Abstract
Purpose of the study: To understand surgical outcomes, based on standardized tools, after surgery of lumbar spinal canal stenosis in patients aged 65 years and older.
Methods: A cross-sectional study was undertaken in 58 elderly patients before and after surgery. Demographic data, procedures, perioperative comorbidities, preoperative and postoperative pain intensity, primary activities of daily living, quality of life, and fear avoidance were collected at baseline. All patients were followed up to 6 and 12 months after operation.
Results: Following surgery, there was a significant reduction in the VAS scale (for pain severity) and fear avoidance beliefs (FAB) questionnaire scale (P<0.001), and a significant increase in the 36-Item Short Form Health Survey (SF-36) index and the Barthel Index for Activities of Daily Living (ADL), which assesses functional independence) (P<0.001).
Implication: The present study suggests that surgery in elderly patients is effective for the treatment of spinal stenosis, in those patients who did not respond well to conservative treatment.
Background
Improving quality and duration of life, particularly in the elderly population, are among the great achievements of the current century. To date, as more people age and become elders, this has prompted a rapid change in the demographics and raised important concerns regarding health care in the elderly [1]. According to the World Health Organization (WHO), between 2015 to 2050, the number of people, ages 60 years and older, is expected to rise from 900 million to 2 billion [2]. Aging is a physiological process that is also inevitable [3]. As the elderly age, they experience a variety of age-related diseases, such as degenerative diseases of the spine. With age, degenerative changes in the lumbar spine are commonly seen in magnetic resonance imaging (MRI) evaluations. Indeed, lumbar spinal defects can be found in 100% of people over the age of 60 [4].
The most common degenerative disease in the elderly (65 years and older) is spinal canal stenosis, which ultimately leads to surgery [1][5][6]. The patients often experience pain, intermittent claudication, physical disability, numbness and weakness of the legs, poorly functioning cramps, inability to perform daily activities, and psychological factors (e.g. depression, anxiety, insomnia, and social isolation). These factors negatively impact patient quality of life. This can lead to an increase in the use of health services. Moreover, worsening of the spinal condition of the patient can occur due to other diseases associated with aging [1][7][8]. According to Iran’s national census of 2016, individuals over 65 years of age constituted about 6.09% of the total population in Iran and over 8.4% of the population in Tehran. In early 2017, about 8.2% of Iran’s population was reported to be 65 years of age and above [9].
Based on the results of studies in other countries, surgery is a safe and effective method for treating spinal canal stenosis, in those who do not respond to cure. Most patients benefit from reducing pain and improving daily function, which lead to greater satisfaction and outcome after surgery [1]. Indeed, the number of spinal surgeries has increased by 105%, between 2005 and 2010, and reportedly increased by 162% for people over the age of 65 [4]. Bati et al. (2012) conducted a study to estimate the burden of disease due to spinal canal stenosis on the quality of life associated with health and its underlying illnesses [10]. There were 7,489 adult patients representing the population, and 245 cases representing spinal canal stenosis. The results showed that the prevalence of arthritis, migraine, hypertension, and urinary incontinence was higher in the group with spinal canal stenosis than in the community representative group. As well, the negative effects of spinal canal stenosis on the quality of life associated with health was equal to or greater than that for conditions, such as diabetes, heart disease, arthritis, and even stroke [10]. The results of the study by Lozano-Alvarez et al. (2014) aimed to investigate the epidemiological factors for the outcome of degenerative spinal stenosis surgery in 263 patients, before and two years after surgery. They showed that there was a significant relationship between age, sex, attenuation, pain, and quality of life in physical and mental dimensions [11].
Regarding the aging process of the Iranian population, thus far, no studies have been conducted in this research area. The aim of the study herein is to investigate the effect of degenerative stenosis on quality of life, pain, avoidance beliefs (due to fear), and daily activities of the elderly.
Methods
This research is a cross-sectional study, consisting of 58 patients (ages 65 years or older) with spinal degenerative stenosis. They were candidates for surgery, who had been referred to the Central Hospital, and selected for trial by convenience sampling method. Inclusion criteria included: patients 65 years of age and older, presence of symptomatic spinal canal stenosis, radiological confirmatory imaging, and failed conservative treatments. Exclusion criteria were: spinal canal stenosis (due to other causes), infection, acute or old vertebral fractures, metastasis and inflammatory diseases, degenerative or isthmic spondylolisthesis, degenerative scoliosis, and/or revision surgery. This study was approved by the Ethics Committee of Tehran University of Medical Sciences, with the code IR.TUMS.REC. 1395.2254. If the patients met the criteria for entry, they were informed of the study purpose, methods, and the patient questionnaires to be completed. All patients submitted informed written consents before the study began.
The questionnaires were presented during interviews, given 6 and 12 months after surgery, by the study researchers. The first part of the questionnaire included information about demographics, including age, sex, education, occupation, and history of underlying diseases. The second part of the questionnaire included the 36-Item Short Form Health Survey (SF-36), Visual Analog Scale (VAS; measures pain), the Barthel Index for Activities of Daily Living (ADL; assesses functional independence), and a Fear-Avoidance Beliefs (FAB) questionnaire.
In the SF-36 standard questionnaire, 36 questions of physical and mental health are addressed based on the following eight components: physical activity, physical pain, physical role, general understanding of general health, force or vital force, social activity, emotional role, and mental health. The Likert scale ranges from 0 to 100 for scoring; zero represents the lowest level of quality of life, and 100 represents the maximum (highest) level of quality of life [12].
The Barthel ADL Index is a scale that measures performance in daily life activities. The ten activities include eating/feeding, disposing of stool (presence of absence of fecal incontinence), urination (presence or absence of urinary incontinence), using the toilet, dressing, grooming (shaving, brushing teeth and hair, etc.), transferring from bed to chair, walking, climbing stairs, and washing/bathing. A score from 95-100 means non-dependence, from 15-69means mild dependence, and 0-14 means complete dependence. Each of these components has its scoring point; a total is calculated up to 100. Lower scores indicate increased disability in the daily life activities. The reliability of this index, as estimated by Kazemi et al., is approximately 0.827 [13].
The FAB questionnaire is used to evaluate the attitude and belief avoidance for work, based on fear of pain. The questionnaire addresses avoidance of attitudes and beliefs about physical activity (scoring from 0 to 24), as well as seven components which examine the avoidance of work-related attitudes and beliefs (scored from 0 to 42). Each item is scored based on the Likert range (from “agree” to “disagree”). A score of over 14 indicates a high degree of avoidance [14]. This standard questionnaire has been translated into Persian by Hedayati et al. [15]. In this study, fear and the avoidance of work were not calculated because since the patients were elderly, most were retired from work or were housewives [16].
The VAS is a standard tool for assessing the severity of pain in patients. The score ranges from 1 (lowest severity) to 10 (highest severity); scoring is based on the patient’s statement. It is worth noting that all patients complied with the protocol of routine housing.
Data were analyzed by SPSS software (version 16), descriptive statistical methods (frequency, percentage, and mean), and analysis of paired T-tests and Pearson’s coefficient.
Results
From March 20, 2016 to March 19, 2017, 58 eligible patients participated in the study. Of the 58 patients in the study, 77.6% were female, and 22.2% were male. 82.8% of the patients were undergoing laminectomy, 13.8% had discectomy, and 3.4% had both. Patient demographic data are presented in Table 1 .
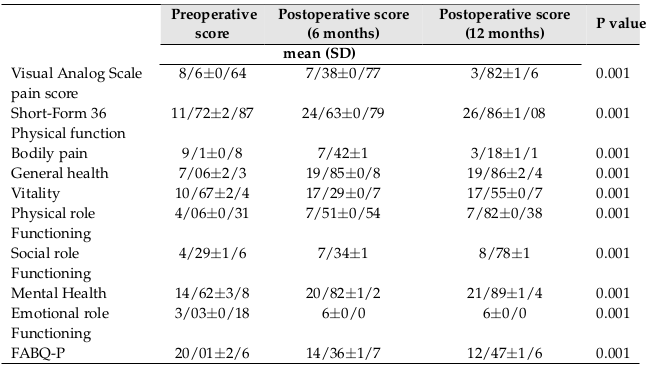
The results showed that the daily activity of patients improved significantly (P <0.001) 3 at 6 months after surgery, as compared with the preoperative assessment (P <0.001). The Barthel score increased from 70.1 ± 9.3 before surgery, to 77.4 ± 4.5 at 6 months after surgery, and 83.3 ± 2.3 at 12 months after surgery. The VAS scale (pain relief) also improved as did the SF-36 survey on quality of life. In the case of fear-avoidance beliefs (avoidance of physical activity), a significant change was observed in fear and avoidance of physical activity, before surgery, and at 6 and 12 months after surgery (P <0.001). The results are detailed in Table 2 .
Discussion
Increased life expectancy has increased the demand for surgery in the elderly with spinal canal stenosis [17]. In this study, we evaluated 58 elderly patients with degenerative spinal canal stenosis. The results showed that quality of life, pain, daily physical activity, and avoidance of physical activity, due to fear, improved significantly. It is worth noting that comparison of this study with other studies in Iran is difficult because there has been no previous study of this subject (elderly with spinal canal stenosis) in Iran.
In the study, the quality of life components of the SF-36 survey was evaluated. These components included physical activity, physical pain, physical role, general understanding of general health, vital or vital force, social activity, emotional role, and mental health pre- and post-surgery. After surgery, there was a significant improvement in all components (P <0.001), especially with regards to physical activity and general understanding of general health. Rosen et al. showed in his study that the quality of life of SF36 also improved, especially regarding physical activity in elderly patients [18]. The findings of Sobottke et al. (2017), Dimar et al. (2004), Sasso et
al. (2004), and Glassman et al. (2006) also referred to the improvement of quality of life in elderly
patients with postoperative spinal canal stenosis [17],[19]–[21].
Moreover, the daily life activities of the elderly significantly also improved, according to the Barthel scale after surgery, as assessed from the 6-month and 1-year follow-ups (P <0.001), which is consistent with the study by Sheha et al. (2011). Sheha showed that the daily activity improved from 42.2 (before surgery) to 94.4 (after surgery) [22]. Shabet et al. (2008) and Gepstein et al. (2006) showed similar results in their studies [1].
In spite of drug treatments, patients with spinal stenosis may still suffer from pain, which leads to physical limitations as they are not able to adapt to the constraints associated with the pain. Therefore, surgery is a suitable option for some [23]. The results from our s study indicate that the postoperative pain in the spinal canal stenosis in the elderly decreased significantly (P < 0.001) after surgery. Our results are consistent with the results of Antoniadis et al. (2017), who showed that after spinal canal stenosis surgery on 159 elderly patients (ages 80 years and older), the VAS scale decreased from 7.2 (before surgery) to 4.5 (after surgery) [24]. Additionally, Rosen et al. (2007) showed pain reduction after surgery, from 5.7 to 2.2 [18]. Ahmad Fathi Shaha also studied the pain level using the VAS scale, before and after lumbar spinal stenosis surgery; they concluded that the mean pain intensity decreased from 8.1 to 1.3 after surgery [22].
Regarding fear-avoidance beliefs, the results of our study showed that in comparing before and after surgery, there was a significant decrease in avoidable beliefs post-surgery (P <0.001). This is significant because patients with low back pain often interpret activities that can lead to chronic pain as a negative factor or stimulus, which in turn provokes fear and refusal to perform such activities [25]. Thus, a decrease in fear-avoidance beliefs has positive ramifications for the patient.
However, the results of our study are not consistent with the study by Burgstaller et al. (2017), which showed that improvement in fear avoidance of patients in the first phase were not observed at 6 and 12 months follow-up. This could be due to cultural, social, and other causes in the elderly in Iran (such as their families and their willingness to have autonomy). A study by Havakeshian et al. (2013) found that 159 patients with SCI who underwent surgery showed fear of physical activity after surgery. The practice declined significantly, which is consistent with our study [26]. From the study herein, it can be concluded that there is a consensus on reducing pain and improving the quality of life after surgery for spinal canal stenosis patients of all ages, particularly with a focus on the elderly in Iran [16]. It is worth noting that our study is the first in Iran to explore the benefits of surgery in the elderly, who have lumbar spinal stenosis, and the first to evaluate the patients at 6 months and one-year follow-up. The limitations of this study include the relatively small number of patients undergoing surgery, the fact that the study was conducted in a center, and the follow-up period of one year (which is too short). Of course, it should be noted that Central Hospital is one of the largest rehabilitation hospitals in Tehran, which is available for access from all parts of the country; its patients can be reagents. However, it is suggested that subsequent studies be carried out in the form of a multi-center. Also, the study should be conducted with a greater sample size and have multi-year follow-up.
With regard to the aging population of Iran and the results of other studies, our overall conclusion is that surgery in the Iranian elderly bearing spinal canal stenosis is an appropriate therapy or method, for this age group (65 years and above) that did not respond to other therapies. The surgery did not add increased risk to the patients and should lead to reduced pain, improved daily living activities, improved quality of life, and also divert from limited physical activity due to fear.
Conclusion
In conclusion, surgical treatment in elderly patients suffering from lumbar spinal canal stenosis or failed conservative treatments appears to have good outcome. For improved results, a larger randomized control study is suggested.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License (CC-BY 4.0) which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
List of abbreviations
ADL: Activities of Daily Living ; DM: Diabetes Mellitus; FAB: Fear Avoidance Beliefs ; FABQ- P: Fear Avoidance Beliefs Questionnaire- Physical activity ; MRI: Magnetic Resonance Imaging; SCI: Spinal Cord Injury; VAS: Visual Analog Scale; WHO: World Health Organization
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Tehran University of Medical Sciences, with the code IR.TUMS.REC. 1395.2254.
Availability of data and materials
Authors will provide if requested.
Competing interests
All authors have no conflicts of interest.
Funding
This study was funded and supported by Tehran University of Medical Sciences.
Authors’ contributions
Fatemeh Mirbazegh (FM), Babak Mirzashahi (BM), Elham Ghasemi (EG) and Mohammad Aghajani (MA) were responsible for the study’s conception and design. FM and BM helped in the process of sampling, Jayran Zebardast (JZ) performed the data analysis.
References
-
S
Shabat,
Z
Arinzon,
Y
Folman,
J
Leitner,
R
David,
E
Pevzner,
R
Gepstein,
P
Ilya,
I
Shuval.
Long-term outcome of decompressive surgery for lumbar spinal stenosis in octogenarians. European Spine Journal.
2008;
17
:
193-198
.
View Article Google Scholar -
O
WH.
World report on ageing and health: World Health Organization. 2015
.
-
R
Hacihasanog lu,
A
Yildirim,
P
Karakurt.
Loneliness in elderly individuals, level of dependence in activities of daily living (ADL) and influential factors. Archives of Gerontology and Geriatrics.
2012;
54
:
61-66
.
-
R
Kalff,
C
Ewald,
A
Waschke,
L
Gobisch,
C
Hopf.
Degenerative lumbar spinal stenosis in older people: current treatment options. Deutsches Ärzteblatt international.
2013;
110
:
613
.
View Article Google Scholar -
TC
Edwards,
DC
Lavallee,
Z
Bauer,
BA
Comstock,
JG
Jarvik,
DL
Patrick,
UE
Makris,
JL
Friedly.
Problem areas identified as important to older adults with lumbar spinal stenosis. The Spine Journal.
2015;
15
:
1636-1644
.
View Article Google Scholar -
EK
Shin,
CH
Kim,
CK
Chung,
Y
Choi,
D
Yim,
W
Jung,
SB
Park,
JH
Moon,
W
Heo,
SM
Kim.
Sagittal imbalance in patients with lumbar spinal stenosis and outcomes after simple decompression surgery. The Spine Journal.
2017;
17
:
175-182
.
View Article Google Scholar -
Y
Ishimoto,
N
Yoshimura,
S
Muraki,
H
Yamada,
K
Nagata,
H
Hashizume,
N
Takiguchi,
A
Minamide,
H
Oka,
H
Kawaguchi.
Prevalence of symptomatic lumbar spinal stenosis and its association with physical performance in a population-based cohort in Japan: the Wakayama Spine Study. Osteoarthritis and cartilage.
2012;
20
:
1103-1108
.
View Article Google Scholar -
J
Jiang,
H
Wang,
L
Wang,
B
Zhang,
Q
Guo,
W
Yuan,
X
Lu.
Multifidus Degeneration, A New Risk Factor for Lumbar Spinal Stenosis: A Case-Control Study. World neurosurgery.
2017;
99
:
226-231
.
View Article Google Scholar -
MT
Sheykhi.
Aging and the Consequent Alzheimer's Disease in Iran: An Outlook. of.
2017;
6
:
2
.
-
MC
Battié,
CA
Jones,
DP
Schopflocher,
RW
Hu.
Health-related quality of life and comorbidities associated with lumbar spinal stenosis. The Spine Journal.
2012;
12
:
189-195
.
View Article Google Scholar -
C
Lozano-Álvarez,
D
Pérez-Prieto,
G
Saló-Bru,
A
Molina,
A
Lladó,
E
Cáceres,
M
Ramírez.
Can epidemiological factors affect the 2-year outcomes after surgery for degenerative lumbar disease in terms of quality of life, disability and post-surgical pain?. Revista Espa-ola de Cirugía Ortopédica y Traumatología (English Edition).
2014;
58
:
78-84
.
View Article Google Scholar -
N
Zahmatkeshan,
S
Akaberian,
S
Yazdanpanah,
R
Khoramroodi,
T
Gharibi,
al
Jamand T et.
Assessing Quality Of Life and related factors in Bushehr, s elders-1387-8. Journal of Fasa University of Medical Sciences.
2012;
2
:
53-58
.
-
H
Kazemi,
S
Ghasemi,
F
Sharifi,
H
Fakhrzadeh,
M
Ghaderpanahi,
M
Mirarefin,
M
Foroughan.
The relationship between mental state and functional status in elderly residents of Kahrizak. Iranian Journal of Ageing.
2010;
4
:
0-0
.
-
S
Poiraudeau,
F
Rannou,
G
Baron,
AL
Henanff,
E
Coudeyre,
S
Rozenberg,
D
Huas,
C
Martineau,
I
Jolivet-Landreau,
al
Garcia-Mace J et.
Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain.
2006;
124
:
305-311
.
View Article Google Scholar -
al
Kahrizi S et.
Stabilization exercises and their effect on fear-avoidance belief and disability in patients with recurrent nonspecific low back pain. Koomesh.
2015;
17
:
142-151
.
-
JM
Burgstaller,
MM
Wertli,
J
Steurer,
AG
Kessels,
U
Held,
HF
Gramke,
SG
LSOS.
The influence of pre-and postoperative fear avoidance beliefs on postoperative pain and disability in patients with lumbar spinal stenosis: Analysis of the Lumbar Spinal Outcome Study (LSOS) Data. Spine.
2017;
42
:
E425-E432
.
View Article Google Scholar -
R
Sobottke,
C
Herren,
J
Siewe,
AF
Mannion,
C
Röder,
E
Aghayev.
Predictors of improvement in quality of life and pain relief in lumbar spinal stenosis relative to patient age: a study based on the Spine Tango registry. European spine journal.
2017;
26
:
462-472
.
View Article Google Scholar -
DS
Rosen,
JE
O'toole,
KM
Eichholz,
M
Hrubes,
D
Huo,
FA
Sandhu,
RG
Fessler.
Minimally invasive lumbar spinal decompression in the elderly: outcomes of 50 patients aged 75 years and older. Neurosurgery.
2007;
60
:
503-510
.
View Article Google Scholar -
J
Dimar,
S
Glassman,
B
Kenneth,
L
Carreon.
P60. A comparison of prospective clinical outcome measures for anterior vs posterior single-level spine fusion. The Spine Journal.
2004;
4
:
S109-S110
.
View Article Google Scholar -
RC
Sasso,
SH
Kitchel,
EG
Dawson.
A prospective, randomized controlled clinical trial of anterior lumbar interbody fusion using a titanium cylindrical threaded fusion device. Spine.
2004;
29
:
113-121
.
View Article Google Scholar -
S
Glassman,
MF
Gornet,
C
Branch,
D
Polly,
J
Peloza,
JD
Schwender,
L
Carreon.
MOS short form 36 and Oswestry Disability Index outcomes in lumbar fusion: a multicenter experience. The Spine Journal.
2006;
6
:
21-26
.
View Article Google Scholar -
AF
Sheha.
Surgical management of post-discectomy spondylodiscitis with transforaminal lumbar interbody fusion (TLIF) and posterior instrumentation. Life Sci J.
2011;
8
.
-
B
MOBINI,
H
Behtash,
MME
AMERI,
SAR
BASAMPOUR.
PATIENT SATISFACTION AFTER SPINAL DECOMPRESSION IN CENTRAL DEGENERATIVE SPINAL STENOSIS (AN EARLY RESULT). 2006
.
-
A
Antoniadis,
NH
Ulrich,
S
Schmid,
M
Farshad,
K
Min.
Decompression surgery for lumbar spinal canal stenosis in octogenarians; a single center experience of 121 consecutive patients. British journal of neurosurgery.
2017;
31
:
67-71
.
View Article Google Scholar -
I
Sajjadian,
HTN
Dost,
H
Molavi,
RB
Sararoudi.
Cognitive and emotional factors effective on chronic low back pain in women: Explanation the role of fear-avoidance believes, pain catastrophizing and anxiety. J Res Behav Sci.
2011;
9
:
79-90
.
-
S
Havakeshian,
AF
Mannion.
Negative beliefs and psychological disturbance in spine surgery patients: a cause or consequence of a poor treatment outcome?. European Spine Journal.
2013;
22
:
2827-2835
.
View Article Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 5 No 5 (2018)
Page No.: 2279-2286
Published on: 2018-05-19
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 11997 times
- Download PDF downloaded - 2266 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress