Seroprevalence of typhus fever at the Kality Prison, Addis Ababa, Ethiopia
Abstract
Background: Peoples living in crowded situations like refugee camps and prisons are highly vulnerable to louse-born typhus infection. The information on the prevalence of louse-borne typhus among prisoners in Ethiopia is limited. Hence, the aim of this study was to determine the prevalence of typhus among prisoners at the Kality Prison, Addis Ababa, Ethiopia.
Methods: A five year retrospective study was conducted from February to March 2014. A total of 6104 typhus fever suspected prisoners tested for typhus at the Kality Prison Hospital from 2008 to 2012 were included. Data on the seroprevalence of typhus were abstracted from Kality Prison Laboratory. Data were entered and analyzed using SPSS 20 statistical software. Descriptive statistics and Chi-square were computed. In all cases p-values less than 0.05 was taken as statistically significant.
Results: The overall prevalence of typhus fever infection was 26.3%. The prevalence of typhus fever infection was found to be higher among prisoners within the age group of 41-50 years (36.9%) and also among male patients (27.3%). The prevalence of typhus fever infection was higher by the year 2009 (40.7%) and overall in the five-year period the summer (31.8%) and fall (30%) seasons showed higher seroprevalence of typhus.
Conclusions: The prevalence of typhus fever infection at Kality prison was high. This high prevalence could be a possible risk for epidemic typhus fever infection within the prison and for the nearby population. Therefore, targeted public health intervention could be important in this high risk population.
Background
Typhus is a bacterial disease caused by the genus Rickettsia. Epidemic typhus is a louse-borne disease caused by Rickettsia prowazekii and endemic typhus caused byRickettsia typhi is transmitted by fleas Gunther, 1935Weissmann, 2005. Epidemic typhus transmitted to humans through the body louse primarily occurs in areas of over population and people with lower socioeconomic condition Fournier et al., 2002 which favors infestation of the vectors Azad, 1998. Fever, nausea, muscle pain, and headaches are among the symptoms of epidemic typhus disease. The occurrence of pink rash on the extremities followed on the stomach and buttocks after few days of infection are also observed Renesto et al., 2005.
Epidemic typhus can cause death in up to 40% of untreated cases and frequently occurs in areas where poverty, lack of hygiene, and cold weather favor the proliferation of lice. The prevalence of louse-born typhus fever infection highly depends on the socio-economic level of a society Fang et al., 2002. Furthermore, louse-borne epidemic typhus continues to strike tens to hundreds of thousands of persons who live in sub-Saharan Africa with civil war, famine, and poor-hygienic conditions Parola,2006.
Typhus fever disease has been well-known several centuries ago. However, it remains as a major public health problem among peoples living in poor-hygiene conditions which might result due to war, social disruptions, poverty, or gaps in public health management. Poor-hygiene conditions favor a higher prevalence of body lice, which are the main vectors for this disease. Outbreaks of epidemic typhus have occurredin jails and refugee camps in developing countries Badiaga and Brouqui, 2012. Therefore, survey of louse-borne diseases in areas where there are overcrowded populations could possibly help to design and implement specific strategies and set public health priorities. Prisons are expected to have poor-hygienic conditions that facilitate vector born disease such as typhus fever. Therefore, this study was aimed to assess the prevalence of typhus fever at the Kality Prison, Addis Ababa, Ethiopia.
Methods
The study was conducted at the Kality Prison which is located in the southern parts of Addis Ababa, Ethiopia. It is the biggest prison in Ethiopia and hosts for about 4000 prisoners. The prison has a clinic and a hospital. The clinic gives service only for prisoners whereas the hospital serves both staffs and high risky prisoners. A retrospective study was conducted from February to March 2014 to assess a five years prevalence of typhus fever among prisoners. At the Kality Prison clinic and hospital all typhus fever suspected prisoners are tested for typhus. Weil-Felix serological test was used to diagnose typhus fever infection. A total of 6104 typhus fever suspected prisoners tested for typhus at the Kality Prison clinic and hospital from 2008 to 2012 were included for the study. Data on the seroprevalence of typhus andsocio-demographic parameters, age, sex and seasons, were abstracted from Kality Prison Laboratory records.
The ethical clearance of the study was obtained from the ethical review committee of the School of Biomedical and Laboratory Sciences, University of Gondar, Ethiopia. Official written permission letter was obtained from the higher management of the Kality Prison. Confidentiality of the result was secured and the name of the client registered in the hospital was coded and blinded during data collection and analysis.
Data entry and analysis was done using SPSS version- 20 software. A descriptive analysis was used to determine socio-demographic characteristics and seroprevalence of typhus. The differences in proportions were tested by the chi-square test. Significance levels were chosen at 0.05 level with a two-tailed test.
Results
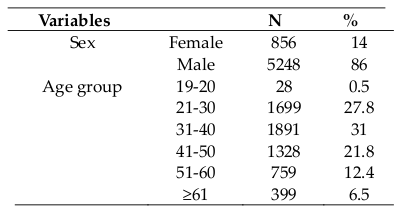
A total of 6104 prisoners were examined for seropositivity of syphilis between 2008 and 2012. The majority of prison patients 5248 (86%) were males. The mean age of the study subjects were 38.83 (SD ± 11.75) years and the highest proportion 1891 (31%) of the prisoners were within the age of 31-40 years ( Table 1 ).
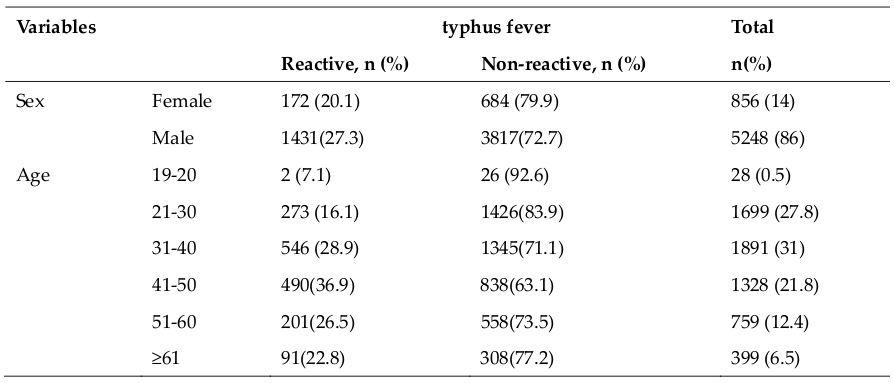
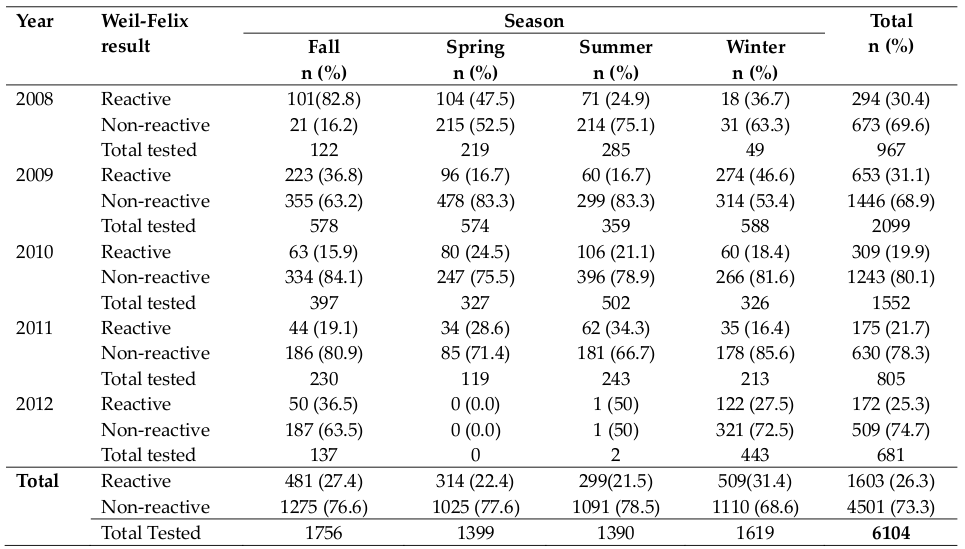
Out of 6104 typhus fever suspected prisoners, 1603 (26.3%) were positive (reactive) for typhus fever. The prevalence of typhus fever among male and female cases were 1431/5248 (27.3%) and 172/856 (20.1%) respectively. The higher proportion of typhus fever positive cases 1603 (89.3%) were among male prisoners compared with female prisoners (10.7%). The upper most prevalence of typhus fever infection was observed in the age group of 41-50 years which was 490 out of 1328 clients (36.9%) ( Table 2 ). However, the differences in the prevalence of typhus fever among different age and sex groups were not statistically significant. The number of patients suspected of acute febrile illness was different from year to year. Year based data showed 967, 2099, 1552, 805, 681 patients’ demonstrated sign and symptoms for acute febrile illness in the years 2008, 2009, 2010, 2011 and 2012, respectively. The prevalence of typhus fever among prisoners was 30.4%, 31.1% 19.9% 21.7% and 25.3% in the consecutive five years ( Table 3 ). Moreover, chi-square (χ2) test statistical analysis showed that typhus fever infection was significantly associated with season (p<0.001).
The numbers of prisoners tested for typhus fever were 1756, 1399, 1390 and 1619 during the fall, spring, summer and winter seasons respectively. The prevalence of typhus fever was 27.4%, 22.4%, 21.5% and 31.4% during the fall, spring, summer and winter seasons respectively. In this study higher prevalence of typhus fever was observed during the winter season ( Table 3 ).
Discussion
Epidemic typhus is one of the highly prevalent diseases in developing countries. Epidemic typhus is considered primarily a disease of war, and has made a significant contribution to human history Raoult et al., 2006. It is still prevalent in areas where poor socioeconomic conditions and a high prevalence of louse infestations exist. The recent circulation or distribution of epidemic typhus is indefinite but since the 1990s, foci of epidemic typhushave been described in Africa, including Algeria Mokrani et al.,2004 and central eastern African countries such as Ethiopia, Zaire, Rwanda and Burundi Perine et al., 1992, in mountainous regions of South America (including Peru), in mountainous or highland regions of North America, in the Himalayan regions in Asia, and in Russia Tarasevich et al., 1998. An autochthonous case of epidemic typhus has been recently reported in France Badiaga and Brouqui, 2012.
Typhus fever was once called "goal fever" or "ship fever;" because it was common in prisons and on ships that had been at sea a long time. The reason is that lice that hold typhus fever causing organism are widespread in large aggregations of persons who do not clean or change clothes with any regularity and are forced by conditions to live in close accommodations. These are also the conditions that refugees and prisoners are likely to find themselves. The lice adhere to the ridge of clothes, in chains, on the edge, or on any other space that provides them a hiding place. They shift from one person to another at a haphazard manner. Simple acts, such as unintentional brushing against, provisional lend of clothing, or simple closeness especially at night can lead to a migration from one person to another. Lice will make a mass migration from a person when death overtakes their host and the rapidly cooling body forces them to find a more hospitable environment David, 2014. Parasitic body lice can serve as a vehicle for transmission of typhus in the community. Since the persistence of the vector enabled the spread of Rickettsia from human carriers back to the louse population, the disease is mostly prevalent in peoples living in poverty and overcrowded conditions. Prisons are among the wellknown living areas that expose peoples to different types of vector born and other communicable diseases. Since Rickettsia survives in insects prisoners are expected with high exposure for infection by these bacterial agents. The incarcerated time of the prisoners may also have significant relationship for the disease. There could be also other factors such as the hygienic environments, the number of prisoners in a unit of prison, the availability of insecticides, and the general health of each prisoner.
In the current study the overall prevalence of epidemic typhus was 26.3%. In a study conducted in a Jail in Burundi, among 9 patients who were tested for Rickettsia, all patients exhibited antibodies specific for R. prowazekii Raoult et al., 1998. The prevalence of typhus fever infection in Kality prison was by far higher than a community based study report from Sierra. In that study, Didier et al reported 16.7% typhus fever infection prevalence in four villages of Peruvian Sierra communities Raoult et al.,1999. There are also reports that showed as high as 18.8% and as low as 2% prevalence of typhus fever infection in Mexico and Algeria respectively Kamarasu et al., 2007Raoult, 1997. The occurrence of epidemic typhus in circumstances where people are interned under poor hygienic conditions should be regarded as a marker for the general social situations. If these indicators are ignored, the consequences could be disastrous. In Burundi, small outbreaks among inmates in prison preceded a nationwide epidemic that afflicted over 45,000 people Raoult et al., 1998.
The prevalence of typhus fever infection was higher among male patients in the present study. Similar study conducted in Jimma, South west Ethiopia, revealed typhus fever preponderance among male patients Mekasha and Tesfahun, 2004. In the current study, epidemic typhus was more prevalent among patients within the age group 41 to 50 years. However, different studies reported that a wide range of age groups (2 to 58 years) were found infected by Rickettsia prowazekii. Some reports showed that all age groups are at risk for Rickettsia infections but patients over 60 years of age have the highest risk of death Eremeeva, 2012.
In the current study the prevalence of epidemic typhus was 30.4% by the year 2008 but a comparatively higher prevalence (31.4%) was observed by the year 2009 in the same prison. A decrease in the prevalence of typhus fever infection (19.9%) was also observed by the year 2010. During the other two consecutive years (2011 and 2012), there was a slight decrease in the prevalence of typhus fever infection (21.7% and 25.3% respectively) in Kality prison. The decreased prevalence of epidemic typhus might be due to improvement of preventive and control mechanisms of the disease. Epidemic typhus was first considered a disease restricted to the human being, with human to human transmission occurring via the human body louse (Pediculushumaniscorporis). The possibility of recurrent infection in humans (referred to as Brill- Zinsser disease) suggested that man may act as a reservoir for the bacteria and explained the maintenance of the disease between epidemics (Raoult and Maurin). However, R. prowazekii has been recently isolated from flying squirrels (Glaucomysvolans) in North America Bozeman et al., 1975, and the disease (referred as indigenous epidemic typhus) may be acquired from flying squirrel-parasitizing arthropods. It has also been found in Amblyomma ticks in Ethiopia and Mexico Parola et al., 2005. Therefore, traditional preventive methods such as the application of insecticide and delousing should be supported with additional and new methods that possibly prevent the transmission of Rickettsia from other sources.
Another important finding in this study was that a higher prevalence of typhus fever found during the fall and winter seasons. This might be due to cold climatic condition of the seasons which favors the transmission of Rickettsia prowazekii. Most cases of epidemic typhus occur during the cold months, when heavy clothing and poor sanitary conditions allow infestation by body lice. There are reports that documented highest infection rate in May as compared to July, August, and October in Denmark (Raoult and Maurin). The limitations of the current study were that data on educational status and incarcerated time were not registered in the laboratory registration book. Moreover, we were unable to observe the overall situation of the prison and most importantly, the prisoner’s hygiene and the number of inmates in each part of the prison.
Conclusion
The current study showed a high prevalence of typhus fever infection among prisoners at Kality Prison. Prisoners infected by typhus fever could be the possible source for an epidemic to occur among the prison community and the general population at large. An outbreak of typhus fever infection presents an enormous threat to the future health of the population of the region, since a very large reservoir of R prowazekii could be established. Since the overall prevalence of epidemic typhus is high in Kality Prison, it is important to strengthen the prevention and control measures such as insecticide application and health education. Long-term prevention and control strategies that address the underlying preconditions of this problem are needed.
Authors’ contributions
Both MW and BG conceived the study and participated in its design. MW performed the data collection and statistical analysis. BG prepared the manuscript for publication. All authors read and approved the final manuscript.
References
-
A.
Azad.
Rickettsial Pathogens and Their Arthropod Vectors. Emerg Infect Dis.
1998;
4
:
179-186
.
-
S.
Badiaga,
P.
Brouqui.
Human louse-transmitted infectious diseases. Clinical Microbiology and Infection.
2012;
18
:
332-337
.
-
F.M.
Bozeman,
S.A.
Masiello,
M.S.
Williams,
B.L.
Elisberg.
Epidemic typhus rickettsiae isolated from flying squirrels. Nature.
1975;
255
:
545-547
.
-
W.
David.
Typhus fever on the eastern frontin World War I. 2014
.
-
M.
Eremeeva.
Rickettsial (Spotted & typhus fevers) & related infections (Anaplasmosis & ehrlichiosis). 2012
.
-
R.
Fang,
L.
Houhamdi,
D.
Raoult.
Detection of Rickettsia prowazekii in Body Lice and Their Feces by Using Monoclonal Antibodies. Journal of Clinical Microbiology.
2002;
40
:
3358-3363
.
-
P.-E.
Fournier,
J.-B.
Ndihokubwayo,
J.
Guidran,
P.J.
Kelly,
D.
Raoult.
Human Pathogens in Body and Head Lice. Emerg Infect Dis.
2002;
8
:
1515-1518
.
-
C.
Gunther.
Endemic typhus in New Guinea. Med J Aust.
1935;
1
:
813-814
.
-
K.
Kamarasu,
M.
Malathi,
V.
Rajagopal,
K.
Subramani,
D.
Jagadeeshramasamy,
E.
Mathai.
Serological evidence for wide distribution of spotted fevers & typhus fever in Tamil Nadu. Indian Journal of Medical Research.
2007;
126
:
128
.
-
A.
Mekasha,
A.
Tesfahun.
Determinants of diarrhoeal diseases: a community based study in urban south western Ethiopia. E Af Med Jrnl.
2004;
80
.
-
K.
Mokrani,
P.E.
Fournier,
M.
Dalichaouche,
S.
Tebbal,
A.
Aouati,
D.
Raoult.
Reemerging Threat of Epidemic Typhus in Algeria. Journal of Clinical Microbiology.
2004;
42
:
3898-3900
.
-
P.
Parola.
Rickettsioses in Sub-Saharan Africa. Annals of the New York Academy of Sciences.
2006;
1078
:
42-47
.
-
P.
Parola,
C.D.
Paddock,
D.
Raoult.
Tick-Borne Rickettsioses around the World: Emerging Diseases Challenging Old Concepts. Clinical Microbiology Reviews.
2005;
18
:
719-756
.
-
P.L.
Perine,
B.P.
Chandler,
D.K.
Krause,
P.
McCardle,
S.
Awoke,
E.
Habte-Gabr,
C.L.
Wisseman,
J.E.
McDade.
A Clinico- Epidemiological Study of Epidemic Typhus in Africa. Clinical Infectious Diseases.
1992;
14
:
1149-1158
.
-
D.
Raoult.
Jail Fever (Epidemic Typhus) Outbreak in Burundi. Emerg Infect Dis.
1997;
3
:
357-360
.
-
D.
Raoult,
R.J.
Birtles,
M.
Montoya,
E.
Perez,
H.
Tissot-Dupont,
V.
Roux,
H.
Guerra.
Survey of three bacterial louseassociated diseases among rural Andean communities in Peru: prevalence of epidemic typhus, trench fever, and relapsing fever. Clinical infectious diseases.
1999;
29
:
434-436
.
-
D.
Raoult,
O.
Dutour,
L.
Houhamdi,
R.
Jankauskas,
P.E.
Fournier,
Y.
Ardagna,
M.
Drancourt,
M.
Signoli,
Vu D.
La,
Y.
Macia.
Evidence for Louse‐Transmitted Diseases in Soldiers of Napoleon’s Grand Army in Vilnius. The Journal of Infectious Diseases.
2006;
193
:
112-120
.
-
D.
Raoult,
M.
Maurin.
Rickettsia prowazekii (Epidemic Typhus and Brill-Zinsser Disease).
.
-
D.
Raoult,
J.B.
Ndihokubwayo,
H.
Tissot-Dupont,
V.
Roux,
B.
Faugere,
R.
Abegbinni,
R.J.
Birtles.
Outbreak of epidemic typhus associated with trench fever in Burundi. The Lancet.
1998;
352
:
353-358
.
-
P.
Renesto,
H.
Ogata,
S.
Audic,
J.-M.
Claverie,
D.
Raoult.
Some lessons from Rickettsia genomics. FEMS Microbiology Reviews.
2005;
29
:
99-117
.
-
I.
Tarasevich,
E.
Rydkina,
D.
Raoult.
Outbreak of epidemic typhus in Russia. The Lancet.
1998;
352
:
1151
.
-
G.
Weissmann.
Rats, Lice, and Zinsser. Emerg Infect Dis.
2005;
11
:
492-496
.
Comments

Downloads
Article Details
Volume & Issue : Vol 2 No 07 (2015)
Page No.: 318-323
Published on: 2015-07-27
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 10021 times
- Download PDF downloaded - 2074 times
- View Article downloaded - 4 times
 Biomedpress
Biomedpress