Abstract
Objective: To assess balance function in patients with radiologically confirmed otosclerosis. Methods: Sixteen patients (14 females and 2 males), who attended the Neuro-Otology clinic/ ENT clinics at the Royal National Throat Nose and Ear Hospital, participated in this study. After general medical, audiological and Neuro-Otological examination, patients underwent the caloric and rotational testing.
Results: Thirteen of the 16 patients had radiologically confirmed otosclerosis (12 females and 1 male). A total of 3 patients (2 females and 1 male) did not have CT confirmation of otosclerosis, and therefore, were excluded from the study. The remaining 13 patients' data were analyzed. Nine patients had a mixed hearing impairment at least on one side, while eight patients had a bilateral mixed hearing loss and one patient had a sensorineural hearing loss on one side. Four patients had a bilateral sensorineural hearing loss. Only 1 patient had a canal paresis (CP) at 35 %. None of the patients had any significant directional preponderance (DP). The patient with significant CP (35%) did not show any rotational asymmetry on impulsive rotation. Eleven patients had a rotational chair test. Only one patient had a significant asymmetry to the right at 25.30% (normal range is <20%). Overall, 18% (n = 2) of the radiologically confirmed otosclerosis patients showed an abnormal balance test, including both caloric and rotational tests. More than 80% (n = 9) of the patients with radiological otosclerosis showed balance symptoms.
Conclusions: the current study indicates a high prevalence of balance symptoms (n = 9 or 82%) in patients with radiological otosclerosis, although only a small proportion (n = 2 or 18%) showed an abnormal vestibular function on caloric and impulse rotation testing. However, due to a small number of samples, further validation of this result is warranted.
Introduction
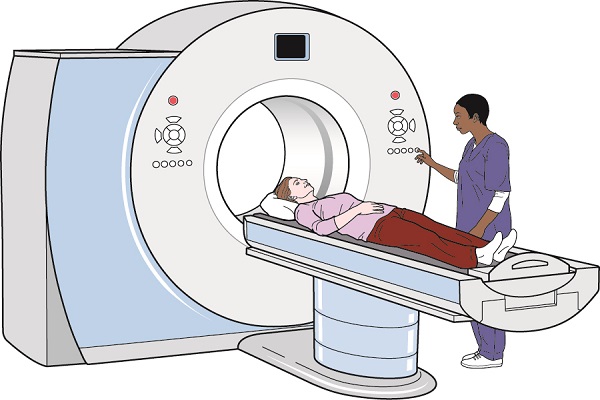
Balance function studies in otosclerosis were carried out mainly in the early and late 70s, when the diagnosis of this condition was based essentially on audiometric findings without any radiological confirmation. It is, therefore, possible that the incidence of balance disorder reported in otosclerosis may not be a true reflection of the problem. We conducted this study to assess balance function in patients with radiologically (CT scan) confirmed otosclerosis, including both patients with fenestral and cochlear diseases.
In addition to typical conductive hearing loss, patients suffering from otosclerosis often have a perceptive hearing loss. Cochlear lesions are caused by the secretions from the active otosclerotic foci, which then enter the endolymph 1. Vestibular disturbances also appear in patients suffering from otosclerosis 2, which may be derived from otosclerotic vascular changes due to the disease or from biochemical changes in the inner ear fluids. Because hearing loss is the dominant feature of otosclerosis, these patients may not be examined for other disorders associated with otosclerosis. Unsteadiness and dizziness have been frequently observed in these patients. Abnormal electronystagmographic (ENG) findings have been reported in otosclerotics 3. In the last few years, the study of otosclerosis has principally been devoted to the histochemistry of otosclerotic foci 4,5.
It is important to distinguish between clinical, non-clinical or histological otosclerosis; the latter is about 10 times more common than the former 6. A study has revealed histological otosclerosis on temporal bones in 12% of patients 7. In 1944, Guild demonstrated histological otosclerosis in only 8.3% of 482 African races, which was much less in the wider population (around 1%) 8.
Otosclerosis is usually bilateral; however, the frequency of histological unilateral otosclerosis ranges between 13% and 30% 8,9,10. The area of the labyrinthine capsule immediately in front of the footplate of the stapes, which is called ‘fissula ante-fenestrum‘, is the site of predilection for otosclerosis. Other frequent sites may include a border of the round window and even the footplate of the stapes around the cochlea, the internal auditory canal, or less often, around the semicircular canal 11.
Previous studies reported vestibular symptoms in patients with otosclerosis 12,13. Clinical studies reported the prevalence of vestibular symptoms in 3-35% of patients with otosclerosis 14. Another study reported increased caloric abnormalities in ears with cochlear pathology when compared to pure conductive hearing loss 15. The current study aimed to evaluate balance function in patients with CT scan confirmed otosclerosis.
Methods
Subjects
The total of 16 patients, aged 13-82 (mean age = 56.5) and suffering from clinical otosclerosis, participated in this study. Patients with otosclerosis were recruited from the Neuro-Otology and the ENT clinics at the Royal National Throat Nose & ear Hospital (RNTNEH). Patients’ details of the above two clinics were collected from the respective consultants and they were invited to take part in the study. Patients with radiologically confirmed otosclerosis were included. Patients with a history of perforated eardrum or ear discharge, ear operations, head injuries, meningitis, and ototoxic medication were excluded. As we already had a normative data for the balance tests from the Neuro-Otology clinic at RNTNEH, the ethics committee did not give permission for caloric testing of normal individuals. Consequently, this study could not have a control group of normal individuals. However, we were able to compare the data from the study with normative data available in the neuro-otology clinic. This study was approved by the Royal Free Hospital and Medical School Local Research Ethics Committee.
After necessary information, instruction and consent, patients had the following tests:
1-Pure tone Audiometry (PTA)
2-Impedance Audiometry (Tympanogram)
3-Bithermal Water Caloric Test
4-Rotational chair Test (ENG)
All patients had the impedance audiometry, pure tone, air, and bone conduction thresholds as per British Society of Audiology (BSA) recommended procedures. All eligible patients had bithermal caloric and rotational chair testing and the response was recorded by electronystagmography. All patients filled in a questionnaire, which included 8 different types of questions regarding to their balance (See appendix A). Each participant was requested to provide a written informed consent form before participation.
Physical examination
Within the clinic, a brief interview was carried out to conform to our inclusion and exclusion criteria. In this initial interview, each patient was asked to fill in the questionnaire and sign the consent form. The outer ear and the tympanic membrane (TM) were examined using a halogen otoscope to exclude any perforations or abnormal looking ear drums prior to the test.
Pure Tone Audiometry (PTA)
PTA was carried out using a GSI6/clinical audiometer with a TDH-50P headphone, following the British Society of Audiology recommended procedure 16,17,18. The audiometer was maintained and calibrated by the CAM services at the Royal National Throat, Nose & Ear Hospital (RNTNE) to ANSI 3.6, ISO 389. The audiometer was checked subjectively according to the recommended procedure before the start of each clinic. Testing was carried out in a soundproof room in the Neuro-Otology clinic. The test was performed by following the BSA recommended procedures. Patients were asked to press the switch button or raise their fingers as soon as they heard the tone, and keep pressing the button until they no longer heard the tone. Tested frequencies were started at 1000 Hz, followed by 2000 Hz, 4000 Hz, 8000 Hz, 500 Hz, and 250 Hz, and retest was done at 1000 Hz, for the first ear only. Then, the opposite ear was tested following the same order. In a 3-second duration, tone was presented at a level that was expected to be clearly audible to the patients, which was commonly about 30 dB above the estimated threshold. Patient responses were checked if it was correct and indicated the entire duration. If there was no response, we raised the volume levels by 20 dB-intervals until a response was obtained, and turned them down by 10 dB intervals until it dropped to 5dB or until the patient no longer responded. Tones were presented up to 4 times to decide whether at least 2 satisfactory responses were received. If this level was heard, it was the threshold for that tone, if not, we raised the levels by 5 dB and repeat the same steps until 2 out of 4 presentations were satisfactory.
Admittance Measures (Tympanometry)
Impedance audiometry was carried out using GSI 33 Impedance Bridge, calibrated by CAM services at the Royal National Throat, Nose & Ear Hospital to ANSI 3.6 (1969), ISO 389 (1975) standards. Screening tympanometry was carried out in all patients, according to the recommended procedures 19. Patients were given a brief description of the test procedure. They were instructed to sit in a comfortable position and to avoid any unnecessary movement, speaking or swallowing after the probe was fitted into the ear canal. A clean tip of a suitable size and shape was selected for each patient by pulling the pinna upward and backward while inserting the probe with rotatory movement to obtain an airtight seal, and by applying an excessive pressure of 200 daPa for a few seconds to ensure that the pressure was maintained. A routine measurement was done by selecting the probe frequency of 226 Hz, with a slow rate of changes in pressure (50 daPa or less).
Vestibular testing
Rotational Test (Impulsive Rotation)
Rotational test was carried out using an ENG chair, GOULD TA 240S (GOULD Instrument systems, Inc) ISO9001-1987. On the test day, otoscopy and tympanometry were carried out to check the condition of the external ear canal and the tympanic membrane for each patient. Patients were given a detailed description of the test and the possible side effects while being seated on a rotational chair. Surgical sprit and cotton were used to clean the patient’s forehead and outer canthi of the eyes with cautions. Three disposable silver–silver chloride electrodes were used. The ground electrode was placed on the center of the forehead, bitemporal electrodes were placed on outer canthi for conjugated horizontal eye movement recording. Electrode Jelly was applied through the hole in the center of the electrode using a syringe and a sterile blunt needle. The skin was gently abraded with the blunt needle to achieve impedance between 2 and 4 Ohms. The electrodes were then connected to the chair. ENG chair was connected to an integral light bar to adjust the patient head position relatively to the light bar and to perform eye calibration. Two calibration points were placed symmetrically on the horizontal plane in front of the patient for this purpose. After calibration, the impulse rotational test was carried out at 600/sec in darkness. The biggest amplitude response for the right- and the left-sided nystagmus in the first 5 wave forms of the tracing after the start and stop of the stimulus was selected by manually measuring individual beats. The average for right- and left-sided nystagmus was calculated separately. Nystagmus was measured manually by drawing a line through the slow phase of a beat of nystagmus, then the line was extended above and below the limits of this beat so that it reached the margins of the paper. After that, we counted 10 mm horizontally, as the paper speed was normally 10 mm/sec and the slow component velocity (SCV) was specified in degrees/sec as a unit of measurement. Then a right-angled triangle was created by connecting the 10 mm time mark to the diagonal line running through the nystagmus beat. The numbers of millimeters that constituted this vertical line up to the intersection were the number of a degree per second for that nystagmus beat. The gain was calculated for each side by the following method:
Gain = Maximum SCV/Stimulus (head/chair) Velocity
Comparing the responses from one side with the other symmetry was assessed by using the maximum SCV as follows:
Symmetry = VmR-VmL/VmR+VmL X 100; Where Vm is maximum SCV.
Caloric Test
Caloric test was carried out using the AQUAMETER water caloric stimulator by HORT MANN, GMBH, using Nicole 1992 by Nystar Computer program (Electronystagmography Testing & Analysis). Patients were given a detailed description of the test and the possible side-effects before starting the test. They were advised to stop any medications, vestibular sedation and alcohol for up to 48 hours before testing. Electrodes were placed on patients as described in the previous method section. The patient was asked to lie supine on a couch with the head elevated at 30 degrees and was instructed to keep his gaze fixed at a small red indicator light on the ceiling in front of him and to do arithmetic through the test. The right ear was first irrigated with warm water (44oC) from the caloric test machine for 40 seconds while ENG was recorded. This was followed by irrigation of the left ear with warm water after a short interval. Similarly, the ears were irrigated with cold (30oC) water in the same order. A five minutes interval was given between each irrigation. The eyes were examined for nystagmus from the start of each irrigation with patients’ gaze fixed on the target light on the ceiling, at first in light, and followed by darkness.
Statistical Analysis
Z-test was used to compare the current caloric and rotational test results with the data available from the literature and the normative data available in the Neuro-otology clinic. The subjects’ audiograms were examined, and the subjects were divided into three groups including sensorineural hearing loss, conductive hearing loss, and mixed hearing loss. In a sensorineural hearing loss, the audiogram of the patients was below 20 dB hearing loss at any frequency or combination of frequencies. This would include flat and low-frequency losses and there was no air-bone gap of greater than 10dB across the frequency range 0.5-4 KHz. In a conductive hearing loss, the air conduction threshold was below 20 dB hearing loss at any frequency in the frequency range 0.25-4 KHz. There would be an air-bone gap of greater than 10 dB hearing loss at least at one frequency in the range 0.5-4 KHz, at which was a hearing loss. In a mixed hearing loss, the audiogram was below 20 dB hearing loss in both air conduction and bone conduction at any frequency in the frequency range 0.25-4 KHz. There would be an air–bone gap of greater than 10 dB hearing loss.
Results
Descriptive statistics of current study
This study included 16 patients of 14 females and 2 males. Thirteen of the patients had radiologically confirmed otosclerosis (12 Females and 1 male). Three patients (2 females and 1 male) did not have CT confirmation of otosclerosis and therefore, were excluded from the study, although they had audiometric features of otosclerosis. The remaining 13 patient data were analyzed with regard to caloric, rotational chair testing, and questionnaire. Two patients were unable to do the caloric test and one other patient was unable to complete the test due to dizziness. Nine patients had a mixed hearing impairment at least on one side, 8 with bilateral mixed hearing loss and 1 with sensorineural hearing loss on the opposite side. Four patients had a bilateral sensorineural hearing loss.
Only 11 patients completed the questionnaire. Nine patients reported symptoms of dizziness. Additionally, they reported some forms of balance problems, including spinning in the head, a spinning of the surroundings, and light-headedness. Eight patients reported some precipitating factors that induced their dizziness. Five patients reported some associated aural symptoms such as hearing, tinnitus or both. Most of the patients reported the episodes of dizziness for a few months or for many years. The frequency of dizziness episode ranged from once a day to 1 – 2 times a year.
One patient had a canal paresis (CP) at 35% (normal ranges for CP is 0-20%). This patient also had a symptom of dizziness. None of the patients had any significant directional preponderance (DP) (normal range for DP is 0-28%). The above patient with significant CP (35%) did not show any rotational asymmetry on impulsive rotation.
Eleven patients had participated in a rotational chair test. Only one patient had a significant asymmetry to the right at 25.30% (normal range is <20%). However, this patient’s caloric test did not show any significant CP or DP. Two patients (18 %) of the radiologically confirmed otosclerosis had an abnormal balance test, including both caloric and rotational tests.
Comparison of current data with the available data in the literature
Caloric test data
One patient (12%) in the current study had a significant CP. One out of 8 had an abnormal caloric test =12% (p). Our result was compared with the literature 20, which reported that 60% of patients (total 191) had abnormal responses to bithermal caloric stimulation.
Cody & Baker 60% (Π)
Z= p- Π /√ p* (100- p)/n
=number of patients in the study=8
=12-60/√ 12*(100-12) /8
= -48/ √12*(88)/8
= -48/ √132
= -48/11.48
= 4.1, p<0.001
Based on the normal distribution function table Probability = p<0.001 (2 tailed test), this result was translated into a significant level.
Vestibular symptoms (questionnaire)
Nine out of 11 patients in the current study had vestibular symptoms (81.81% (p)). We compared our result with the literature 20. A study done by Cody and Baker 20 tested 191 patients with both vestibular and auditory symptoms of otosclerosis. They found that about 42.5% of the patients had vestibular symptoms in their group.
Cody& Baker 42.5% (Π)
Z= p- Π /√ p * (100- p)/n
=number of patients in the study=11
=81.81-42.5/√ 81.81*(100-81.81) /11
= 39.31/ √81.81*(18.19)/11
= 39.31/√1488.123/11
=39.31/√135.228
=39.31/11.63
=3.4 p<0.001
Based on the normal distribution function table Probability = p<0.001 (2 tailed test), this result was translated into a significant level.
Therefore, in the current study, data about both caloric testing and vestibular symptoms were statically significant compared to the available data in the literature.
Discussion
Otosclerosis is the most frequent cause for those cases of progressive deafness, which may result in severe handicap. Vestibular disturbances in otosclerosis may arise from otosclerotic vascular changes of the abnormal spongy bone formation or from biochemical changes in the inner ear fluids. George Shambaugh, Jr., 21 has observed that the inner ear damage in otosclerosis commonly occurs at the beginning of the disease, he was the first to describe a case of otosclerosis presenting at first with pure perspective deafness and only showing signs of stapedial ankylosis years later.
Cody and Baker 20 conducted a study in which they tested 191 patients with both vestibular and auditory symptoms of otosclerosis for three and a half years (between mid –1973 and December 1976). They found that about 60% of their patients had abnormal responses to bithermal caloric stimulation. A similar prevalence was reported by Virolanen 22, who also found directional preponderance or positional nystagmus in one third to one half of the patients he studied. He found nystagmus in 41.17% of the patients on ENG. In the same study done by Cody and Baker 20, they found that the incidence of vestibular symptoms increased as the relative and the absolute amount of sensorineural hearing loss increased. Not only did the incidence of the vestibular symptoms increase in the amount of sensorineural hearing loss, but also did the degree of severity of the vestibular symptoms.
In the current study, 12% (n = 1) of patients had an abnormal caloric test and 18.18% (n = 2) had abnormal ENG findings, including both caloric and rotational tests. We did not attempt to compare our impulse rotation parameter, i.e. symmetry with the literature, as we were unable to find similar data. Our questionnaire analysis confirmed that 81.81% (n = 11) of our patients had some forms of dizziness. This is in contrast with Cody and Baker 20 study, which reported a figure of 42.5% vestibular symptoms and 60% abnormal response to caloric stimulation. This may be because our patients were a small group that possibly did not include those with significant vestibular test abnormalities.
The current study had many potential limitations. The number of patients tested in this study was small. The restrictions imposed by the ethics committee in carrying out the caloric test in normal individuals precluded control subjects for this study. The manual evaluation of maximum SCV used to assess gain and symmetry in impulse rotation test was known to be inaccurate and it also introduced an element of observer bias.
Conclusions
The current study suggests a high prevalence of balance symptoms (81.81%, n = 9) in patients with radiological otosclerosis, although only a small proportion (18.18%, n = 2) showed abnormal vestibular function on caloric and impulse rotation testing. However, due to a small number of samples in the current study, further studies on the larger sample are warranted to validate these findings.
Abbreviations
BSA: British Society of Audiology
CP: canal paresis
DP: directional preponderance
ENG: Electronystagmography
p: prevalence
PTA: Pure tone Audiometry
SCV: Slow component velocity
TM: Tympanic membrane
Competing Interests
None of the authors reported any conflict interest related to this study.
Authors' Contributions
Rania Abdulfattah Sharaf: the corresponding author, participated in the study design, participated in the data collection, drafted the manuscript, and finalized the manuscript. Rudrapathy Palaniappan: participated in the study design, helped with the ethics application and revised the manuscript critically.
References
-
Cureoglu
S.,
Baylan
M.Y.,
Paparella
M.M.,
Cochlear otosclerosis. Current Opinion in Otolaryngology {&}amp; Head {&}amp; Neck Surgery.
2010;
18
(5)
:
357-62
.
View Article PubMed Google Scholar -
de Vilhena
D.,
Gambôa
I.,
Duarte
D.,
Lopes
G.,
Vestibular Disorders after Stapedial Surgery in Patients with Otosclerosis. International Journal of Otolaryngology.
2016;
2016
:
6830648
.
View Article PubMed Google Scholar -
Parnes
S.,
Black
F.O.,
Wall
C.,
O'Leary
D.P.,
Feltyberger
E.,
Vestibular system abnormalities in otosclerotic subjects. Otolaryngology.
1978;
86
(1)
:
98-106
.
View Article PubMed Google Scholar -
Redfors
Y.D.,
Gröndahl
H.G.,
Hellgren
J.,
Lindfors
N.,
Nilsson
I.,
Möller
C.,
Otosclerosis: anatomy and pathology in the temporal bone assessed by multi-slice and cone-beam CT. Otology {&}amp; Neurotology.
2012;
33
(6)
:
922-7
.
View Article PubMed Google Scholar -
Faccioli
N.,
Barillari
M.,
Guariglia
S.,
Zivelonghi
E.,
Rizzotti
A.,
Cerini
R.,
others
Radiation dose saving through the use of cone-beam CT in hearing-impaired patients. La Radiologia Medica.
2009;
114
(8)
:
1308-18
.
View Article PubMed Google Scholar -
Kanzara
T.,
Virk
J.S.,
Diagnostic performance of high resolution computed tomography in otosclerosis. World Journal of Clinical Cases.
2017;
5
(7)
:
286-91
.
View Article PubMed Google Scholar -
Quesnel
A.M.,
Ishai
R.,
McKenna
M.J.,
Otosclerosis: Temporal Bone Pathology. Otolaryngologic Clinics of North America.
2018;
51
(2)
:
291-303
.
View Article PubMed Google Scholar -
Guild
S.R.,
Normal and Pathological Anatomy of the Petrous Pyramid 1935.
Google Scholar -
Nylen
B.,
Histopathological investigations on the localization, number, activity and extent of otosclerotic foci. The Journal of Laryngology and Otology.
1949;
63
(6)
:
321-7
.
View Article PubMed Google Scholar -
Cawthorne
T.,
Otosclerosis. J Laryngol Otol.
1955;
69
(7)
:
437-56
.
-
Virolainen
Erkki,
Vestibular disturbances in clinical otosclerosis. Acta Oto-Laryngologica.
1972;
74
(sup306)
:
5-34
.
-
Panda
N.K.,
Saha
A.K.,
Gupta
A.K.,
Mann
S.B.,
Evaluation of vestibular functions in otosclerosis before and after small fenestra stapedotomy. Indian Journal of Otolaryngology and Head and Neck Surgery.
2001;
53
(1)
:
23-7
.
View Article PubMed Google Scholar -
Yetişer
S.,
Bilateral Vestibulopathy Due to Severe Cochlear Otosclerosis: A Well-Known Condition Without Any Favorable Solution. Turk Arch Otorhinolaryngol.
2018;
56
(3)
:
174-6
.
View Article PubMed Google Scholar -
Meurman
O.H.,
Aantaa
E.,
Virolainen
E.,
Vestibular disturbances in clinical otosclerosis. Archives of Otolaryngology (Chicago, Ill.).
1969;
90
(6)
:
756-8
.
View Article Google Scholar -
Morales-Garcia
C.,
Cochleo-vestibular involvement in otosclerosis. Acta Oto-Laryngologica.
1972;
73
(6)
:
484-92
.
View Article PubMed Google Scholar -
Moore
D.R.,
Rosen
S.,
Bamiou
D.E.,
Campbell
N.G.,
Sirimanna
T.,
Evolving concepts of developmental auditory processing disorder (APD): a British Society of Audiology APD special interest group `white paper'. International Journal of Audiology.
2013;
52
(1)
:
3-13
.
View Article PubMed Google Scholar -
Audiology
British Society of,
Pure tone air and bone conduction threshold audiometry with and without masking and determination of uncomfortable loudness levelsBritish Society of Audiology: Reading, UK; 2004.
Google Scholar -
Audiology
British Society of,
Recommended procedure for pure-tone bone-conduction audiometry without masking using a manually operated instrumentBritish Society of Audiology 1985.
Google Scholar -
British-Society-of-Audiology
Recommended procedure for tympanometryBritish Society of Audiology: Bathgate EH47 7AQ; 1992.
Google Scholar -
Cody
D.T.,
Baker
H.L.,
Otosclerosis: vestibular symptoms and sensorineural hearing loss. The Annals of Otology, Rhinology, and Laryngology.
1978;
87
(6 Pt 1)
:
778-96
.
View Article PubMed Google Scholar -
Shambaugh
G.E.,
Endocrine aspects of Meniere's disease. The Laryngoscope.
1959;
69
(8)
:
1027-32
.
View Article PubMed Google Scholar -
Terence
C.,
Otosclerosis: The Dalby Memorial Lecture. The Journal of Laryngology and Otology.
1955;
69
:
437-56
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 6 No 3 (2019)
Page No.: 3034-3039
Published on: 2019-03-29
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 7764 times
- Download PDF downloaded - 2198 times
- View Article downloaded - 0 times
- Appendix downloaded - 1632 times
 Biomedpress
Biomedpress

