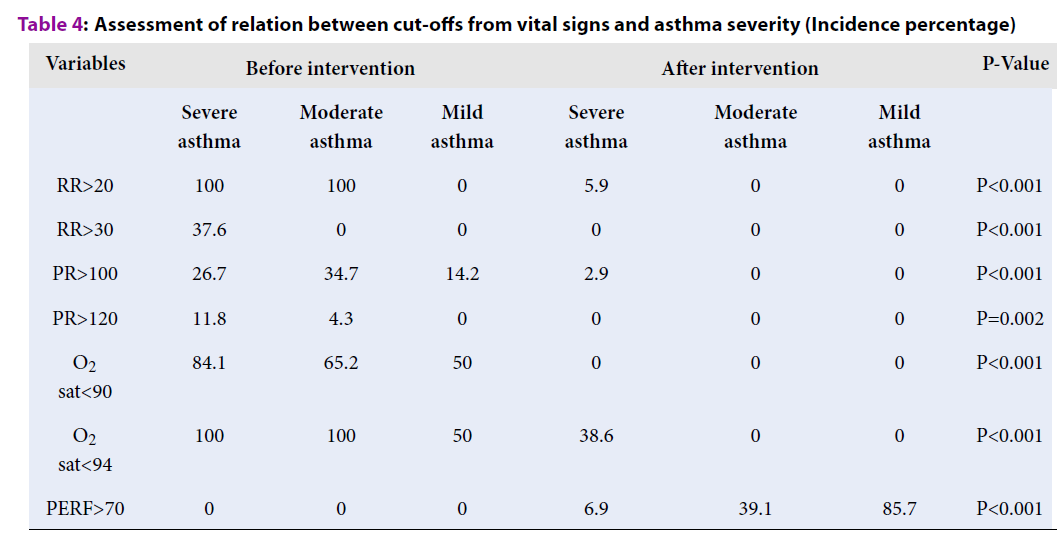
| Variables | Before intervention | After intervention | P-Value | ||||
| Severe asthma | Moderate asthma | Mild asthma | Severe asthma | Moderate asthma | Mild asthma | ||
| RR>20 | 100 | 100 | 0 | 5.9 | 0 | 0 | P<0.001 |
| RR>30 | 37.6 | 0 | 0 | 0 | 0 | 0 | P<0.001 |
| PR>100 | 26.7 | 34.7 | 14.2 | 2.9 | 0 | 0 | P<0.001 |
| PR>120 | 11.8 | 4.3 | 0 | 0 | 0 | 0 | P=0.002 |
| O2 saturation<90 | 84.1 | 65.2 | 50 | 0 | 0 | 0 | P<0.001 |
| O2 saturation<94 | 100 | 100 | 50 | 38.6 | 0 | 0 | P<0.001 |
| PERF>70 | 0 | 0 | 0 | 6.9 | 39.1 | 85.7 | P<0.001 |
An analysis of the several numbers as cut-off points for the existing variables and their function in diagnosing the asthma severity revealed that in one case, RR > 20 was observed in all patients with severe and moderate asthma before the treatment, while it does not exist in patients with mild asthma. All the RRs > 30 (38 cases) occurred in patients with severe asthma. Aft er the treatment, the RR values > 20 existed in only 6 percent of patients with severe asthma (5.9 percent), and the RR higher than 30 was not found (Table 4).
| Variables | Correlation rate | P-value* |
| PEFR - Age | -0.082 | 0.34 |
| PEFR - Heart rate | -0.696 | <0.001 |
| PEFR Breathing rate | -0.49 | <0.001 |
| PEFR Systolic BP | 0.036 | 0.686 |
| PEFR Diastolic BP | -0.069 | <0.001 |
| PEFR - O2 saturation | 0.422 | <0.001 |
The RR >100 was found in 27 patients with severe asthma (26.7 percent), 8 patients with moderate asthma (34.7 percent) and 2 patients with mild asthma (14.2 percent) before treatment, and only 3 patients (2.9 percent) with severe asthma after the treatment. The RR value above 120 was seen in only 12 patients (11.8 percent) with severe asthma and in a single patient with moderate asthma before treatment and in no patient after treatment. Oxygen saturation below 90 was found in 85 patients (84.1 percent) with severe asthma, 15 patients with moderate asthma (65.2 percent) and 7 patients (50 percent) with mild asthma before the treatment. It was not observed in any patients after the treatment. Oxygen saturation below 94 was found in all patients with severe and moderate asthma and 7 patients (50 percent) with mild asthma, but it was seen only in 39 patient s (38.6 percent) with severe asthma after the treatment. The PERF values above 70 was seen in 12 patients (85.7 percent) with mild asthma, 9 patients with moderate asthma (39.1 percent) and 7 patients (6.9 percent) with severe asthma after treatment; a fact which shows that out of the 138 total cases, 28 cases had the PEFR value of 70% at the time of discharge.
On the other hand, during patients’ discharge, the final clinical decision of the physician was the complete recovery in all 138 patients. By reviewing the correlation between PEFR value and clinical judgment of patients (Table 5), the Kappa value of 0.074 (0.912) was found, which indicates the low accordance rate of the two criteria at the time of patient’s discharge.
Discussion
Asthma attack is one of the most frequent and most difficult cases at emergency departments, which requires the physician’s decision on whether it is an outpatient or in-hospital case. There is disagreement regarding the patient’s discharge. Different studies have suggested various solutions for this issue, but the results are inconsistent4.
With the current costs of hospitalization and morbidity associated with the disease, it is crucial to separate accurately the in-hospital treatment from outpatients.
In current study, the accordance rate of physicians' clinical judgment in indicating the severity of patients with acute asthma before treatment was compared with the results from Peak Flowmetry; based on the obtained results, it can be concluded that the clinical judgment is probably not a good criterion for indicating asthma severity. In a study conducted by Tomita et al., it was confirmed that the asthma severity cannot be decided via clinical judgment 5.
The REF values less than 30% (less than 120 L/min) and a FEV1<25% indicate a severe asthma. The physical signs and symptoms are consistent with the Spiro metric rates; however, the range of these symptoms are so wide that they cannot be used alone. The severe asthma patients, who are diagnosed on the first visit, should be referred to the hospital. The patients can be discharged if they recover in the first several hours and remain stable clinically with a PEF value of PEF>75% 6.
Some agreements exist on signs and symptoms of asthma, which may help diagnose deadly asthma attack. For instance, diaphoresis and inability to lie down in supine situation are related to hard blocking of air stream, which is measured by REF. The increased HR is associated with asthma severity.
The wheezing is minimally related to measuring the air path block and is a poor predictor for hospitalization need.
By and large, lack of wheezing in patients with dyspnea or a changed consciousness is an alarming sign, which may change by modifying the air path in order to respond to treatment.
Aldana et al. 3 reviewed the arterial O2 saturation rate and the peak expiratory flow as the risk factors for critical condition in children with asthma. The asthmatic attack is one of the most common cases at emergency departments in children. Their study is a predictive, linear, comparative and observational plan, which was performed on 50 children (20 girls and 30 boys) between 6 and 18 years old with previous mild asthma attack. In the study, the rate of arterial O2 saturation and the peak expiratory flow was assessed in 30 minutes, 2, 4, and 24 hours after treatment with inspiratory albuterol (nebulizer). After treatment intervention, a significant difference was found in the rate of arterial oxygen saturation in 2, 4 and 24 hours and 24 hours after treatment. The authors concluded that the rate of arterial oxygen saturation is a better predictive factor than the peak expiratory flow in asthmatic attacks in children 3.
In another study, Fernández et al. 7 investigated the functionality of oxygen saturation and the peak expiratory flow in assessing the severity of acute asthma and the predictive value of the two factors for hospitalizing conditions of patients. In their cohort study, 123 children, who were referred to the emergency ward following asthma diagnosis, were included in the study. The rate of arterial O2 saturation and the peak expiratory flow were recorded at the time of attendance, after receiving treatment and before discharge or hospitalization. The rate of O2 saturation before and after treatment reduced significantly in the in-hospitalized children in comparison with the discharged patients. This was similar for peak expiratory flow. The 95% O2 saturation had a sensitivity and specificity of 83% and 81% respectively. It was concluded that the rate of O2 saturation and the peak expiratory flow can be used as suitable instruments for predicting the consequent treatment for children with acute asthma 7.
Sole et al. 8 examined the oximetric pulse function in assessing the severity of acute asthma and wheezing in children. They examined 174 children with acute asthma signs or wheezing. The clinical signs and patients’ spirometric findings were compared with the rate of O2 saturation measured by oximetric pulse. 74 children in asthma clinics and 100 children in the emergency ward were assessed regarding acute asthma, wheezing treatment and clinical scoring was measured based on their existing signs. Among patients in asthma clinics, 58 patients were able to take pulmonary tests and the rates of FEV1 and FEF25-75 were determined. The results showed that there is a significant relationship between the reduction of clinical signs points and increase of O2 saturation rate in the treatment with bronchodilators in both groups. There was also a significant relationship between SpO2 level and the values of FEV1 and FEF25-75. On the other hand, SpO2 level had a reverse relation with clinical scoring and heart rate. The obtained results demonstrated that clinical point higher than 3 and SpO2<94% are correlated with the increase in asthma attack severity and can be used as a predicator and indicator of the severity of asthma attack and wheezing 8.
In the current study, it was indicated that, at the time of discharge, only 28 out of 138 patients had a PEFR level of 70% as expected.
Based on the existing resources 9, patients can be discharged from the emergency department only if their PEFR reaches the expected level of 70%; thus, it can be concluded that the clinical judgment is not a trusted criterion for the discharge of asthmatic patients from the emergency department. Therefore, based on the study conducted, we suggest that the physician’s clinical judgment is correct neither for indicating the severity of the asthma, nor for the discharge of the acute asthmatic patient from the emergency department. In order to decide that, further research in varied statistical population is warranted.
The rate of O2 saturation in the three groups of severe, moderate and mild asthma increased significantly following the treatment. Among the variables studied after treatment, heart rate had a significant reverse relation with the PEFR rate, and the rate of O2 saturation had a reverse poor correlation with the PEFR rate. However, the inspiration rate had no significant relationship with the PEFR rate. At the time of discharge, 110 patients out of 138 patients, had not reached the expected 70% PEFR or higher; thus, measuring PR, RR, O2 saturation and other clinical signs in this study cannot be considered as reliable criteria for deciding about the patients’ discharge. In order to use the clinical signs, such as PR, RR and O2 saturation as the criteria, further studies should be performed, in which the PEFR rate reaches the expected 70% in each patient.
In the current study, 11.8% of the severe asthma cases with PR > 120 and 37.6% of the patients with severe asthma had the RR rate higher than 30. Since PR>120 and RR>30 are specific to patients with severe asthma, their existence can suggest the severe cases. In the study of Silverman et al. 10 on RA, it was demonstrated that only 15% of the patients with acute asthma had tachycardia rate higher than 120 per minute and less than 20% of the patients had RR rate higher than 20 per minute.
Based on a review study by Rodrigo GJ, the severity of airflow obstruction cannot be accurately judged by patient’s symptoms and physical examination alone11. Accordingly, it is important to use an objective measure of airway obstruction (spirometry or peak flow meter). Although spirometry can be performed in acutely ill emergency department asthmatics, measurement of peak expiratory flow, with values expressed as predicted normal values, represents an alternative if spirometry is not available.
Peak expiratory flow rate measured at 15-60 min of treatment, coupled with continuous monitoring of oxygen saturation may be the best ways to assess patients with acute asthma 11.
Conclusions
The results indicate that the physicians’ clinical judgment and any of the vital signs such as inspiration rate, heart rates and the rates of O2 saturation cannot be a valid criterion for assessing the severity of asthma in patients attending the emergency department. However, based on the correlation between RR, PR and O2 saturation with PEFR rates, these vital signs can be suggested as criteria for classifying the severity of asthma. In order to reach an acceptable criteria for assessing the severity of asthma, further research in larger statistical population is needed. The results of the study revealed that the physician’s clinical judgment cannot be a correct criterion for discharging an asthma patient from the emergency department and for a scientific and correct discharge, the pulmonary function needs to be assessed with Peak Flowmetry and/or spirometers.
Abbreviations
ANOVA: Analyze of variance
COPD: Chronic Obstructive Pulmonary Disease
ED: Emergency Department
HR: Heart rate
PEFR: Peak expiratory flow rate
PR: Pulse rate
RR: Respiratory rate
Competing Interests
The authors report no conflicts of interest in this work.
Authors' Contributions
MD Sharif conceptualized and designed the study, H Feiz Disfani contributed in data collection and managing analysis, HR Rahmatzadeh collected the Data and Contributed in writing and approving the study. Finally, all authors approved the manuscript.
Acknowledgment
The authors of this study are grateful to all the personnel of Imam Reza Hospital as well as the Vice-Chancellor for Research, Mashhad University of Medical Sciences, for their contribution to the implementation of this research projects.
References
-
Longo
D,
Fauci
A S,
Kasper
D L,
Hauser
S,
Jameson
J L,
Loscalzo
J,
Harrisons manual of medicineMcGraw Hill Professional 2012.
Google Scholar -
Markoff
B A,
Macmillan
J F,
Kumra
V,
Discharge of the asthmatic patient. Clinical reviews in allergy & immunology.
2001;
20
(3)
:
341-55
.
View Article PubMed Google Scholar -
Ortiz
I A,
Arreguín
L O,
García
R C,
Arterial oxygen saturation versus peak expiratory flow as predictive values in the course of asthmatic crises in children. Revista alergia Mexico (Tecamachalco, Puebla, Mexico: 1993).
1997;
44
(6)
:
158-61
.
-
Corre
K A,
Rothstein
R J,
Assessing severity of adult asthma and need for hospitalization. Annals of emergency medicine.
1985;
14
(1)
:
45-51
.
View Article PubMed Google Scholar -
Tomita
K,
Hanaki
K,
Hasegawa
Y,
Watanabe
M,
Sano
H,
Igishi
T,
Underrecognition of the severity of asthma and undertreatment of asthma in a rural area of Japan. Journal of Asthma.
2005;
42
(8)
:
689-96
.
View Article PubMed Google Scholar -
Bolliger
C,
Perruchoud
A,
Acute severe asthma: emergency diagnostic and therapeutic measures. Schweizerische medizinische Wochenschrift.
1992;
122
(48)
:
1823-30
.
PubMed Google Scholar -
Benito
J F,
Mintegui
S R,
Snchez
J E,
Montejo
M F,
Soto
E P,
Usefulness of oxygen saturation and peak expiratory flow in the management of acute asthma. Anales espanoles de pediatria.
1996;
45
(4)
:
361-4
.
PubMed Google Scholar -
Sole
D,
Komatsu
M,
Carvalho
K,
Naspitz
C,
Pulse oximetry in the evaluation of the severity of acute asthma and/or wheezing in children. Journal of Asthma.
1999;
36
(4)
:
327-23
.
View Article PubMed Google Scholar -
Wardhani
R P,
Pengaruh Pemberian Ekstrak Daun Binahong (Anredera cordifolia (Tenore) Steenis) terhadap Reepitalisasi Kulit Pasca Luka Bakar Derajat II Tikus Sprague dawleyFKIK UIN Jakarta .
Google Scholar -
Silverman
R A,
Flaster
E,
Enright
P L,
Simonson
S G,
FEV1performance among patients with acute asthma: results from a multicenter clinical trial. Chest.
2007;
131
(1)
:
164-71
.
View Article PubMed Google Scholar -
Rodrigo
G J,
Predicting response to therapy in acute asthma. Current opinion in pulmonary medicine.
2009;
15
(1)
:
35-8
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 6 No 10 (2019)
Page No.: 3405-3411
Published on: 2019-10-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6204 times
- Download PDF downloaded - 1880 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress

