
Comparison of brain CT angiography/venography and temporal bone HRCT scan findings in patients with subjective pulsatile tinnitus in affected side and unaffected side
- Assistant Professor of otorhinolaryngology, ENT and Head & Neck Research center and Department, Hazrat Rasoul Akram Hospital, Iran University of Medical Sciences (IUMS), Tehran, Iran
- Professor of Otorhinolaryngology, Skull base research center, Iran University of Medical Sciences, Tehran, Iran
- Professor of Otorhinolaryngology, ENT and Head & Neck Research center and Department, Hazrat Rasoul Akram Hospital, Iran University of Medical Sciences (IUMS), Tehran, Iran
- Associate Professor of Otorhinolaryngology, Skull base research center, Iran University of Medical Sciences, Tehran, Iran
- Resident of Otorhinolaryngology, ENT and Head & Neck Research center and Department, Hazrat Rasoul Akram Hospital, Iran University of Medical Sciences (IUMS), Tehran, Iran
Abstract
Introduction: Pulsatile tinnitus (PT) is a discrete repetitive sound that is synchronous with the patient’s pulse. Incidence of abnormal, often treatable and structural findings in patients with PT has been noted to be high, ranging from 44% to 91%. So, accurate diagnosis of pathologic causes is important for treatment and prognosis.
Objective: The main objective of our study was evaluation of abnormal findings in temporal bone HRCT scan and CTA/CTV in patients affected by pulsatile tinnitus, and comparing these findings with unaffected ear of the same individuals.
Methods: A case-control study was conducted and all the patients who had subjective pulsatile tinnitus with normal physical examinations among outpatient individuals referred to our institution; Rasoul Akram Hospital from September 2015 to august 2017 was included in this study. All patients underwent brain CT Angiography/Venography (CTA/V) and temporal bone high resolution CT scan (HRCT), and their findings were compared.
Results: Thirty patients consist of 20 females and 10 males with mean age of 50.83 years were evaluated in this study. Pulsatile tinnitus was unilateral in all patients except one. Comparing results of CTA/V and temporal HRCT scan in the affected ear showed that temporal HRCT scan in 19(63.3%) out of 30 patients reported normal, while CTA/V only in eight (26.6%) of these patients reported normally. So, capability of CTA/V is statistically significant in diagnosis of abnormalities in the affected ear (P=0.012).
Conclusion: Our findings demonstrate that CTA/V can be a more accurate imaging tool than temporal bone HRCT in initial assessment of patients with subjective pulsatile tinnitus and normal physical examination, and should be done as the first imaging tool in these patients.
Abstract
Introduction: Pulsatile tinnitus (PT) is a discrete repetitive sound that is synchronous with the patient’s pulse. Incidence of abnormal, often treatable and structural findings in patients with PT has been noted to be high, ranging from 44% to 91%. So, accurate diagnosis of pathologic causes is important for treatment and prognosis. Objective: The main objective of our study was evaluation of abnormal findings in temporal bone HRCT scan and CTA/CTV in patients affected by pulsatile tinnitus, and comparing these findings with unaffected ear of the same individuals. Methods: A case-control study was conducted and all the patients who had subjective pulsatile tinnitus with normal physical examinations among outpatient individuals referred to our institution; Rasoul Akram Hospital from September 2015 to august 2017 was included in this study. All patients underwent brain CT Angiography/Venography (CTA/V) and temporal bone high resolution CT scan (HRCT), and their findings were compared. Results: Thirty patients consist of 20 females and 10 males with mean age of 50.83 years were evaluated in this study. Pulsatile tinnitus was unilateral in all patients except one. Comparing results of CTA/V and temporal HRCT scan in the affected ear showed that temporal HRCT scan in 19(63.3%) out of 30 patients reported normal, while CTA/V only in eight (26.6%) of these patients reported normally. So, capability of CTA/V is statistically significant in diagnosis of abnormalities in the affected ear (P=0.012). Conclusion: Our findings demonstrate that CTA/V can be a more accurate imaging tool than temporal bone HRCT in initial assessment of patients with subjective pulsatile tinnitus and normal physical examination, and should be done as the first imaging tool in these patients.
Background
Tinnitus is the conscious, unwanted perception of sound that arises involuntarily source of sound 1. It is an annoying symptom that affects about 10% of the population. In more than 60% of patients, even an extensive workup may not lead to diagnosis. The imaging protocol study should therefore be adapted to the history of the patient, and each imaging study should underline which etiologies it may exclude 2. It is most prevalent between 40 and 70 years of age, has a roughly equal prevalence in men and women and can occur to children 3.
Tinnitus may be classified as subjective versus the objective and pulsatile versus continuous. Pulsatile tinnitus is a discrete repetitive sound that is synchronous with the patient’s pulse 4.
Pulsatile tinnitus (PT) is a relatively rare cause of tinnitus. It makes up about 4% of patients with tinnitus. Incidence of abnormal, often treatable, structural findings in patients with PT has been noted to be high, ranging from 44% to 91% 5. In about 70% of these cases, an underlying cause can be identified by adequate diagnostic work-up 6.
The most important differential diagnosis in the patients with subjective PT that categorized by Mattox and Hudgins in 2008, were consisted of middle ear, neoplastic, arterial and venous diseases.
Vascular abnormalities were the most common radiological findings in these patients 7.
There is a general consensus that a contrast-enhanced high-resolution CT of the temporal bone should be the initial imaging study for pulsatile tinnitus 8910. CTA/CTV appears to be a promising initial imaging in most cases of PT 11.
The main objective of our study was evaluation of abnormal findings in temporal bone HRCT scan and CTA/CTV in patients affected by pulsatile tinnitus, and comparing these findings with unaffected ear of the same individuals. Some alternative goals are investigating the incidence of abnormal findings in a Temporal HRCT scan and CTA/CTV separately in both ears and also comparing ability of temporal HRCT and CTA/CTV in diagnosis of these abnormalities.
We believe that CTA/CTV can diagnose pulsatile tinnitus causes more accurately than temporal HRCT scan and furthermore not having risks of four vessels Angiography.
Methods
The study was approved by our institutional review board (Iran University of Medical Science ethical committee, Ethical code: IR.IUMS.FMD.REC 1396.9311369001). Through a prospective investigation, all the patients who had subjective pulsatile tinnitus with normal physical examination among outpatient individuals referred to our institution; Rasoul Akram Hospital, otology and head and neck department from September 2015 to august 2017 was included in this study.
All patients received a careful history taking and neurotologic examinations, Audiogram and radiological studies as indicated. The physical examination included otomicroscopic examination of the ear, auscultation of the neck and periauricular areas and determination if changes occurred in the sound based on head position and neck turning. Patients who had objective pulsatile tinnitus, abnormal physical examination and history of head trauma were excluded from this study. Informed consent obtained from the patients or legal representative for the use of imaging tools.
A case-control study was conducted, and a study group consists of ear side which is affected with subjective pulsatile tinnitus, and a control group consists of sides without pulsatile tinnitus was designed. All patients underwent brain CT Angiography/Venography (CTA/V) and temporal bone high resolution CT scan (HRCT) and Imaging findings included temporal HRCT scan and CTA/CTV of affected ears (study group) and unaffected ears (control group) in each temporal HRCT scan and CTA/CTV evaluated separately and compared.
Temporal bone HRCT/CTA/CTV was performed with a 64-section multidetector CT scanner (Brilliance 64, Philips Medical Systems, Cleveland, Ohio) with 350 mA and 120 kV. Axial reconstructed section thickness was 1.25 mm with a 0.625 mm Section interval. For CTA/V, this was performed from the vertex to approximately the C6 level. All images were reconstructed using standard bone reconstruction algorithms.
Statistical analysis
Statistical analysis was performed using SPSS 23 software. The statistical assessment of differences between groups was performed using the chi-square test. A-value < 0.05 was considered statistically significant.
Results
Thirty patients consist of 20 females and 10 males comprised our study population. The average age was 50.83 ± 11.26 years (Median=51.5). Women average age was 0.30 ± 10.42 and men average age was 51.9 ±13.32 which was not statistically significant. The tinnitus was right-sided in 14 (46.7%); 15(50%) complained of left-sided PT, and one (3.3%) had bilateral PT. Only two patients had vertigo. Physical examination was normal in all 30 patients. Hearing level was normal in 14 patients (46.7%) and mild SNHL in 14 (46.7%) and moderate SNHL in two (6.7%) was observed.
Temporal HRCT scan findings in affected ear are showing as frequency and relative frequency
| Variables | Frequency | Relative frequency |
| Normal | 19 | 63.3% |
| High jugular bulb | 4 | 13.3% |
| Glomus tumor | 4 | 13.3% |
| High jugular bulb + dehiscent jugular bulb | 2 | 6.7% |
| Bilateral high jugular bulb+ dehiscent jugular bulb | 1 | 3.3% |
| Total | 30 | 100% |
Temporal HRCT findings in side of the affected ear were normal in 19 patients (63.3%) and in four patients (13.3%) high Jugular bulb, in four patients (13.3%) Glomus tumor, in two (6.7%) High Jugular bulb and dehiscent Jugular bulb coincide, and in one (3.3%) Bilateral high jugular bulb and dehiscent jugular bulb has been detected. In the other hand 7 patients had high Jugular bulband3 had a dehiscent Jugular bulb. These findings are showing in
CTA/V findings in affected ear showing as frequency and relative frequency
| CTA/V findings | Frequency | Relative frequency |
| Normal | 8 | 26.7% |
| Arterial Stenosis | 2 | 6.7% |
| Anatomical Abnormality of Arteries | 5 | 16.7% |
| Anatomical Abnormality of Veins | 1 | 3.3% |
| Carotid body tumor | 1 | 3.3% |
| Glomus tumor | 5 | 16.7% |
| High jugular bulb | 1 | 3.3% |
| Venous stenosis | 1 | 3.3% |
| High jugular bulb+ dehiscent jugular bulb | 2 | 6.7% |
| High jugular bulb+ dehiscent jugular bulb + DAVF | 1 | 3.3% |
| ICHTN+ High jugular bulb | 1 | 3.3% |
| Anatomical Abnormalities of veins+ High jugular bulb | 2 | 6.7% |
Temporal HRCT scan in unaffected ear was normal in 29 patients (96.7%) and only one patient (3.3%) had High jugular bulb and dehiscent jugular bulb.
Findings of CTA/V in affected ear were summarized in
Comparing results of CTA/V and temporal HRCT scan in unaffected ear revealed that temporal HRCT scan in 29 (96.7%) out of 30 patients reported normally, while CTA/V in 24 (80%) of these patients were normal, which was statistically significant (P=0.042) (
Comparing CTA/V and Temporal HRCT Scan findings in unaffected ear
| CT Angiography report | Temporal HRCT | P value | |
| Normal | High jugular bulb+ jugular bulb dehiscence | ||
| Normal | 24 | 0 | 0.042 |
| ICHTN | 1 | 0 | |
| Anatomical Abnormalities of arteries | 3 | 0 | |
| Anatomical Abnormalities of venous | 1 | 0 | |
| High jugular bulb+ dehiscent jugular bulb | 0 | 1 |
Comparing results of CTA/V and temporal HRCT scan in the affected ear showed that temporal HRCT scan in 19 (63.3%) out of 30 patients reported normal while CTA/V only in eight (26.6%) of these patients reported normally. So, capability of CTA/V is statistically significant (P=0.012) in diagnosis of abnormalities in affected ears (
Comparing CTA/V and Temporal HRCT Scan findings in affected ear
| Report CT-Angiography | Temporal HRCT scan | P Value | ||||
| Normal | Bilateral high jugular bulb+ dehiscent jugular bulb | High Jugular bulb+ dehiscent Jugular bulb | Glomus tumor | High Jugular bulb | ||
| Normal | 8 | 0 | 0 | 0 | 0 | 0.012 |
| Arterial Stenosis | 2 | 0 | 0 | 0 | 0 | |
| Anatomical Abnormalities of arteries | 5 | 0 | 0 | 0 | 0 | |
| Anatomical Abnormalities of venous | 1 | 0 | 0 | 0 | 0 | |
| Carotid body tumor | 1 | 0 | 0 | 0 | 0 | |
| Glomus tumor | 1 | 0 | 0 | 4 | 0 | |
| High jugular bulb | 0 | 0 | 0 | 0 | 1 | |
| Venous Stenosis | 1 | 0 | 0 | 0 | 0 | |
| High jugular bulb+ dehiscent jugular bulb | 0 | 0 | 2 | 0 | 0 | |
| High jugular bulb+ dehiscent jugular bulb + DAVF | 0 | 1 | 0 | 0 | 0 | |
| ICHTN+ High jugular bulb | 0 | 0 | 0 | 0 | 1 | |
| Anatomical Abnormalities of venous+ High jugular bulb | 0 | 0 | 0 | 0 | 2 |
Temporal HRCT scan findings in affected and unaffected sides of patients also compared and showed that in unaffected side, 29 ears (96.7%) were normal while in affected side, 19 ears (63.3%) reported normal which was statistically significant (p<0.001) (
Evaluating some other variables such as side, sex, age, underlying disease, hearing level and vertigo showed no statistically significant difference.
Comparing temporal HRCT Scan findings in affected ear and unaffected ear
| Temporal HRCT scan report in affected ear | Temporal HRCT scan report in unaffected ear | P Value | |
| High jugular bulb+ dehiscent jugular bulb | Normal | ||
| Normal | 0 | 19 | <0.001 |
| High Jugular bulb | 0 | 4 | |
| Glomus tumor | 0 | 4 | |
| High Jugular bulb+ dehiscent Jugular bulb | 0 | 2 | |
| Bilateral high jugular bulb+ dehiscent jugular bulb | 1 | 0 |

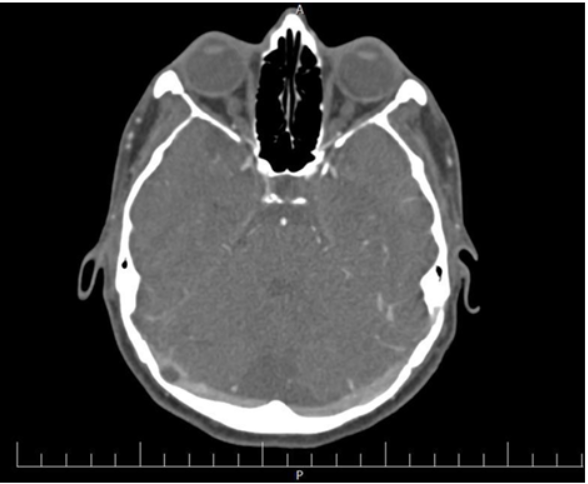
High jugular bulb and jugular bulb dehiscency in left side. (Bone algorithm reconstruction from CTA).

The figures show a left frontal dural AVF in CTA.
Discussion
Pulsatile tinnitus can be vascular and nonvascular in the origin. Most sources are vascular and have a long differential diagnosis. They include 1) high-riding jugular bulb, 2) dehiscent jugular bulb, 3) transverse sinus stenosis, 4) vertebral artery hypoplasia, 5) atherosclerotic carotid artery disease, 6) arteriovenous fistulas Figure 2, 7) arachnoid granulations (Figure 5), 8) glomus tumor, 9) deep cervical artery, 10) laterally placed sigmoid sinus, 11) benign intracranial hypertension and 12) vein abnormalities.

The figure showed right VAH in CTA.
The identification of the source is often difficult and requires a staged set of diagnostic tests. There is some disagreement regarding the primary imaging modality used for the patient with PT. Most observers recommend temporal bone HRCT as the first examination of choice for individuals with a visible mass behind the tympanic membrane 12. In the evaluating arterial subjective PT, the most widely performed tests are MRI/MRA, CTA or a four-vessel angiogram. Both MRI/MRA and CTA are useful in evaluating PT; however, MRI/MRA is limited by poor bony resolution, flow, and artifacts related to air-fat interface.

The figure showed the left deep cervical artery anomaly in CTA.
The figure showed Arachnoid granulations of right transverse sinus in CTA.
Sismanis revealed it is felt that the initial test in these cases should begin with a CTA. Due to cost and risks of complications, a four-vessel angiogram should not be used in most cases 7. CTA/V could serve as that single examination by providing high-resolution images of the temporal bones to evaluate for a middle ear lesion, an arterial phase to evaluate for carotid bifurcation or ICA pathology, and a venous phase to evaluate the size, patency and integrity of the major venous sinuses and internal jugular veins 13.
In the study was performed by Narvid and coworkers in 2011, CT Angiography as a screening tool for dural arteriovenous fistula in patients with pulsatile tinnitus was evaluated and they suggested that the combined signs of abnormally prominent arterial feeders, shaggy sinus/tentorium, and asymmetric jugular venous attenuation produce useful diagnostic information with a combined sensitivity and specificity 90% 11.
Stenosis, strictures, and segmentation of the transverse sinus are also associated with pulsatile tinnitus 14. This finding was best appreciated on both axial and coronal CTA/V reformations through the posterior fossa venous sinus system 13.
Temporal bone HRCT can demonstrate the detailed anatomy and pathology of the temporal bone and is a fast becoming modality in the diagnosis. It can provide information which will help surgeons in the management of their patients. These conditions are middle ear inflammation, cholesteatoma, temporal bone trauma, external auditory canal atresia and vascular tympanic membrane. In 2008, Mattox . proposed an algorithm for evaluation of pulsatile tinnitus. They suggested temporal bone HRCT in the patients with vascular tinnitus and autophonia without audible breathing that can show dehiscent semicircular canal 6.
Atypical formations of the jugular bulb favor the development of venous tinnitus. There are huge variations between individuals, and these are common, asymptomatic and incidental findings 1516. A HRCT scan is diagnostic and should be examined specifically for these lesions 17.
Sonmez reviewed 74 patients with pulsatile tinnitus who evaluated radiologically with HRCT, CTA, MRA or DSA overall. They found underlying pathology in 50 patients (67.6%) and 24 patients were normal. The most common cause was high jugular bulbs 15.
In our study, Temporal HRCT findings in side of the affected ear were normal in 19 (63.3%) out of 30 patients but CTA/V findings were normal only in eight (26.7%) patients. It revealed that CTA/V can be a more accurate imaging tool than temporal bone HRCT in diagnosis of underlying pathology in these patients.Although our study evaluated fewer patients than previous study, but all patients underwent both HRCT and CTA/V separately. The most common causes detected in temporal bone HRCT were glomus tumor and high jugular bulb (Figure 1) and the most common causes in CTA/V were glomus tumor and anatomical abnormality of the arteries (Figure 3Figure 4). Based on our findings, glomus tumor was most common cause in both HRCT and CTA/V.
Also in our study, temporal bone HRCT findings in unaffected ear were normal in 29 patients (96.7%), while Findings of CTA/V in unaffected ear were Normal in 24 patients (80%). Therefore, the advantage of CTA/V is that it can demonstrate the underlying pathology in the side of unaffected ear.
Also CTA/V can demonstrate arterial and venous anatomy of the neck and intracranial circulation, but also renders excellent views of the temporal bone. Multidetector CTA or CTV of the head and neck region can be performed for the evaluation of vascular pathology. Bone window images of the skull and temporal bone can be reconstructed from a multi-detector CTA or CTV acquisition, obviating the need for a separate acquisition, which reduces radiation exposure 18.
Limitations of our study were few numbers of the patients and also patients with negative results in CTA/V didn’t evaluate with DSA. Further studies are needed to compare the results of CTA/V with DSA to evaluate false negative results of CTA/V.
Conclusions
Pulsatile tinnitus may cause significant morbidity, and recognition of its pathologic causes is important for the treatment. Our study demonstrates that CTA/V can be a more accurate imaging tool than temporal bone HRCT in initial assessment of patients with subjective pulsatile tinnitus and normal physical examinations. CTA/V can discover bone lesions in bone reconstructed images and also can evaluate vascular abnormalities with high-accuracy measurement while it is not accompanying morbidities of conventional 4 vessels Angiography. But conventional 4 vessels angiography is still indicated if CTA is negative but clinical suspicion of DAVF or other vascular lesions is high.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License (CCBY4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
List of abbreviations
ACAD: Atherosclerotic carotid artery disease; AVF: Arteriovenous fistula; CTA/V: Computed Tomography Angiography/ Venography; HRCT : High Resolution Computed tomography; PT: Pulsatile Tinnitus; SNHL : Sensory Neural Hearing Loss; VAH: Vertebral artery hypoplasia; VP: Vagal Paraganglioma
Ethics approval and consent to participate
The study was approved by our institutional review board (Iran University of Medical Science ethical committee, Ethical code: IR.IUMS.FMD.REC 1396.9311369001).
Competing interests
All authors declare that they have no significant competing financial, professional, or personal interests that might have influenced the performance or presentation of the work described in this manuscript.
Authors' contributions
Sara Rostami: Literature search, Design, Clinical studies, Data acquisition, Manuscript preparation, corresponder. Mohammad Mohseni: Concepts, Design, Definition of intellectual content, Clinical studies, Manuscript editing. Maryam Jalessi: Design, Concepts, Manuscript editing. Ahmad Daneshi: Clinical studies, Concepts, Manuscript review. Alimohamad Asghari: Concepts, Design, Clinical studies, Manuscript editing. Yasser Nasoori: Data analysis, Manuscript review. All authors read and approved the final manuscript.

