Abstract
Introduction: Plasmodium falciparum has developed resistance to artemisinin drugs in Southeast Asia, and its reduced sensitivity has been reported in other regions. This study aims to determine parasite susceptibility to the bioactive form of artemisinin derivatives- dihydroartemisinin (DHA)-, and to detect the K13 polymorphism in isolates from an endemic area of Nigeria.
Methods: Ex-vivo response in 55 parasites isolates obtained from malaria-positive patients were exposed to pulse DHA concentration and cultured for 66 hours ex-vivo. Parasite ring stage survival (RSAex-vivo) relative to unexposed matched control was determined by microscopy, and parasite growth was compared using Mann-Whitney U-test at a significance level of P<0.05. The Kelch propeller gene was amplified using specific primers, then sequenced and analyzed for single nucleotide polymorphisms (SNPs), which were compared to reference PF3D7_1343700.
Results: Overall, 151 of 375 (40.2%) individuals were positive during the study period. In 55 selected isolates, there was increased growth in unexposed wells but growth was inhibited in DHA-exposed wells, with growth rate between 14.9 – 96.7%. The mean RSAex-vivo value was 0.18 ± 0.09%, 95% CI (0.15-0.20). There was no significant mutation of the K13 gene in the parasite isolates evaluated.
Conclusions: Plasmodium falciparum isolates from this endemic area show high sensitivity to dihydroartemisinin ex-vivo, with no mutations conferring artemisinin resistance. Continuous monitoring of parasite susceptibility to artemisinin combination drugs should be intensified to reduce chances of artemisinin resistance in endemic areas.
Introduction
Artemisinin combination treatments (ACTs) have been widely adopted for the treatment of falciparum malaria control globally 1. However, in some areas in Southeast (SE) Asia, artemisinin-resistant parasites have emerged2345678. In highly endemic African countries, it is essential to constantly monitor susceptibility to artemisinin derivatives and ACTs. In Asia, an emergence of artemisinin-resistant parasites have been confirmed with declining sensitivity in-vitro and in-vivo to artemisinin 9101112, whereby the parasites remain in quiescent or dormant state, and exhibit phenotypic delayed clearance from peripheral blood 131415. These parasites have ring stage survival value >1, delayed parasite clearance in-vivo, and polymorphisms of the Kelch propeller (K13) gene that confers resistance to artemisinin drugs 678141516. These form the basis for detection and confirmation of parasite resistance to artemisinin drugs globally 17.
Susceptibility of Plasmodium falciparum to non-artemisinin drugs can be determined by comparing IC50 values with a sensitive strain. However, this method fails to correctly predict parasite susceptibility to artemisinin 3. Determining the survival of the ring stage parasite in-vitro or ex-vivo is a more robust method for detection of susceptibility to artemisinins 16. In Nigeria, reports of in-vitro declining response to artemisinin and its association with mutations of transporter genes have been previously reported 1819. Yet, there are few studies that assess in-vivo or ex-vivo susceptibility of P. falciparum to artemisinin and assess the K13 gene polymorphism in the parasites; one study has reported no polymorphisms of the K13 gene in Nigerian isolates 20. The World Health Organization (WHO) recommends continuous monitoring of responses to ACTs to curb the spread of resistance to other areas 17. Therefore, the aim of this study was to evaluate the ring stage survival of P. falciparum isolates and the K13 gene polymorphism in a high malaria hotspot in Africa.
Methods
Study population
The study population was a cohort from a larger population of 375 individuals who were part of an on-going community health survey in Ota, Nigeria, evaluating malaria prevalence and markers of antimalarial drug resistance in an endemic area. Data from this population has been published in part previously 21. The sub-population included for the current study were children and adults (aged > 6months) with P. falciparum mono-infection and parasitemia between 1-5% as detectable by microscopy. Persons with baseline parasitemia <1% were excluded from this evaluation. Informed consent was sought from the participants and ethical approval was sought from local authorities and the Covenant Health Research Ethics Committee, Nigeria.
Sample collection
Venous blood from 55 malaria positive subjects who met the inclusion criteria was taken aseptically into EDTA bottles, and blood was spotted on slides for thin and thick film microscopy to confirm P. falciparum mono-infection. The samples were transported to the laboratory on ice for further processing.
Laboratory analysis
Blood samples were washed twice in RPMI 1640 medium (Sigma Aldrich, USA), centrifuged at 2500 x g and made up to 1.5% hematocrit and 1% parasitemia. Ex-vivo ring stage survival assay (RSAex-vivo) was performed within 24 hours of blood collection without culture adaptation according to a previously established method 16. Briefly, dilution of stock of dihydroartemisinin (DHA) (1mg/mL) was made in a final volume of 900 µL complete medium supplemented with pooled human serum, and 100 µL infected erythrocyte suspension was added to test drug wells and exposed for 6 hours; each sample was cultured in triplicates. The samples were transferred to a 1.5 mL tube and washed twice, then maintained in culture for another 66 hours at 37°C using the candle jar method of Trager and Jensen 22. Drug-unexposed wells for each sample served as control. The culture was terminated after 66 hours of growth and the pellet from the suspension was used to make thin smears, which were fixed in methanol and stained with Giemsa for determination of ring stage growth at 100x magnification by light microscopy. The proportion of viable parasites (survival) in DHA exposed/unexposed wells was expressed as a percentage. RSAex-vivo values >1 was taken to indicate artemisinin resistance 1617.
Molecular analysis
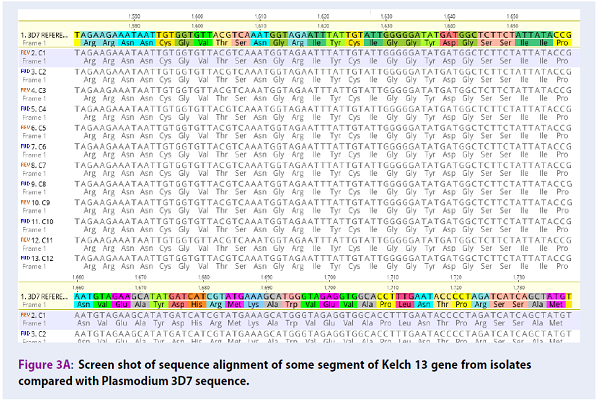
Parasite DNA was extracted and amplified using previously published methods with primers specific for blade 6 of the K13 gene 6; next, 10 µL of the secondary product was resolved on 2% agarose gel to confirm amplification. The secondary amplicons of a few isolates were sent for sequencing at Inqaba Biotech West Africa Ltd (South Africa). The sequences were deposited in GenBank with accession numbers MH464876-464887. Polymorphisms in the parasite isolates encoding the Kelch propeller (K13) protein were compared with PF3D7_1343700 reference gene (sequence region spanning region 1,724,817-1,726,997 bp of chromosome 13 downloaded from www.plasmoDB.org). The sequence was analyzed for molecular markers of artemisinin resistance: SNPs at codons Y493H, R539T, I543T, and C580Y, and any mutations of the gene (using Geneious software version 11.6.1). The data are reported as mean ± standard deviation, 95% confidence interval (CI) for continuous data; P-value of < 0.05 indicates a significant difference. Sequence alignments with reference to 3D7 are shown in the Appendix.
Results
During the study period, a parasite prevalence of 40.2% (151 had detectable parasitemia) was recorded from the cohort of 375 individuals tested for malaria infection. From this population, 55 positive samples meeting the inclusion criteria were cultured to evaluate the ex-vivo response of P. falciparum to DHA. At baseline, the geometric mean parasitemia in the 55 samples was 1800/µL blood [95% confidence interval: 1823 – 2974/ µL blood]. The mean age ± SEM was 9.82 ± 1.02 years, range [0.5 – 40 years], and 26 (47%) of them were males.
Ring stage survival rates
The parasite growth rate in drug unexposed control wells was significantly higher than exposed well (P < 0.001), ranging from 14.9 – 96.7%. The mean value of parasite ring stage survival after 6 hours of DHA exposure (RSAex-vivo) in the drug-exposed wells was 0.18 ± 0.09%, 95% confidence interval [0.15 -0.20%]. Figure 1 shows the distribution of individual RSAex-vivo values obtained after exposure to 700 nM DHA. One parasite isolate had a high RSAex-vivo value of 0.8%. The amplified K13 gene from this isolate (C5) and other randomly selected samples are shown in Figure 2, with gene size of 849 bp.
K13 gene polymorphism
Six of the 55 (10%) isolates were analyzed for the K13 gene polymorphism and compared with the reference 3D7 strain using the standard bi-directional sequence alignment (Figure 3Figure 4Figure 5). There were polymorphisms of 2 isolates (C1 and C11) on single strands of the DNA (this was taken to be reading errors and not mutations). No SNPs were observed at codons C580, Y493H, R539T, I543T, R561H or N458Y, all of which are validated molecular markers of artemisinin resistance in the Mekong Sub-region, Southeast Asia 17. Similarly, there were no SNPs at codon A578S and A675V, which are K13 polymorphisms reported in some African regions.
Discussion
Development of resistance by P. falciparum to all antimalarial drugs (including artemisinin derivatives) is a major problem limiting malaria elimination globally 17. In SE Asia, isolates resistant to artemisinin have developed several mutations in the Kelch propeller gene 56. Candidate markers which confer resistance to other ACTs, such as dihydroartemisinin-piperaquine 23, have been identified. Six of these markers (i.e. SNPs at codon C580Y, Y493H, R539T, I543T, R561H, and N458Y) have been validated as artemisinin resistance markers in the Greater Mekong sub-region 17. However, in Africa, reduced susceptibility to artemisinin and ACTs 24 and limited mutations in the Kelch 13 gene 1720252627 with no associated artemisinin resistance have been reported 282930313233.
Continuous monitoring of parasite responses to individual components of the recommended ACTs should indicate any early emergence of resistance and serve to preserve the efficiency of available anti-malarials in endemic areas. In Nigeria, studies indicate that malaria transmission is still high 2134, with recent studies from regions in Nigeria reporting high mutations in genes that modulate response to non-artemisinin drugs by P. falciparum 353637. Conversely, other studies have reported high in-vivo response after ACTs with parasitemia half-life <5 hours, and 42-day cure rates >90% 38. However, few studies elsewhere have recently evaluated the WHO benchmarks for artemisinin resistance using RSA value and K13 gene polymorphism 1720. From the mean RSA of 0.18%, determined in the small parasite population evaluated in this study together with no molecular marker of resistance, it can be implied that parasites susceptible to artemisinin are prevalent. Development of the ring stage survival assay for the in-vitro or ex-vivo detection of artemisinin resistance abrogates the challenge of inconsistent in-vitro results and provides a simple tool for resource-poor countries for the detection of artemisinin resistance even with small sample size 56.
The findings of the present study support previous reports of limited artemisinin resistance in Africa 282930313233. This, however, does not undermine the need for continuous monitoring of response to artemisinin and ACTs in endemic areas to mark the beginning of declining resistance to both components of ACTs, to prevent the consequences of high morbidity and mortality in the future, and to curb the spread of artemisinin-resistant parasites to Africa where consequences will be intense 1. As part of strategies devised to contain the spread of artemisinin resistance, active monitoring of parasite responses and markers of artemisinin resistance in different areas is advocated as regional differences in parasite response may exist in Nigeria 38. A potential challenge will be to identify and validate resistance markers if unique markers exist in other areas. It is pertinent to monitor possible emergence in Africa from detected Kelch 13 SNP on codon A578S reported in some African countries (e.g. Kenya) 825, M579I in China (apparently imported from Guinea, Africa) 26, and A675V in Uganda 28, as well as other un-validated non-synonymous SNPs 17 in regions outside of Southeast Asia.
A wide range of SNPs in the K13 propeller gene developing independently from Asia, Africa and other regions 2526272930312345678323328 calls for further research on emerging resistance and other factors that drive mutations in the malaria parasite. Furthermore, chances of emerging artemisinin resistance will increase with increasing resistance to the artemisinin drugs, as this will gradually increase drug pressure on artemisinin in endemic areas where malaria transmission is high 2134. Since clinical drug failure attributable to artemisinin has not been established, the genetic background of P. falciparum isolates reported in this and another study 20 will aid in the early detection of mutations of the Kelch 13 domain in the parasite if artemisinin resistance develops in Nigeria. Some limitations of the current study include a small sample size of DNA that was sequenced, as well as sampling was done only in communities from one regional area (Ota, Nigeria). This may not truly represent the entire parasite population in the country.
Conclusion
This study reports a high susceptibility of parasites to artemisinin and no K13 polymorphism in the study area. As part of malaria elimination strategies, it is recommended that large-scale genomic studies be done routinely in the future to scale up monitoring of responses to artemisinin and its partner drugs in order to reduce the chances of development of resistance.
Competing Interests
The authors hereby declare there are no conflicts of interest associated with this work.
Authors' Contributions
TMD and GIO participated in the design, conduct, analysis and writing of the manuscript; DOO, CUA, AEA, OAO, CJE, GSJ participated in the conduct and analysis of the study.
Abbreviations
ACTs: artemisinin based combination treatments
DHA: Dihydroartemisinin
K13: Kelch 13 propeller gene
RSA(ex-vivo): ring stage survival assay ex-vivo
Acknowledgments
This research received publication funding support from Covenant University Centre for Research, Innovation and Discovery (CUCRID), Nigeria.
References
-
WHO
World malaria report 2017. World Health Organisation.
2017
.
-
Noedl
H.,
Se
Y.,
Schaecher
K.,
Smith
B. L.,
Socheat
D.,
Fukuda
M. M.,
Artemisinin Resistance in Cambodia 1 Study
Consortium.
Evidence of artemisinin-resistant malaria in western Cambodia. The New England Journal of Medicine.
2008;
359
:
2619-20
.
-
Dondorp
A. M.,
Nosten
F.,
Yi
P.,
Das
D.,
Phyo
A. P.,
Tarning
J..
Artemisinin resistance in Plasmodium falciparum malaria. The New England Journal of Medicine.
2009;
361
:
455-67
.
-
Tun
K. M.,
Imwong
M.,
Lwin
K. M.,
Win
A. A.,
Hlaing
T. M.,
Hlaing
T..
Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. The Lancet. Infectious Diseases.
2015;
15
:
415-21
.
-
Ashley
E. A.,
Dhorda
M.,
Fairhurst
R. M.,
Amaratunga
C.,
Lim
P.,
Suon
S.,
Tracking Resistance to Artemisinin
Collaboration.
Spread of artemisinin resistance in Plasmodium falciparum malaria. The New England Journal of Medicine.
2014;
371
:
411-23
.
-
Ariey
F.,
Witkowski
B.,
Amaratunga
C.,
Beghain
J.,
Langlois
A. C.,
Khim
N..
A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature.
2014;
505
:
50-5
.
-
Phyo
A. P.,
Nkhoma
S.,
Stepniewska
K.,
Ashley
E. A.,
Nair
S.,
McGready
R..
Emergence of artemisinin-resistant malaria on the western border of Thailand: a longitudinal study. Lancet.
2012;
379
:
1960-6
.
-
Ménard
D.,
Khim
N.,
Beghain
J.,
Adegnika
A. A.,
Shafiul-Alam
M.,
Amodu
O..
A Worldwide Map of Plasmodium falciparum K13-Propeller Polymorphisms. The New England Journal of Medicine.
2016;
374
:
2453-64
.
-
Imwong
M.,
Suwannasin
K.,
Kunasol
C.,
Sutawong
K.,
Mayxay
M.,
Rekol
H..
The spread of artemisinin-resistant Plasmodium falciparum in the Greater Mekong subregion: a molecular epidemiology observational study. The Lancet. Infectious Diseases.
2017;
17
:
491-7
.
-
Straimer
J.,
Gnädig
N. F.,
Witkowski
B.,
Amaratunga
C.,
Duru
V.,
Ramadani
A. P..
Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science.
2015;
347
:
428-31
.
-
Kyaw
M. P.,
Nyunt
M. H.,
Chit
K.,
Aye
M. M.,
Aye
K. H.,
Aye
M. M..
Reduced susceptibility of Plasmodium falciparum to artesunate in southern Myanmar. PLoS One.
2013;
8
:
e57689
.
-
Witkowski
B.,
Khim
N.,
Chim
P.,
Kim
S.,
Ke
S.,
Kloeung
N..
Reduced artemisinin susceptibility of Plasmodium falciparum ring stages in western Cambodia. Antimicrobial Agents and Chemotherapy.
2013;
57
:
914-23
.
-
Teuscher
F.,
Gatton
M. L.,
Chen
N.,
Peters
J.,
Kyle
D. E.,
Cheng
Q..
Artemisinin‐induced dormancy in plasmodium falciparum: duration, recovery rates, and implications in treatment failure. The Journal of Infectious Diseases.
2010;
202
:
1362-8
.
-
Witkowski
B.,
Lelièvre
J.,
Barragán
M. J.,
Laurent
V.,
Su
X. Z.,
Berry
A..
Increased tolerance to artemisinin in Plasmodium falciparum is mediated by a quiescence mechanism. Antimicrobial Agents and Chemotherapy.
2010;
54
:
1872-7
.
-
Amaratunga
C.,
Sreng
S.,
Suon
S.,
Phelps
E. S.,
Stepniewska
K.,
Lim
P..
Artemisinin-resistant Plasmodium falciparum in Pursat province, western Cambodia: a parasite clearance rate study. The Lancet. Infectious Diseases.
2012;
12
:
851-8
.
-
Network
Worldwide Antimalarial Resistance.
Ring-stage Survival Assays (RSA) to evaluate the in-vitro and ex-vivo susceptibility of Plasmodium falciparum to artemisinins. 2015
.
-
WHO
Status report on artemisinin and ACT resistance. World Health Organisation.
2017
.
-
Bustamante
C.,
Folarin
O. A.,
Gbotosho
G. O.,
Batista
C. N.,
Mesquita
E. A.,
Brindeiro
R. M..
In vitro-reduced susceptibility to artemether in P. falciparum and its association with polymorphisms on transporter genes. The Journal of Infectious Diseases.
2012;
206
:
324-32
.
-
Oduola
A. M.,
Sowunmi
A.,
Milhous
W. K.,
Kyle
D. E.,
Martin
R. K.,
Walker
O..
Innate resistance to new antimalarial drugs in Plasmodium falciparum from Nigeria. Transactions of the Royal Society of Tropical Medicine and Hygiene.
1992;
86
:
123-6
.
-
Kamau
E.,
Campino
S.,
Amenga-Etego
L.,
Drury
E.,
Ishengoma
D.,
Johnson
K..
K13-propeller polymorphisms in Plasmodium falciparum parasites from sub-Saharan Africa. African Journal of Infectious Diseases.
2015;
211
:
1352-5
.
-
Dokunmu
T. M.,
Olasehinde
G. I.,
Oladejo
D. O.,
Olanrewaju
O.,
Akinbobola
A.,
Adjekukor
C. U..
Efficiency of histidine rich protein II-based rapid diagnostic tests for monitoring malaria transmission intensities in an endemic area. AIP Conference Proceedings.
2018;
1954
:
030001
.
-
Trager
W.,
Jenson
J. B..
Cultivation of malarial parasites. Nature.
1978;
273
:
621-2
.
-
Amato
R.,
Lim
P.,
Miotto
O.,
Amaratunga
C.,
Dek
D.,
Pearson
R. D..
Genetic markers associated with dihydroartemisinin-piperaquine failure in Plasmodium falciparum malaria in Cambodia: a genotype-phenotype association study. The Lancet. Infectious Diseases.
2017;
17
:
164-73
.
-
Borrmann
S.,
Sasi
P.,
Mwai
L.,
Bashraheil
M.,
Abdallah
A.,
Muriithi
S..
Declining responsiveness of Plasmodium falciparum infections to artemisinin-based combination treatments on the Kenyan coast. PLoS One.
2011;
6
:
e26005
.
-
de Laurent
Z. R.,
Chebon
L. J.,
Ingasia
L. A.,
Akala
H. M.,
Andagalu
B.,
Ochola-Oyier
L. I..
Polymorphisms in the K13 gene in Plasmodium falciparum from different malaria transmission areas of Kenya. The American Journal of Tropical Medicine and Hygiene.
2018;
98
:
1360-6
.
-
Lu
F.,
Culleton
R.,
Zhang
M.,
Ramaprasad
A.,
von Seidlein
L.,
Zhou
H..
Emergence of indigenous artemisinin-resistant Plasmodium falciparum in Africa. The New England Journal of Medicine.
2017;
376
:
991-3
.
-
Li
J.,
Chen
J.,
Xie
D.,
Eyi
U. M.,
Matesa
R. A.,
Ondo Obono
M. M..
Limited artemisinin resistance-associated polymorphisms in Plasmodium falciparum K13-propeller and PfATPase6 gene isolated from Bioko Island, Equatorial Guinea. International Journal for Parasitology. Drugs and Drug Resistance.
2016;
6
:
54-9
.
-
Ikeda
M.,
Kaneko
M.,
Tachibana
S. I.,
Balikagala
B.,
Sakurai-Yatsushiro
M.,
Yatsushiro
S..
artemisinin-resistant Plasmodium falciparum with high survival rates, Uganda, 2014–2016. Emerging Infectious Diseases.
2018;
24
:
718-26
.
-
Taylor
S. M.,
Parobek
C. M.,
DeConti
D. K.,
Kayentao
K.,
Coulibaly
S. O.,
Greenwood
B. M..
Absence of putative artemisinin resistance mutations among Plasmodium falciparum in Sub-Saharan Africa: a molecular epidemiologic study. The Journal of Infectious Diseases.
2015;
211
:
680-8
.
-
Torrentino-Madamet
M.,
Fall
B.,
Benoit
N.,
Camara
C.,
Amalvict
R.,
Fall
M..
Limited polymorphisms in k13 gene in Plasmodium falciparum isolates from Dakar, Senegal in 2012-2013. Malaria Journal.
2014;
13
:
472
.
-
Heuchert
A.,
Abduselam
N.,
Zeynudin
A.,
Eshetu
T.,
Löscher
T.,
Wieser
A..
Molecular markers of anti-malarial drug resistance in southwest Ethiopia over time: regional surveillance from 2006 to 2013. Malaria Journal.
2015;
14
:
208
.
-
Escobar
Carlos,
Pateira
Sara,
Lobo
Elsa,
Lobo
Lis,
Teodosio
Rosa,
Dias
Fernanda,
Fernandes
Natercia,
Arez
Ana Paula,
Varandas
Luis,
Nogueira
Fatima.
Polymorphisms in Plasmodium falciparum K13-propeller in Angola and Mozambique after the introduction of the ACTs. PLoS One.
2015;
10
(3)
:
e0119215
.
-
Conrad
M. D.,
Bigira
V.,
Kapisi
J.,
Muhindo
M.,
Kamya
M. R.,
Havlir
D. V..
Polymorphisms in K13 and falcipain-2 associated with artemisinin resistance are not prevalent in Plasmodium falciparum isolated from Ugandan children. PLoS One.
2014;
9
:
e105690
.
-
Olasehinde
G. I.,
Ojurongbe
D. O.,
Akinjogunla
O. J.,
Egwari
L. O.,
Adeyeba
A. O..
Prevalence of malaria and predisposing factors to antimalarial drug resistance in southwestern Nigeria. Research Journal of Parasitology.
2015;
10
:
92-101
.
-
Muhammad
R. H.,
Nock
I. H.,
Ndams
I. S.,
George
J. B.,
Deeni
Y..
Distribution of pfmdr1 and pfcrt chloroquine drug resistance alleles in north-western Nigeria. MalariaWorld Journal.
2017;
8
:
15
.
-
Oladipo
O. O.,
Wellington
O. A.,
Sutherland
C. J..
Persistence of chloroquine-resistant haplotypes of Plasmodium falciparum in children with uncomplicated Malaria in Lagos, Nigeria, four years after change of chloroquine as first-line antimalarial medicine. Diagnostic Pathology.
2015;
10
:
41
.
-
Gbotosho
G. O.,
Sowunmi
A.,
Happi
C. T.,
Okuboyejo
T. M..
Therapeutic efficacies of artemisinin-based combination therapies in Nigerian children with uncomplicated falciparum malaria during five years of adoption as first-line treatments. The American Journal of Tropical Medicine and Hygiene.
2011;
84
:
936-43
.
-
Oguche
S.,
Okafor
H. U.,
Watila
I.,
Meremikwu
M.,
Agomo
P.,
Ogala
W..
Efficacy of artemisinin-based combination treatments of uncomplicated falciparum malaria in under-five-year-old Nigerian children. The American Journal of Tropical Medicine and Hygiene.
2014;
91
:
925-35
.
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 9 (2018)
Page No.: 2651-2657
Published on: 2018-09-24
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 6959 times
- Download PDF downloaded - 2380 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress







