Abstract
Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethidine on postoperative shivering.
Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shivering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square and Pearson correlation.
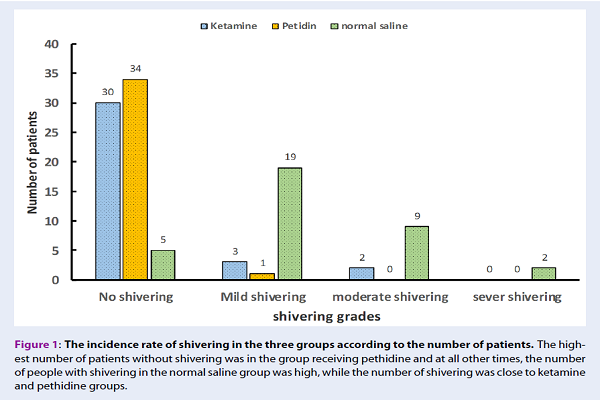
Results: The mean age of patients was 35.8+/-11.45 years in the ketamine group, 34.8+/-11.64 years in the normal saline group, and 33.11+/-10.5 years in the pethidine group. The one-way ANOVA showed no significant difference in the mean age between the three groups (P=0.645). The incidence and intensity of shivering were significantly higher in the normal saline group than in the ketamine and pethidine groups (p=0.001). However, there was no significant difference in the incidence and the intensity of shivering between the ketamine and the pethidine groups (p=0.936).
Conclusion: The results showed that the 0.5 mg/kg of ketamine could control the post-anesthetic shivering.
Introduction
Surgery and anesthesia disturb the balance between the production and loss of body temperature. The use of anesthetics and opioids leads to motor and behavioral inhibition, body movements and consequently a decrease in body temperature, which results in shivering 12. The core body temperature decreases from 0.5ºC to 1.5ºC after anesthesia induction. All anesthetic drugs specifically change the temperature-regulating system 3. Postoperative shivering, in addition to discomfort and dissatisfaction of the patient, accounts for numerous complications such as cardiorespiratory abnormalities, increased oxygen consumption, subsequent cell hypoxia, and increased production of lactic acid and carbon dioxide. The shivering can also increase return time, pain perception, and intraocular and intracranial pressure 45. Previous studies recommended various medications such as Meperidine, Ketamine plus Midazolam, Neostigmine and Ketanserin to control and treat post anesthetic shivering 67.
Pethidine is one of the most effective drugs to control postoperative shivering 8. In more recent studies, ketamine has also been reported as an effective drug to control postanesthetic shivering 9. Another study introduced the use of pethidine with dexamethasone as the more effective method than ketamine and midazolam 10. Ketamine controls postanesthetic shivering by multiple mechanism. Ketamine is a drug binding to N-methyl-d-aspartate (NMDA) receptor, which is critical at different levels in thermoregulation. NMDA receptors regulate noradrenergic and serotonergic systems in locus coeruleus 11. Previous studies have shown that ketamine is effective in controlling postanesthetic shivering 121314. Therefore, this study was conducted to compare the effects of prophylactic injection of ketamine, and pethidine on post-anesthetic shivering.
Methods
Study Design, Ethical Considerations, Patients
The current double-blind clinical trial was approved by the Deputy of Research and Technology at Zahedan University of Medical Sciences, Iran, and permitted by the Ethics Committee of the University. All enrolled patients in the study signed consents after being fully informed.
Sample Size and Randomization
The sample size was calculated to be 105 people according to previous studies and formula to calculate sample size. These patients were divided randomly into three groups of 35 after enrolling in the study based on inclusion criteria 15.
Inclusion and Exclusion Criteria
The inclusion criteria were Class I and II American Society of Anaesthesiology (ASA) including no history of cardiovascular, respiratory, psychiatric, neuromuscular (myoclonus, Parkinson, Huntington, multiple sclerosis, seizure), endocrine disorders (diabetes and thyroid disorders), and body temperature ranging from 36.5ºC to 38ºC. In addition, patients with intraoperative blood transfusion were also excluded from the study.
Interventions
The operating room temperature was adjusted to 24°C by air conditioner according to the tropical nature of the area. Then, the ear temperature was measured and recorded.
Next, an angiocath number 18 was fixed in the left antecubital fossa for all patients, followed by normal saline infusion (10cc/kg). The monitoring device (SAADAT, Iran) was used to non-invasively monitor of heart rhythm, arterial oxygen saturation, and blood pressure. The oxygen was prescribed with a face mask for patients (7 liters per minute). The anesthesia was induced with propofol (2 mg/kg/IV), midazolam (2 mg/IV), fentanyl (1 μg/kg/IV) and atracurium (0.5 mg/kg/IV). The intubation was done with a video laryngoscope. During the operation, the anesthesia continued with 60% N2O, oxygen and propofol (100-200 μg/kg/min) and remifentanil (0.05-0.1 μg/kg/min). A repeated dose of the atracurium, if needed (0.1 mg/kg/IV), was performed every 20 minutes. All medications were injected and stored at room temperature.
Twenty minutes prior to the end of surgery, the first group was injected with 0.4 mg/kg of pethidine (Iran Pharmaceutical darou pakhsh Company), the second group with 0.5 mg/kg of ketamine (Manufacture of Germany ROTEXMEDICA company), and the third group with placebo (normal saline); the volume of three syringes reached 3 cc. For blinding, the used drugs were prepared by the researcher and presented to an anesthetic expert who was unaware of the study and grouping of patients. After completing the surgery, the residual neuromuscular block was returned with neostigmine (0.04 mg/kg/IV) and atropine (0.02 mg/kg/IV).
After obtaining the necessary criteria, the tracheal tube was removed from the patients. The type and duration of operation were recorded in information forms. The patients were transferred to a recovery ward and oxygen therapy was started with a face mask (7 liters per minute), and the patient's body was covered with a double layer linen bed sheet.
An anesthesiologist, who was unaware of processing and grouping of the studied patients, assessed the patients for the shivering. The tympanic membrane temperature was recorded at 0, 10, 20 and 30 minutes after entering the recovery room. The shivering was evaluated with a four-point grading system.
| Grade | Clinical signs |
| 0 | No shivering |
| 1 | Mild fasciculation of face or neck |
| 2 | Visible tremor involving more than one muscle group |
| 3 | Gross muscular activity involving the entire body |
In case of obtaining the score of two and over, the shivering was treated with 25 mg/IV of pethidine.
Statistical Analysis
Data were then compared with SPSS version 22 software using descriptive statistics and one-way ANOVA, Kruskal Wallis, chi-square and Pearson correlation.
Results
In total, the patients were composed of 62% of women and 38% of men. There was no significant difference regarding gender distribution among patients in the three groups (P=0.176) (Table 2).
| Groups | Sex | Total | P-value | |
| Male | Female | |||
| Ketamine | 1543% | 2057% | 35 | 0.176 |
| Pethidine | 1646% | 1954% | 35 | |
| Normal saline | 926% | 2974% | 35 | |
| Total | 4038% | 6562% | 105 |
The mean age of patients was 35.8±11.45 years in the ketamine group, 33.11±10.5 years in the pethidine group, and 34.8±11.64 years in the normal saline group. The one-way ANOVA showed no significant difference in the mean age between the three groups (P=0.645).
The mean duration of surgery was 109.24±37.87 minutes in the ketamine group, 105.30±36.97 minutes in the normal saline group and 106.41±35.94 in the pethidine group, which was not significantly different (P=0.975) Table 3.
| Groups | Shivering | p-value | |
| Without shivering | With shivering | ||
| Ketamine,Pethidine | 30(86%)34(97%) | 5(14%)1(3%) | 0.06 |
| Ketamine,Normal saline | 30(86%)5(14%) | 5(14%)30(86%) | 0.001 |
| Pethidine,Normal saline | 34(97%)5(14%) | 1(3%)30(86%) | 0.001 |
| Total | 69(66%) | 36(34%) |
The frequency of shivering in the groups receiving ketamine and pethidine was significantly lower than in the normal saline group (p=0.001).
The shivering grade was significantly lower in the ketamine and pethidine groups than in the normal saline group (p=0.001). In the normal saline group, 86% of patients had postoperative shivering, of which only 6% were severe that reported in the same group. In the ketamine group, only 14% of the patients experienced shivering, of which 6% had moderate grade and the rest was mild, and none of the patients had severe shivering.
In the pethidine group, only 3% of the patients had mild shivering, but there was no significant difference in the incidence rate of shivering between the pethidine and ketamine groups (p=0.0936) (Table 4 and Figure 1).
| Groups | Shivering grades | p-value | |||
| Negative | Mild | Moderate | Severe | ||
| Ketamine,Pethidine | 30(86%)34(97%) | 3(8%)1(3%) | 2(6%) 0(0%) | 0(0%)0( 0%) | 0.0936 |
| Ketamine,Normal saline | 30(86%)5(14%) | 3(8%)19(34%) | 2(6%)9(26%) | 0(0%)2(6%) | 0.001 |
| Pethidine,Normal saline | 34(97%)5(14%) | 1(3%)19(34%) | 0(0%) 9(26%) | 0(0%) 2(6%) | 0.001 |
| Total | 6965% | 2322% | 1111% | 22% |
| Groups | Need for pethidine injection in recovery room | P-value | |
| No | Yes | ||
| Ketamine,Pethidine | 33(94%)35(100%) | 2(6%)0(0%) | 0.7 |
| Ketamine, Normal saline | 33(94%)16(46%) | 2(6%) 19(54%) | 0.001 |
| Pethidine, Normal saline | 35(100%)16(46%) | 0(0%)19(54%) | 0.000 |
| Total | 8480% | 2120% |
The patients with the Grade 2 shivering (moderate) were treated by the pethidine injection in the recovery room. In the ketamine group, only two patients (6%) required the pethidine, while 19 patients (54%) in the normal saline group needed the pethidine injection, so the need for the pethidine injection was significantly lower in the ketamine group than in the normal saline group (P<0.001). However, no significant difference was observed between the pethidine and ketamine groups (P=0.7). In addition, there was a significant and reverse correlation between the postoperative shivering and the tympanic membrane temperature at the time before induction of anesthesia, at the beginning of the recovery room and 0, 10, 20 and 30 minutes after entering the recovery room (r=-0.6, P=0.001).
Discussion
The results of this study showed that the use of a low dose prophylactic ketamine could be effective in controlling the postoperative shivering of patients, while pethidine requires a higher dose to achieve the same effect. However, in studies with a dose of 0.75 mg/kg, the control of shivering by the ketamine has been reported to be more effective than the pethidine, but accompanied by side effects such as nystagmus and vertigo 1617. In any case, the prophylactic use of an appropriate drug seems necessary to control the postoperative shivering. In line with the results of this study, Manouchehrian et al. reported that the ketamine is effective in controlling postoperative shivering. However, the difference between this study and our study is that ketamine was compared to hydrocortisone and placebo (normal saline) instead of pethidine. They concluded that ketamine was more effective to control postoperative shivering. According to the results of both studies, the emphasis was placed on the ability of prophylactic ketamine to control the postoperative shivering 18. Akram et al. compared ketamine and tramadol to control postoperative shivering and reported that ketamine could control postoperative shivering better than tramadol 9. Contrary to the results of the study, Loyal et al. compared the effect of intravenous clonidine and tramadol to control post-spinal anesthesia shivering and reported that tramadol is more effective in controlling postoperative shivering 2. No complete and specific treatment has been identified for postoperative shivering 19. With sympathetic stimulation, ketamine can increase blood pressure, heart rate, and cardiac output, and these can be beneficial in patients with hypothermia 2021. Low-dose of ketamine during spinal anesthesia prevents lower body temperature 22. Kishnani et al. compared the combination of ketamine plus midazolam versus tramadol and placebo to control the post-spinal anesthesia shivering and reported that tramadol controls postoperative shivering better than the combination of ketamine plus midazolam. It should be noted that the mentioned study used a dose of 25 mg/kg of ketamine and 40 μg/kg of midazolam and only five patients experienced mild shivering, while our results reported three patients with mild shivering in the ketamine group and six patients with moderate shivering, which are much higher than the mentioned study. The reason for this is probably related to midazolam and synergistic effects between these two drugs. In the noted study, the difference in the tramadol group with the ketamine group was only in one patient, but this difference was statistically significant 7. Based on the results of this study, Mahoori et al. compared the prophylactic use with a dose of 0.5 mg/kg of ketamine and placebo and concluded that the incidence rate of shivering in the two groups did not differ significantly, but the intensity of shivering was much lower in the ketamine group 21. Solhpour et al. compared the prophylactic use of meperidine, meperidine plus dexamethasone, and ketamine plus midazolam for preventing shivering during spinal anesthesia. Different from other studies, they stated that the use of meperidine plus dexamethasone controls the post-spinal anesthesia shivering better than the ketamine plus midazolam and the meperidine alone though differences in Grades 2 and three shivering occurred between three groups was related to only two patients 10. Mohamed et al. reported that the administration of 0.5mg/kg of pethidine controls postoperative shivering better than 0.5mg/kg of tramadol, but induces more sedation 23.
One of the limitations of the present study is the failure to accurately adjust the temperature of all parts of the recovery environment due to its large space which may have affected the results. Other limitations include small sample size in each group, and only one center was involved in the study. Thus, larger sample size and multiple studying sites would be recommended to validate the findings in this study.
Conclusions
Despite the better ability of pethidine to control postanesthetic shivering, there is a potential risk of respiratory depression by pethidine in general anesthetized patients who have received opioid for induction. Given the small difference in the incidence rate and the intensity of shivering between pethidine and ketamine in this study, the use of pethidine is recommended to control post-spinal anesthesia shivering and the prophylactic ketamine should be used to control the post general anesthesia shivering.
Competing Interests
The authors have expressed no financial conflict of interest.
Authors' Contributions
Masoum Khoshfetrat: participation in implementation of research and supervision over data collection and revising this paper. Ali Rosom Jalali: participation in implementation of research and data collection. Gholamreza Komeili: Statistics consultant and statistical analysis. Aliakbar Keykha: Compilation of the paper and Editing this paper carefully. All authors reviewed, commented and approved the final version.
Funding
The present study was financially supported by Zahedan University of Medical Sciences, Zahedan, Iran.
Acknowledgments
This article has been adopted from the Thesis written by Resident of Anesthesiology and Critical Care, approved and funded by Research and Technology Deputy of Zahedan University of Medical Sciences. The researcher would like to express own gratitude to the Research and Technology Deputy of the University and the staff and ICU ward at the Khatam-ol-Anbia Hospital of Zahedan
References
-
Crowley
L. J.,
Buggy
D. J..
Shivering and neuraxial anesthesia. Regional Anesthesia and Pain Medicine.
2008;
33
:
241-52
.
View Article Google Scholar -
Loyal
M.,
Chauhan
S.,
Khandelwal
M..
Randomized double blind comparative study of intravenous clonidine and tramadol in post spinal anaesthesia shivering. International Journal of Scientific Research (Ahmedabad, India).
2018;
6
:
53-5
.
-
Mathews
S.,
Mulla
A. Al,
Varghese
P.,
Radim
K.,
Mumtaz
S..
Postanaesthetic shivering-a new look at tramadol. Anaesthesia.
2002;
57
:
387-4
.
View Article PubMed Google Scholar -
Yu
S. C.,
Kee
W. D. Ngan,
Kwan
A. S..
Addition of meperidine to bupivacaine for spinal anaesthesia for Caesarean section. British Journal of Anaesthesia.
2002;
88
:
379-83
.
View Article PubMed Google Scholar -
Hasannasab
B.,
Banihashem
N.,
Khoshbakht
A..
Prophylactic Effects of Doxapram, Ketamine and Meperidine in Postoperative Shivering. Anesthesia and Pain Medicine.
2016;
6
:
e27515
.
View Article PubMed Google Scholar -
Zhang
Y.,
Wong
K. C..
Anesthesia and postoperative shivering: its etiology, treatment and prevention. Acta Anaesthesiologica Sinica.
1999;
37
:
115-20
.
PubMed Google Scholar -
Kishnani
K. L.,
Dave
S. P.,
Jain
P..
Pervention of Post Spinal Shevering:Using Combination Of Ketamine Plus Midazolam Vs Tramadol ang Plasebo. 2018;
7
:
48-50
.
-
Terasako
K.,
Yamamoto
M..
Comparison between pentazocine, pethidine and placebo in the treatment of post-anesthetic shivering. Acta Anaesthesiologica Scandinavica.
2000;
44
:
311-2
.
View Article PubMed Google Scholar -
Akram
M.,
Raza
H.,
Imam
S. M..
Efficacy of Prophylactic Low Dose Ketamine and Tramadol for Prevention of Shivering During Spinal Anaesthesia in Patients Undergoing Lower Abdominal Surgeries. Pakistan Journal of Medical & Health Sciences.
2015;
11
:
378-80
.
-
Solhpour
A.,
Jafari
A.,
Hashemi
M.,
Hosseini
B.,
Razavi
S.,
Mohseni
G..
A comparison of prophylactic use of meperidine, meperidine plus dexamethasone, and ketamine plus midazolam for preventing of shivering during spinal anesthesia: a randomized, double-blind, placebo-controlled study. Journal of Clinical Anesthesia.
2016;
34
:
128-35
.
View Article PubMed Google Scholar -
Dal
D.,
Kose
A.,
Honca
M.,
Akinci
S. B.,
Basgul
E.,
Aypar
U..
Efficacy of prophylactic ketamine in preventing postoperative shivering. British Journal of Anaesthesia.
2005;
95
:
189-92
.
View Article Google Scholar -
Kose
E. A.,
Honca
M.,
Dal
D.,
Akinci
S. B.,
Aypar
U..
Prophylactic ketamine to prevent shivering in parturients undergoing Cesarean delivery during spinal anesthesia. Journal of Clinical Anesthesia.
2013;
25
:
275-80
.
View Article PubMed Google Scholar -
Norouzi
M.,
Doroodian
M. R.,
Salajegheh
S..
Optimum dose of ketamine for prevention of postanesthetic shivering; a randomized double-blind placebo-controlled clinical trial. Acta Anaesthesiologica Belgica.
2011;
62
:
33-6
.
PubMed Google Scholar -
Gecaj-Gashi
A.,
Hashimi
M.,
Sada
F.,
Salihu
S.,
Terziqi
H..
Prophylactic ketamine reduces incidence of postanaesthetic shivering. Nigerian Journal of Medicine.
2010;
19
:
267-70
.
View Article PubMed Google Scholar -
Khezri
M. B.,
Mosallaei
M. A.,
Ebtehaj
M.,
Mohammadi
N..
Comparison of preemptive effect of intravenous ketorolac versus meperidine on postoperative shivering and pain in patients undergoing cesarean section under spinal anesthesia: A prospective, randomized, double-blind study. Caspian Journal of Internal Medicine.
2018;
9
:
151-7
.
View Article PubMed Google Scholar -
Kose
E. A.,
Dal
D.,
Akinci
S. B.,
Saricaoglu
F.,
Aypar
U..
The efficacy of ketamine for the treatment of postoperative shivering. Anesthesia and Analgesia.
2008;
106
:
120-2
.
View Article PubMed Google Scholar -
Nasreen
L.,
Muhammad
N.,
Namika
N.,
Shahid
K..
Prevention of postoperative shivering by prophylactic ketamine in patients undergoing major surgeries under General Anesthesia. 2006;
2
:
163-6
.
-
Manouchehrian
N.,
Sanatkar
M.,
Asadi
H. K.,
Soleimani
E.,
Moradi
A..
A Comparative Study on the Effect of Intravenous Hydrocortisone and Ketamine on Reducing Shivering after Spinal Anesthesia in Cesarean Section: A Double-blind Randomized Controlled Trial. 2018;
4
:
459-63
.
-
Kranke
P.,
Eberhart
L. H.,
Roewer
N.,
Tramer
M. R..
Pharmacological treatment of postoperative shivering: a quantitative systematic review of randomized controlled trials. Anesthesia and Analgesia.
2002;
94
:
453-60
.
View Article PubMed Google Scholar -
Ikeda
T.,
Kazama
T.,
Sessler
D. I.,
Toriyama
S.,
Niwa
K.,
Shimada
C..
Induction of anesthesia with ketamine reduces the magnitude of redistribution hypothermia. Anesthesia and Analgesia.
2001;
93
:
934-8
.
View Article PubMed Google Scholar -
Mahoori
A.,
Hasanloei
M. Valizade,
Hassani
E.,
Sadighi
F..
The effect of intravenous low dose ketamine for prevention of shivering after ingouinal herniorrhaphy. The Journal Of Urmia University Of Medical Scinces.
2013;
24
:
779-84
.
-
Kinoshita
T.,
Suzuki
M.,
Shimada
Y.,
Ogawa
R..
Effect of low-dose ketamine on redistribution hypothermia during spinal anesthesia sedated by propofol. Journal of Nippon Medical School.
2004;
71
:
92-8
.
View Article PubMed Google Scholar -
Mohamed
T.,
Hema
V. R..
A comparison of tramadol and pethidine for control of shivering during caesarean section under spinal anaesthesia. Group.
2017;
11
:
2231-4
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 12 (2018)
Page No.: 2898-2903
Published on: 2018-12-25
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 10604 times
- Download PDF downloaded - 2343 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress



