Abstract
Background: Generally, there are two methods for childbirth: normal vaginal and cesarean section (C-section). Each method has advantages and complications. In this study, we investigated the effects of type of delivery on hematological parameters in healthy full-term neonates in an Iranian population, from 2016-2017.
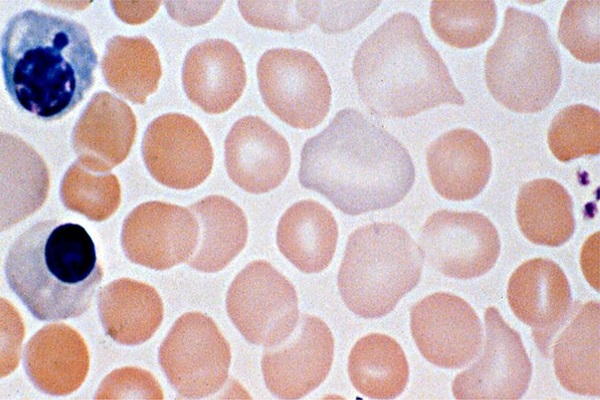
Materials: Three hundred pregnant women, along with their healthy and term babies, were studied. According to the route of delivery, the neonates were divided into two groups: vaginal (n=150) and C-section (n=150). Complete blood count (CBC) and peripheral blood smear (PBS) were performed on the neonates from umbilical cord blood immediately after birth. Data were analyzed by using SPSS v. 22 and statistical analyses were done by student's t-test and correlation tests, with P-value < 0.05 set as the lowest limit of significance.
Results: We observed a significant increase in hematologic parameters, such as red blood cell (RBC) count, hemoglobin, hematocrit, red cell distribution width (RDW), platelets, total leukocyte count and neutrophil count, in full-term neonates who delivered vaginally compared to those delivered by cesarean section (p<0.001). However, there was no significant difference between the delivery types in terms of mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), mean platelet volume (MPV), platelet distribution width (PDW), eosinophil count, lymphocyte count, or monocyte count.
Conclusion: According to our study, the mode of delivery influences the hematological parameters in full-term neonates; thrombocytopenia and anemia in neonates were associated with cesarean section delivery. Thus, we recommend that pregnant women do not deliver by C-section unless in emergency situations.
Introduction
Childbirth is one of the divine gifts for procreation and increasing the human population on earth, from the time of Adam and Eve to now. The mechanism of childbirth is a self-sustaining process with no need for external intervention. If the childbirth is dangerous for the fetus or mother, a cesarean section (C-section) can help to save the mother’s or baby's life 12.
Unfortunately, nowadays, the prevalence of C-section in most of the developed countries has reached more than 50%, and indeed, in many societies childbirth by this method has turned into a cultural trend such that more than half of women voluntarily prefer to have a C-section 345. Thus, in addition to increasing the mother’s risk of death after performing this surgery, as well as creating physical and psychological complications, C-section can increase costs for the mother and her family by 2-3 fold. Moreover, mothers who experience disabilities after C-section are prone to inattention, less care, and incorrect breastfeeding after the birth of the newborn 67.
C-sections are typically limited to special, emergency cases in which childbirth through the natural channel isn’t possible or when serious dangers are posed for mother and fetus. Thus, the use of C-section surgery is restrictive. It is not the preferred method for childbirth since like other surgeries, it is accompanied with risks and complications for mother and fetus 89, in comparison to vaginal childbirth. Indeed, the rate of mortality from C-section is 7-fold greater than that for natural childbirth 10. Owing to the complications C-section poses to mother and fetus, in recent years, international organizations such as the World Health Organization have emphasized that this type of childbirth delivery should only be performed based on the clinical dangers for the mother 1112.
When vaginal birth occurs naturally, without use of instruments and medications, the newborn immediately has skin contact with the mother, and this can increase the possibility of breastfeeding 13. The pain of natural childbirth causes the production of oxytocin, epinephrine, and adrenaline which have important roles in facilitating responses between mother and newborn, as well as in early breastfeeding post-delivery 141516. On the other hand, the breastfeeding period is the most sensitive period for growth and evolution in the human life and, thus, correct infant feeding plays an important role in this period. Breast milk is the most complete food for infants in the first few months after birth 1718.
Breast milk includes different protective immunological substances, such as immunoglobulins and growth factors. Human milk contains antibodies produced against the mother’s peripheral antigens, such as E. coli. As a result, infants fed by breast milk are less susceptible to intestinal infections 19202122, and are more protected against rotavirus which can cause infantile gastroenteritis 23. Furthermore, breastfeeding can decrease the risk of atopic dermatitis and respiratory infections 24. A mother’s milk contains both T and B lymphocytes. T lymphocytes in breast milk are different from those found in the blood; T cells in breast milk particularly present specific antigens. It is suggested an infant benefits from the mother’s immunological experiences via the memory T lymphocytes in the milk 252627. For the first newborn, the hematological indexes (such as leukocytes, hematocrit, platelets, and hemoglobin) were higher than those for the second and third newborn.
In women with high parity due to frequent childbirth and menstrual cycles, iron deficiency is greater than in nulliparous women 282930. Iron deficiency increases the risk of preterm childbirth and low weight in newborns. In fact, in low weight and premature infants, hematocrit levels are decreased 31. On the other hand, in women with high parity, natural childbirth or C-section is accompanied by less stress, in comparison to nulliparous women, because of previous childbirth experience and short deliveries. Moreover, the leukocyte and neutrophil counts in nulliparous women are higher because of the high rate of cortisol 3233.
Sexual hormones (like testosterone) are one of the reasons of why hematocrit levels are increased in males during puberty. Various studies have reported that levels of testosterone among male infants are higher than among female ones 34. According to the studies, the level of umbilical vein testosterone in male newborns is significantly higher than that in female newborns. It seems that one of the reasons for high hematocrit in male infants is the higher level of testosterone in males versus female infants 3536. During puberty, sexual steroids such as estrogen and progesterone will increase; these hormones impress hematopoiesis and play a role in the reduction of hemoglobin in the pregnancy period. The levels of the steroid hormones (estrogen and progesterone) are high, while the mother’s hemoglobin concentration is reduced during the pregnancy period 37.
It has been hypothesized that female infants may have the sexual hormones as those in the puberty period, as well as lower levels of hemoglobin than male infants 38. The infant levels of hemoglobin and hematocrit depend on various factors. The delayed close of the umbilical cord can increase infant hemoglobin levels up to 20%. Also, if the placenta is cut off and interrupted, and/or one of the fetus vessels is pierced or torn and the infant is kept significantly above the level of the placenta before closing the cord, the hemoglobin concentration may be decreased after childbirth 39. Factors such as early birth, anemia during pregnancy, and C-section can also decrease levels of hemoglobin at the beginning of birth and can be followed by accelerated or intensified anemia 404142.
Accordingly, the type of childbirth can have different effects on various infant hematological factors. Thus, it is also important to determine and understand the neonatal blood indices as it relates to childbirth effects. In this study, an Iranian population was evaluated with the purpose of surveying and comparing the effects of natural childbirth versus C-section on infant hematological factors.
Methods
Study population
Patients included in this study consisted of healthy male newborns born by normal delivery or non-emergency C-section, whose mothers were at gestational age greater than 38 weeks, with positive RH and non-O blood type, without underlying illness and anemia, and referred to the Aslian Hospital (Khorramabad) or Imam Khomeini Hospital (Aleshtar) in 2017. Due to the exclusion of all possible interactions, we only selected male neonates. To prevent possible ABO and Rh HDN (hemolytic disease of the newborns), mothers with O blood group and Rh negative were excluded from the study. Any underlying disease and anemia may affect the blood indices so we excluded all mothers (and her babies) with these conditions.
Research and information gathering
In this cross-sectional study, 300 umbilical cord blood samples were taken from 300 neonates, including 150 neonates delivered naturally and 150 cases of neonates delivered by C-section. All of the newborns were of male gender and had not shown any abnormal findings in the primary examination. Subsequently, accurate records were gathered for the mothers such as maternal hospital records, information about the number of pregnancies, underlying illnesses, and hemoglobin levels. Only those mothers and infants who had met these criteria or parameters were included in the study; any mother and infant who did not have the above conditions were excluded.
Two mL blood samples from the umbilical cord were taken immediately after closing the umbilical cord and were poured in a special test tube, which contains an anti-coagulant ethylenediaminetetraacetic acid (EDTA), and slowly shaken to prevent clotting. Peripheral blood slides were immediately prepared and used for morphological examination of blood cells. Samples were analyzed by a calibrated counter (Sysmex KX 21N) in three hours. For samples that were left for more than three hours (maximum 6 hours), it was not possible to test them that day and they were placed in the refrigerator at 4oC. It should be noted that all mothers were satisfied verbally and were told that there was no danger to the baby and mother during the umbilical cord blood sampling. Blood samples were collected after clamping the umbilical cord at a site of the umbilical cord still attached to the infant.
Data Analysis
The statistical software used to analyze the data was SPSS version 11.5. Independent t-test and Mann-Whitney test were used to compare the indices between the two groups. Chi-square test was also used to measure the relationship between two qualitative variables.
Ethical Statements
This study is licensed with code LUMS.REC.1396.229 from the Ethics Committee of Lorestan University of Medical Sciences, Iran.
Results
The blood cell parameters of the 150 neonates of C-section and 150 neonates of normal delivery by mothers who were referred to Asalian Hospital (Khorramabad) and Imam Khomeini Hospital (Aleshtar), from February 19, 2017 to September 22, 2017, were examined. The mean age of the mothers was 25.9±2.65 in the vaginal delivery group and 26.4±3.45 in the cesarean group; there was no underlying disease in both groups. All mothers had RH blood+ type and were pregnant for the second time. Mothers with blood group O were excluded from the study in order to prevent possible immune interference between mother and fetus. The average maternal hemoglobin in normal delivery was 12.9±0.89 and in the C-section was 13.04±0.77. There was no significant difference between the two groups (P = 0.649).
| Row | Blood parameter | Delivery type | P-value | |
| C-section (Mean±SD) | Normal delivery (Mean±SD) | |||
| 1 | Hemoglobin (gram/dL) | 14.09±1.2 | 14.9±1.3 | <0.001 |
| 2 | Hematocrit (%) | 42±3.7 | 44±1.4 | <0.001 |
| 3 | RBC (x 10 12 /L) | 4.4±0.008 | 5.05±0.007 | <0.001 |
| 4 | MCV (femtoliter) | 106±5.7 | 107±5.9 | 0.524 |
| 5 | MCH (picogram) | 34.4±3.3 | 34.6±3.2 | 0.591 |
| 6 | MCHC (gram/dL) | 34.15±1.15 | 34.41±1.19 | 0.452 |
| 7 | RDW (%) | 16.3±3.2 | 17.94±4.1 | <0.001 |
The mean neonatal hemoglobin, hematocrit, red blood cell (RBC) count, and RDW in normal delivery were 14.9±1.3 g/dL, 44±1.4%, 5.05±0.007 x 1012/L, and 17.94±4.1%, respectively; the corresponding parameters for delivery by C-section were 14.09±1.2 g/dL, 42±3.7%, 4.4±0.008 x 1012/L, and 16.3±3.2%, respectively (Table 1). There was a significant difference between all groups (p<0.001). There were no significant differences in other RBC indices, such as mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and mean corpuscular hemoglobin concentration (MCHC) (P>0.05). The mean white blood cell (WBC), neutrophil count, and lymphocyte count of neonates in normal delivery were 18.3±8 x 109/L, 58±7%, and 34±7 %, respectively; in C-section, they were 7.78±3 x 109/L, 38±8% and 57±8%, respectively. Notably, a p-value of P <0.001 indicated that there was a significant difference between the two groups in all parameters The mean percentage of the infant’s monocytes and eosinophils in normal delivery were 4.0±0.85% and 7.1±0.36%, respectively; in cesarean delivery those values were 4±0.81 % and 1.7±0.27%, respectively (Table 2). There were no significant differences between the two groups (p=0.836).
| Row | Blood parameter | Delivery type | P-value | |
| C-section (Mean±SD) | Normal delivery (Mean±SD) | |||
| 1 | Mean neutrophil (%) | 38±8 | 58±7 | <0.001 |
| 2 | Lymphocyte (%) | 57±8 | 34±7 | <0.001 |
| 3 | Monocyte (%) | 4±0.81 | 4±0.85 | 0.836 |
| 4 | Eosinophil (%) | 1.7±0.27 | 1.7±0.36 | 0.822 |
| 5 | WBC count (x 10 9 /L) | 7.78±3 | 18.3±8 | <0.001 |
The average platelet count, mean platelet volume (MPV), and PDW of neonates of normal delivery were 305±82 x 109/L, 9.84±0.64 femtoliter (fL), and 12.18±2.03%, respectively. In those delivered by C-section, the corresponding parameters were 242±92 x 109/L, 9.87±0.65 fL, and 11.88±1.7%, respectively. There was a significant difference between all groups (P<0.001; Table 3).
| Row | Blood factor | Delivery type | P-value | |
| C-section (Mean±SD) | Normal delivery (Mean±SD) | |||
| 1 | Platelet average (x 10 9 /L) | 242±92 | 305±82 | <0.001 |
| 2 | MPV (fL) | 9.87±0.65 | 9.84±0.64 | 0.684 |
| 3 | PDW (%) | 11.88±1.7 | 12.18±2.03 | 0.637 |
The anemia rate of infants in normal delivery versus C-section was 34% versus 53%, respectively. There was significant relationship between the type of delivery and anemia (P<0.001). Also, the rate of thrombocytopenia in infants was 1% in normal delivery and 7% in C-section. Since P<0.001, this indicated a significant relationship between the type of delivery and anemia (Table 4).
| Delivery type | ||||
| Normal delivery | C-section | P-value | ||
| Anemia | Hemoglobin above 13.7 (g/dL) | 125 (83.3%) | 25 (16.7%) | <0.001 |
| Hemoglobin below 13.7 (g/dL) | 92 (61.3%) | 58 (38.7%) | ||
| Thrombocytopenia | Platelet over150 (x 10 9 /L) | 149 (0.99) | 1 (0.01) | <0.001 |
| Platelet over150 (x 10 9 /L) | 139 (0.93) | 11 (0.07) | ||
Discussion
For a long time, there has been discussion about the advantages and disadvantages of the types of childbirth on mothers and infants. Many studies have been conducted to evaluate the effects of childbirth, in various aspects, on both mother and infant. In the study herein, we evaluated 300 male term neonates for their cord blood indexes; these neonates were born from mothers who had come to Imam Khomeini Hospital (Aleshtar city) and Asalian Hospital (Khorramabad city) for selective natural childbirth or C-section, from March to September 2017. All of the selected newborns were term neonates who did not show any abnormalities in their first examination. Their mothers did not indicate any background diseases, and all of them were gravida 2 with A, B, AB or RH positive blood type. Due to the probable immunological incompatibilities between the mother and the embryo, mothers with blood type O (related to ABO hemolytic disease of the newborn, i.e. ABO HDN) 43 were excluded from the study, as were those mothers who were Rh negative.
Among the 300 neonates studied, 150 neonates were born by natural (vaginal) delivery while 150 neonates were born by selective C-section. According to the results of this study, which are based on complete blood count and peripheral blood smear taken from newborns at the beginning of birth, blood indexes such as hemoglobin, hematocrit, RBC, WBC, neutrophil count, platelet count, and RDW were higher in those newborns delivered naturally than in those delivered by C-section. Other blood indexes such as MCV, MCH, MCHC, MPV, PDW, eosinophils, and monocytes showed no differences between the two kinds of childbirth. The lymphocytes index did not show a significantly different count between the two types of childbirth. However, babies born by caesarean showed a higher percentage of relative abundance of lymphocytes than those babies born vaginally.
Past studies by others have also investigated the relationship of mode of childbirth delivery and blood indexes. For instance, in 2011, Chang et al. demonstrated that there is no meaningful relationship between the kind of delivery and blood indexes (such as MCV, MCHC and MCH) 44, which is in agreement with our study. Qaiser et al. showed in a cross-sectional study, in 2006, that there was no change in MCV, MCHC, or MCH in the two kinds of childbirth delivery 45, which is, again, in agreement with our current study. Moreover, Nikischin et al., in 1997, studied the impact of type of childbirth on the healthy and term newborn’s blood indexes. Their study was based in Germany and they demonstrated that there is no relevance between MCV, MCHC, and MCH with the type of delivery 46, which is consistent, too, with the findings of our study.
According to our study, the average hemoglobin in cord blood of babies born by natural delivery is 14.9±1.3 g/dL, and in cesarean babies is 14.09±0.2 g/dL. Therefore, infants born by normal delivery show about 0.8% higher mean hemoglobin. The hematocrit index in newborns born vaginally is 44±4.1% and in cesarean newborns is 42±3.7%; thus, the newborn hematocrit level from neonates of natural birth is approximately 2% higher than that for cesarean birth. Moreover, the RBC count in vaginal newborns was 5.05 x 106/ μL, whereas the count in cesarean newborns was 4.4 x 106/ μL (thus vaginal newborns have 600,000 RBC/ μL more than cesarean newborns).
Generally, our results were aligned with study results from Hajia Borna et al. in Tehran in 2004 47, Shahla Vaziri et al. in Ahvaz in 2003 48, Zibdad et al. at Bahman Gonabad Hospital in 2011 49, Hemmatyar et al. at Najmieh Tehran Hospital in 2005 50, Marwaha et al. in 1992 51, Sheffer et al. in 2003 52, Zhou et al. 53, Chang et al. in Taiwan in 2011 54, Wu J.H. et al. in Taiwan in 2009 55, Fady et al. in Egypt in 2013 56, Lee et al. in Korea in 1998 57, Acharya et al. in 2009 58, Eskola et al. in 2011 59, and Nogurea et al. in Bono Siro in 1999 60.
In conclusion, the mean of hematological indexes (e.g. hemoglobin, hematocrit, RBC, WBC, neutrophil count, platelet count, and RDW) were higher in neonates who were born by natural childbirth versus those born by cesarean delivery. Other blood indices such as MCV, MCH, MCHC, MPV, PDW, eosinophils, and monocytes did not show any significant difference between the two methods of delivery. On the other hand, 16.7% of normal birth infants and 38.7% of C-section birth infants had hemoglobin below 13.7 g/dL, and approximately 1% of normal birth infants and 7% of C-section birth infants had platelet counts below 150,000 platelets/ μL. Platelets below 100,000/ μL and hemoglobin < 10 g/dL were not seen in any of the newborns. The umbilical cord blood hemoglobin of the studied infants was significantly lower than the hemoglobin listed in the Nelson textbook of pediatrics (16.5±1.5). According to the results of our study, there were higher levels of beneficial blood parameters (such as hemoglobin and hematocrit) in normal birth neonates, but a higher percentage of anemia and thrombocytopenia in cesarean birth neonates.
Conclusions
In the current study, although there were some limitations, such as low sample size and few analysis techniques, the findings demonstrate that it is necessary to raise the awareness of parents about the benefits of normal delivery and to refrain them from making selective and unnecessary cesareans inasmuch as possible.
Competing Interests
The authors declare no conflict of interest in this investigation.
Authors' Contributions
Ali Asghar Kiani: Study design, data collection Majid Fathi: data collection, doing experiments Hossein Eliyasy: data collection, doing experiments Mehdi Birhjandi: data analysis Babak Abdolkarimi: data collection Parastoo Baharvand: study design, writing
Acknowledgments
The authors should be thankful from the staff of Aslian Hospital (Khorramabad) and Imam Khomeini Hospital (Aleshtar) for helping them in sample collecting.
References
-
Bohren
M. A.,
Hofmeyr
G. J.,
Sakala
C.,
Fukuzawa
R. K.,
Cuthbert
A..
Continuous support for women during childbirth. The Cochrane Library.
2017;
7
:
CD003766
.
PubMed Google Scholar -
Blyholder
L.,
Chumanov
E.,
Carr
K.,
Heiderscheit
B..
Exercise Behaviors and Health Conditions of Runners After Childbirth. Sports Health.
2017;
9
:
45-51
.
PubMed Google Scholar -
Azami-Aghdash
S.,
Ghojazadeh
M.,
Dehdilani
N.,
Mohammadi
M.,
Abad
R. Asl Amin.
Prevalence and causes of cesarean section in Iran: systematic review and meta-analysis. Iranian Journal of Public Health.
2014;
43
:
545-55
.
PubMed Google Scholar -
Vaate
A. J. Bij de,
Voet
L. F. van der,
Naji
O.,
Witmer
M.,
Veersema
S.,
Brölmann
H. A..
Prevalence, potential risk factors for development and symptoms related to the presence of uterine niches following Cesarean section: systematic review. Ultrasound in Obstetrics & Gynecology.
2014;
43
:
372-82
.
PubMed Google Scholar -
Mylonas
I.,
Friese
K..
Indications for and risks of elective cesarean section. Deutsches Ärzteblatt International.
2015;
112
:
489-95
.
PubMed Google Scholar -
Mueller
N. T.,
Whyatt
R.,
Hoepner
L.,
Oberfield
S.,
Dominguez-Bello
M. G.,
Widen
E. M..
Prenatal exposure to antibiotics, cesarean section and risk of childhood obesity. International Journal of Obesity.
2015;
39
:
665-70
.
PubMed Google Scholar -
Huang
L.,
Chen
Q.,
Zhao
Y.,
Wang
W.,
Fang
F.,
Bao
Y..
Is elective cesarean section associated with a higher risk of asthma? A meta-analysis. The Journal of Asthma.
2015;
52
:
16-25
.
PubMed Google Scholar -
Myers
S. A.,
Gleicher
N..
A successful program to lower cesarean-section rates. The New England Journal of Medicine.
1988;
319
:
1511-6
.
PubMed Google Scholar -
Taffel
S. M.,
Placek
P. J.,
Liss
T..
Trends in the United States cesarean section rate and reasons for the 1980-85 rise. American Journal of Public Health.
1987;
77
:
955-9
.
PubMed Google Scholar -
Osser
O. V.,
Jokubkiene
L.,
Valentin
L..
High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound in Obstetrics & Gynecology.
2009;
34
:
90-7
.
PubMed Google Scholar -
Tower
A. M.,
Frishman
G. N..
Cesarean scar defects: an underrecognized cause of abnormal uterine bleeding and other gynecologic complications. Journal of Minimally Invasive Gynecology.
2013;
20
:
562-72
.
PubMed Google Scholar -
Negahban
T,
Ansari Jaberei
A,
Kazemi
M.
The preferred delivery method and influenced factors from view of pregnant women referred to Rafsanjan city health and treatment units and clinics. Rafsanjan Uni Med Sci J.
2006;
5
:
161-168
.
-
Patel
R. R.,
Liebling
R. E.,
Murphy
D. J..
Effect of operative delivery in the second stage of labor on breastfeeding success. Birth (Berkeley, Calif.).
2003;
30
:
255-60
.
PubMed Google Scholar -
Jonas
K.,
Johansson
L. M.,
Nissen
E.,
Ejdebäck
M.,
Ransjö-Arvidson
A. B.,
Uvnäs-Moberg
K..
Effects of intrapartum oxytocin administration and epidural analgesia on the concentration of plasma oxytocin and prolactin, in response to suckling during the second day postpartum. Breastfeeding Medicine.
2009;
4
:
71-82
.
PubMed Google Scholar -
Soltanpour
M.S.,
Soheili
Z.,
Pourfathollah
A.A.,
Samiei
S.H.,
Meshkani
R.,
Kiani
A.A,
Majid
S.,
Ataei
A.,
Kavari
M..
The A1298C Mutation in Methylenetetrahydrofolate Reductase Gene and Its Association With Idiopathic Venous Thrombosis in an Iranian Population. Laboratory Medicine.
2011;
42
(v)
:
213-216
.
-
Verster
A,
Mannaerts
D,
Van Der Veken
L,
De Maeyer
K,
Coppejans
H,
Jacquemyn
Y.
Protocol for a randomized trial on nausea, vomitus and arterial hypotension comparing carbetocin and oxytocin as prevention for hemorrhage after cesarean section. International Journal of Clinical Trials.
2017;
4
:
28-30
.
-
Victora
C. G.,
Bahl
R.,
Barros
A. J.,
França
G. V.,
Horton
S.,
Krasevec
J.,
Series
Group Lancet Breastfeeding.
Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet.
2016;
387
:
475-90
.
PubMed Google Scholar -
Wambach
Karen,
Riordan
Jan.
2014.
Google Scholar -
Cravioto
A.,
Tello
A.,
Villafán
H.,
Ruiz
J.,
Vedovo
S. del,
Neeser
J. R..
Inhibition of localized adhesion of enteropathogenic Escherichia coli to HEp-2 cells by immunoglobulin and oligosaccharide fractions of human colostrum and breast milk. The Journal of Infectious Diseases.
1991;
163
:
1247-55
.
PubMed Google Scholar -
Kumar
Tarun,
Kumar
Sanjay,
Sunita
Manish Kumar,
Jhillmill
Anju,
Sharan
Ashok.
Study on Effects of Exclusive Breastfeeding on Immunity of Infants. Prof. RK Sharma.
2016;
7
:
2300
.
-
Bridgman
S. L.,
Konya
T.,
Azad
M. B.,
Sears
M. R.,
Becker
A. B.,
Turvey
S. E.,
null
null.
Infant gut immunity: a preliminary study of IgA associations with breastfeeding. Journal of Developmental Origins of Health and Disease.
2016;
7
:
68-72
.
PubMed Google Scholar -
Koczo
Agnes,
Marino
Amy,
Jeyabalan
Arun,
Elkayam
Uri,
Cooper
Leslie,
Fett
James,
McTiernan
Charles,
Morel
Penelope,
Hanley-Yanez
Karen,
McNamara
Dennis.
Cellular Immune Activation and Breastfeeding in Peripartum Cardiomyopathy. 2017
.
-
Newburg
D. S.,
Peterson
J. A.,
Ruiz-Palacios
G. M.,
Matson
D. O.,
Morrow
A. L.,
Shults
J..
Role of human-milk lactadherin in protection against symptomatic rotavirus infection. Lancet.
1998;
351
:
1160-4
.
PubMed Google Scholar -
Ip
S.,
Chung
M.,
Raman
G.,
Trikalinos
T. A.,
Lau
J..
A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeeding Medicine.
2009;
4
:
S17-30
.
PubMed Google Scholar -
Verhasselt
Valerie.
Is infant immunization by breastfeeding possible?. Phil. Trans. R. Soc. B.
2015;
370
:
20140139
.
-
Turfkruyer
M.,
Verhasselt
V..
Breast milk and its impact on maturation of the neonatal immune system. Current Opinion in Infectious Diseases.
2015;
28
:
199-206
.
PubMed Google Scholar -
Maschmann
J.,
Goelz
R.,
Witzel
S.,
Strittmatter
U.,
Steinmassl
M.,
Jahn
G..
Characterization of human breast milk leukocytes and their potential role in cytomegalovirus transmission to newborns. Neonatology.
2015;
107
:
213-9
.
PubMed Google Scholar -
Cecunjanin
Zuvdija,
Selimović
Amina,
Milišić
Selma,
Muji\vcić
Ermina.
ASSESSMENT OF HEMATOLOGICAL PARAMETERS, ACID-BASE STATUS AND ARTERIAL BLOOD GAS TEST BEFORE AND AFTER TREATMENT OF ACUTE BRONCHIOLITIS IN CHILDREN. International Journal of Surgery and Medicine.
2016;
2
(3)
:
1-1
.
-
Panwar
Champa,
Kaushik
Shyam L,
Kaushik
Rajni,
Sood
Arvind.
Correlation of neonatal and maternal clinico-hematological parameters as predictors of early onset neonatal sepsis. International Journal of Contemporary Pediatrics.
2016;
4
:
36-42
.
-
Gholami
M.,
Abbaszadeh
A.,
Khayat
Z. Khanipour,
K. Anbari,
Baharvand
P.,
Gharravi
A.M..
Honey improves spermatogenesis and hormone secretion in testicular ischaemia-reperfusion-induced injury in rats. Andrologia.
2018;
50
(1)
:
e12804
.
PubMed Google Scholar -
Clark
K. M.,
Li
M.,
Zhu
B.,
Liang
F.,
Shao
J.,
Zhang
Y..
Breastfeeding, mixed, or formula feeding at 9 months of age and the prevalence of iron deficiency and iron deficiency anemia in two cohorts of infants in China. The Journal of Pediatrics.
2017;
181
:
56-61
.
PubMed Google Scholar -
Bhandari
Sushila Devi,
Joshi
Sarala.
Perception and perceived experiences about prevention and consequences of teenage pregnancy and childbirth among teenage mothers: A qualitative study. Journal of Advanced Academic Research.
2017;
3
:
164-172
.
-
Ganchimeg
T.,
Ota
E.,
Morisaki
N.,
Laopaiboon
M.,
Lumbiganon
P.,
Zhang
J.,
null
null.
Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multicountry study. BJOG.
2014;
121
:
40-8
.
PubMed Google Scholar -
Johns
L. E.,
Ferguson
K. K.,
Soldin
O. P.,
Cantonwine
D. E.,
Rivera-González
L. O.,
Toro
L. V. Del.
Urinary phthalate metabolites in relation to maternal serum thyroid and sex hormone levels during pregnancy: a longitudinal analysis. Reproductive Biology and Endocrinology.
2015;
13
:
4
.
PubMed Google Scholar -
Butler
A. M.,
Charoensiriwatana
W.,
Krasao
P.,
Pankanjanato
R.,
Thong-Ngao
P.,
Polson
R. C..
Newborn Thyroid Screening: Influence of Pre-Analytic Variables on Dried Blood Spot Thyrotropin Measurement. Thyroid.
2017;
27
:
1128-34
.
PubMed Google Scholar -
Orlandini
C.,
Torricelli
M.,
Spirito
N.,
Alaimo
L.,
Tommaso
M. Di,
Severi
F. M..
Maternal anemia effects during pregnancy on male and female fetuses: are there any differences?. The Journal of Maternal-Fetal & Neonatal Medicine.
2017;
30
:
1704-8
.
PubMed Google Scholar -
Dodd
JM,
Grivell
RM,
O’Brien
C,
Dowswell
T,
Deussen
AR.
Prenatal administration of progestogens for preventing preterm birth in women with a multiple pregnancy. Cochrane Database of Systematic Reviews.
2016
.
-
Herruzo
A. J.,
Mozas
J.,
Alarcón
J. L.,
López
J. M.,
Molina
R.,
Molto
L..
Sex differences in serum hormone levels in umbilical vein blood. International Journal of Gynaecology and Obstetrics: the Official Organ of the International Federation of Gynaecology and Obstetrics.
1993;
41
:
37-41
.
PubMed Google Scholar -
Cunningham
F. G.,
Leveno
K. J.,
Bloom
S. L.,
Hauth
J. C.,
Gilstrap
L. C.,
Wenstrom
K. D..
2005.
Google Scholar -
Kliegman
RM,
Stoll
BJ.
Anemia in the newborn in fant, blood disorders, non infectious disorders, the fetus and the neonatal infant. Behrman RE., kligman RM. Arvin, AM. Nelson textbook of pediatrics.
2004;
:
599-601
.
-
Reinhardt
M. C.,
Marti
H. R..
Haematological data of African newborns and their mothers in Abidjan. Helvetica Paediatrica Acta. Suppl..
1978;
:
85-99
.
PubMed Google Scholar -
Darvish
Soodabeh,
Etemad
Koorosh,
Mosaheb
Azar,
Yazdanpanah
Ghasem.
Comparing Maternal and Neonatal Side Effects of Natural Vaginal Delivery under Neuro-Axial Analgesia with Usual Vaginal Delivery and Cesarean Section: A Primary Single Center Study. J Obstet Gynecol Cancer Res. In Press (In Press): e11411. Published online.
2017
.
-
Firouzi
M.,
Yazdanmehr
R.,
Elyasi
H.,
Birjandi
M.,
Goudarzi
A.,
Almasian
M..
The prevalence of the ABO hemolytic disease of the newborn and its complications in an Iranian population. Iranian Journal of Pediatric Hematology and Oncology.
2018;
7
:
37-47
.
-
Chang
Y. H.,
Yang
S. H.,
Wang
T. F.,
Lin
T. Y.,
Yang
K. L.,
Chen
S. H..
Complete blood count reference values of cord blood in Taiwan and the influence of gender and delivery route on them. Pediatrics and Neonatology.
2011;
52
:
155-60
.
PubMed Google Scholar -
Qaiser
Danish Hasan,
Sandila
Mohammad Perwaiz,
Kazmi
Tahseen,
Ahmed
Syed Tousif.
Influence of maternal factors on hematological parameters of healthy newborns of Karachi. Pakistan Journal of Physiology.
2009;
5
:
34-37
.
-
Nikischin
W.,
Peter
M.,
Oldigs
H. D..
The influence of mode of delivery on hematologic values in the umbilical vein. Gynecologic and Obstetric Investigation.
1997;
43
:
104-7
.
PubMed Google Scholar -
Boma
H.,
Borna
S.,
Rafati
S. H..
Haji Ebrahimi Tehrani.Umbilical cord hematologic in different mode of delivery. Tehran University Medical Journal.
2006;
64
:
49-56
.
-
Vaziri Esfarjani
Sh.
Asgharinejad L. Correlation beetwean mean hemoglobin of umblicul cord who were borned in razi hospital. Majallah-i Danishkadah-i Pizishki-i Isfahan.
2006;
82
:
21-5
.
-
Zibad
H. A.,
Moghadam
K. B.,
Moghadam
M. B.,
Binabaj
N. B.,
Rafat
E..
The Correlation between Type of Delivery and Umbilical Cord Blood Hemoglobin and Hematocrit in Full-Term Neonates. Majallah-i Danishkadah-i Pizishki-i Isfahan.
2012;
29
.
-
Hematyar
M,
Ekhtiari
A.
Correlation between neonatal cord blood hemoglobin and hematocrit with mode of delivery. JQUMS.
2008;
12
:
22-3
.
-
Marwaha
N.,
Marwaha
R. K.,
Narang
A.,
Thusu
K.,
Garewal
G.,
Bhakoo
O. N..
Routine hematological values in term newborns. Indian Pediatrics.
1992;
29
:
1095-9
.
PubMed Google Scholar -
Sheffer-Mimouni
G.,
Mimouni
F. B.,
Lubetzky
R.,
Kupferminc
M.,
Deutsch
V.,
Dollberg
S..
Labor does not affect the neonatal absolute nucleated red blood cell count. American Journal of Perinatology.
2003;
20
:
367-71
.
PubMed Google Scholar -
Zhou
Y. B.,
Li
H. T.,
Zhu
L. P.,
Liu
J. M..
Impact of cesarean section on placental transfusion and iron-related hematological indices in term neonates: a systematic review and meta-analysis. Placenta.
2014;
35
:
1-8
.
PubMed Google Scholar -
Chang
Y. H.,
Yang
S. H.,
Wang
T. F.,
Lin
T. Y.,
Yang
K. L.,
Chen
S. H..
Complete blood count reference values of cord blood in Taiwan and the influence of gender and delivery route on them. Pediatrics and Neonatology.
2011;
52
:
155-60
.
PubMed Google Scholar -
Wu
J. H.,
Chou
H. C.,
Chen
P. C.,
Jeng
S. F.,
Chen
C. Y.,
Tsao
P. N..
Impact of delivery mode and gestational age on haematological parameters in Taiwanese preterm infants. Journal of Paediatrics and Child Health.
2009;
45
:
332-6
.
PubMed Google Scholar -
Fady
M.,
Alif
A.,
Maha
M.,
Rania
K..
Haematological parameters of newborns delivered vaginally versus caesarean section. Menoufia Medical Journal.
2016;
29
:
259-64
.
-
Lee
H. R.,
Shin
S.,
Yoon
J. H.,
Kim
B. J.,
Hwang
K. R.,
Kim
J. J..
[Complete blood count reference values of donated cord blood from Korean neonates]. The Korean Journal of Laboratory Medicine.
2009;
29
:
179-84
.
PubMed Google Scholar -
Acharya
G.,
Sitras
V..
Oxygen uptake of the human fetus at term. Acta Obstetricia et Gynecologica Scandinavica.
2009;
88
:
104-9
.
PubMed Google Scholar -
Eskola
M.,
Juutistenaho
S.,
Aranko
K.,
Sainio
S.,
Kekomäki
R..
Association of cord blood platelet count and volume with hemoglobin in healthy term infants. Journal of Perinatology.
2011;
31
:
258-62
.
PubMed Google Scholar -
Noguera
Nelida I,
Detarsio
German,
Perez
Susana M,
Bragos
Irma M,
Lanza
Olga,
Rodriguez
Jose H,
Acosta
Irma,
Davoli
Ruben,
Milani
Angela C.
Hematologic study of newborn umbilical cord blood. MEDICINA-BUENOS AIRES-.
1999;
59
:
446-448
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 10 (2018)
Page No.: 2768-2775
Published on: 2018-10-27
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 7122 times
- Download PDF downloaded - 2045 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress

