Abstract
Introduction: Newborns have a limited amount of antioxidant protection. Exchange transfusion may affect Prooxidant-Antioxidant Balance (PAB). The present study is conducted to investigate the effect of the exchange transfusion on PAB in newborn jaundice.
Methods: The present study is based on a clinical trial which is conducted at Ghaem Hospital in Mashhad, Iran during 2015-2016 that involved sampling on 22 jaundiced newborns (high bilirubin of 17 mg/dL) over a course of 35 weeks. Data collection for the study questionnaire included maternal blood group, neonatal characteristics (age, sex, weight, gestational age, Apgar score, etc.), and laboratory assessment (bilirubin, hematocrit, direct and indirect Coombs testing, reticulocytes, Glucose-6-phosphate dehydrogenase (G6PD), thyroxine (T4), thyroid stimulating hormone (TSH), and PAB). The amount of PAB and serum total bilirubin (STB) of newborns before, after and 6 hours after the exchange transfusion were investigated. Data analysis was performed via statistical tests (paired t-test) using SPSS version 19.
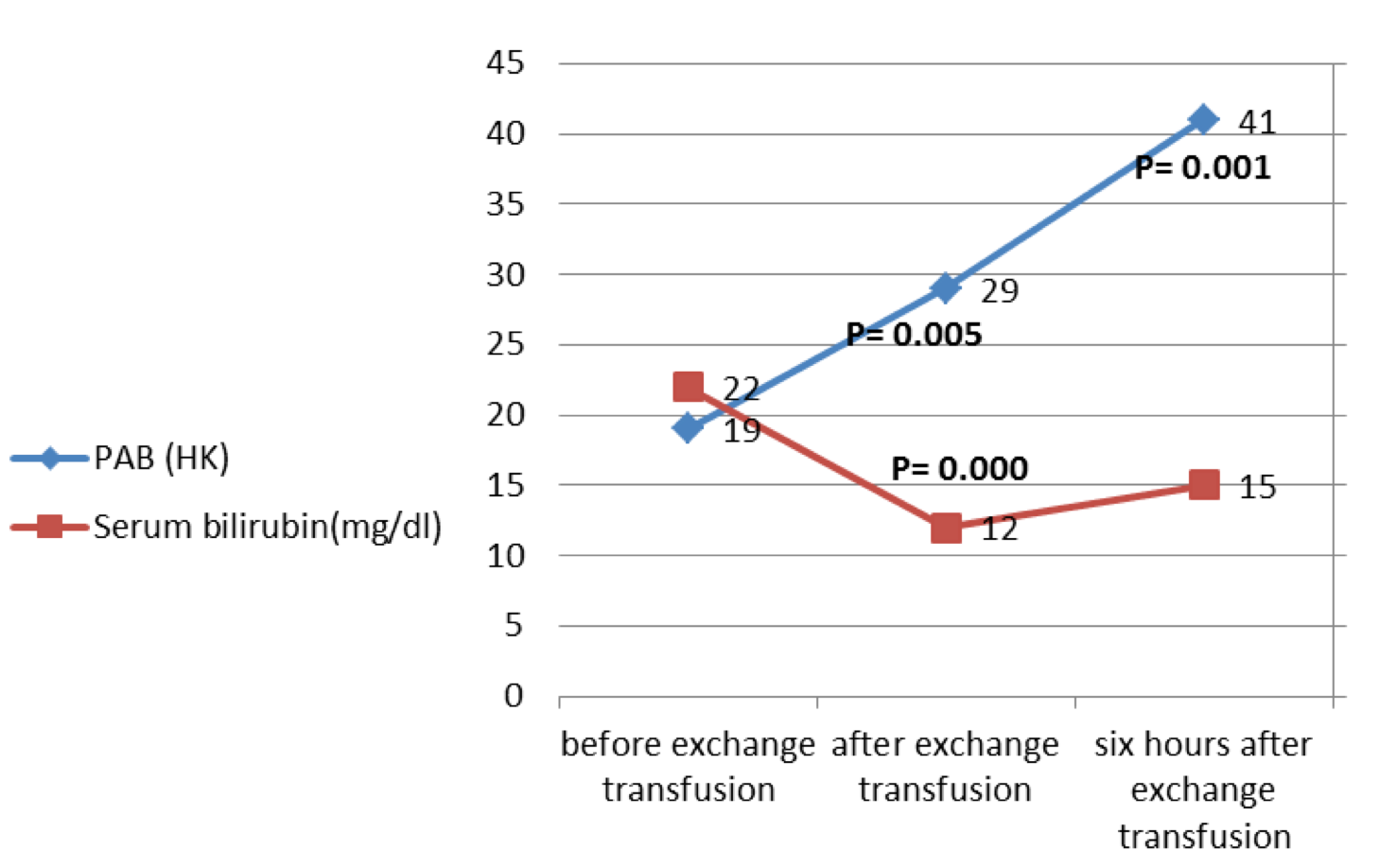
Results: The average bilirubin before the exchange transfusion was 22.02±5.80 mg/dL, after the exchange transfusion was 11.56±3.95 mg/dL, and at 6 hours after the exchange transfusion was 14.99±4.20 mg/dL. The average PAB before the exchange transfusion was 19.06±11.91 HK units, after the exchange transfusion was 29.40±17.70 HK, and at 6 hours after the exchange transfusion was 40.82±18.79 HK.
Conclusion: The results of the study show that the Prooxidant-Antioxidant balance in the exchange transfusion changes in favor of prooxidants and also intensifies even up to 6 hours after the exchange transfusion.
Introduction
Hyperbilirubinemia is observed in about two-thirds of newborns; most cases are benign and gradually improve, but about 8-11% of newborns have bilirubin that progresses over 95% and require evaluation and treatment Boskabadi et al., 2011. The appropriate diagnosis, treatment and follow-up of jaundice have always been important challenges in neonatology. Currently, the most common treatment for neonatal jaundice is phototherapy Bhutani et al., 2013. However, in the event that phototherapy is not successful, the next and final step for jaundice control is the exchange transfusion.
The exchange transfusion may affect the Prooxidant-Antioxidant Balance (PAB) in newborns. Indeed, newborns have a limited amount of protective antioxidants and oxidative damage plays an important role in the pathogenesis of many diseases Boskabadi et al., 2014Boskabadi et al., 2016Perrone et al., 2012.
Oxidative stress is the result of an imbalance between the prooxidants and antioxidants Alamdari et al., 2007. Oxidative stress occurs when the production of oxidants or reactive oxygen species (ROS) exceeds the antioxidant capacity. Subsequently, oxidative stress induces a cellular adaptive response that entails the production of antioxidants Boskabadi et al., 2012.
Following oxidative stress, severe damage occurs to the DNA, proteins and fat Golubnitschaja et al., 2011. The antioxidant capacity of jaundiced newborns depends on the serum bilirubin level, which is reduced after the exchange transfusions Turgut et al., 2004. Moreover, the exchange transfusion rapidly results in change of concentrations of peroxide and antioxidants. Therefore, exchange transfusion affects free radical metabolism in newborns Lindeman et al., 1992.
Hirano et al. showed that the conversion of non-bonded iron to transferrin in the blood is increased after the transfusion in premature newborns. In fact, the conversion of non-bonded iron to transferrin may catalyze the production of ROS and may have a role in the incidence of retinopathy of prematurity and chronic lung disease Hirano et al., 2001. Before connecting to the transferrin, the iron should be transformed by ferroxidase to the ferric state Gutteridge and Stocks, 1981.
Despite of the increase of serum iron after the transfusion, a significant change in the level of oxidative stress was not observed in a study by Dani et al. Dani et al., 2001. The results of the study of Gopinathan et al., on the relationship between bilirubin and ascorbate in plasma antioxidant activity in infants, showed that there was a direct relationship between antioxidant activity and plasma bilirubin Gopinathan et al., 1994. According to the studies, it seems that the role of the exchange transfusion is unclear with regards to the PAB. Therefore, the aim of this study was to evaluate the amount of PAB before the exchange transfusion after transfusion, and six hours after.
Materials - Methods
The present study is based on a clinical trial which was conducted in Ghaem Hospital in Mashhad, Iran during 2015-2016, with sampling on 22 newborn jaundice cases over 2 to 14 days with elevated bilirubin levels (>17mg/dL). In this study, the newborns, term and near-term (>35 weeks), were selected with available sampling. This study was approved by the Ethics committee of the Research Deputy, Mashhad University of Medical Sciences; before entering the study, an informed consent was obtained from the parents of all infants. Exclusion criteria for the study included: severe birth defects, birth asphyxia, respiratory distress, sepsis, Rh incompatibility and ABO, a positive direct Coombs test, maternal diabetes, and preeclampsia/eclampsia.
The instrument for data collection was a questionnaire that the study researchers included on maternal blood group, neonatal characteristics (age, sex, weight, gestational age, Apgar score, etc.), and laboratory assessments (bilirubin, hematocrit, direct and indirect Coombs, reticulocytes, Glucose-6-phosphate dehydrogenase (G6PD), thyroxine (T4), thyroid stimulating hormone (TSH), and PAB). The amount of PAB and serum total bilirubin (STB) in newborns before, immediately after, and 6 hours after the exchange transfusion were investigated.
The PAB is determined by Tetra methyl benzidine (TMB) in two different reactions; one is an enzymatic reaction oxidized by peroxide (hydrogen peroxide (H2O2) in this experiment) to the cation TMB, and another is a reaction which the cation is restored by the antioxidants (uric acid in this experiment). For this purpose, 16 mg of TMB powder was dissolved in 10ml of Dimethyl sulfoxide (DMSO) so that the solution of DMSO/TMB could be obtained. Then, to prepare the TMB cation solution, TMB (400 μL) of the above solution was added to 20 mL of sodium acetate buffer (pH=4.5, 0.05 M). Then, 70 μL of the freshly prepared Chloramine T solution (100 mM) was added to 20 mL of this solution, and was mixed well and incubated for 2 h at room temperature in the dark room. In the second phase, 25 U of peroxidase solution was added to 20 mL of TMB cation solution and 1 cc was distributed in micro-tubes and stored at -20°C.
To prepare the solution of TMB, 200 mL was added from the DMSO/TMB solution to 10 ml of sodium acetate buffer (pH=5.8, 0.05 M). Next, 1 ml of TMB cation solution with peroxidase enzyme (soluble step 2) was mixed with 10 mL of TMB solution and incubated for 2 minutes at room temperature in the dark room. Ten mL was aliquoted from each serum sample, including a standard or blank sample (distilled water), and mixed with 200 μL of solution phase 3. The mix was then plated into wells of an ELISA plate and incubated for 12 min at 37°C. The standard solution included the known percentage of H2O2 (250 μM) and uric acid (3 mM) in sodium hydroxide (NaOH; 10mM). After incubation, 100 μL of 2N hydrochloric acid (HCl) was added to the wells. Using an ELISA plate reader set at wavelength of 450 nm, the absorption of each well was read. A standard curve was obtained from the absorption of the standard samples (H2O2 0-100% and uric acid 0-100%); the concentrations of the serum samples could be extrapolated from the standard curve. The PAB values were measured based on the HK conventional unit which reflects the percent of hydrogen peroxide in the standard solution Boskabadi et al., 2014Boskabadi et al., 2016. Unknown values of specimens were calculated based on the values obtained from the standard curve Alamdari et al., 2007.
Statistical analysis
Data analysis was performed by paired t-test using statistical software SPSS (version 19); P≤0.05 was considered statistically significant.
Results
Incidence rate
Among the 22 newborns studied, 12 infants (54.5%) were female and 10 (45.5%) were male. Fourteen cases (59.1%) were born by vaginal delivery and 8 cases (31.8%) were born by Caesarean section.
The average age of the newborns was 6.89±4.04 days. The average weight at birth and weight at admittance of the newborns were 2836±723.13 and 2656±740.63 g, respectively. The average bilirubin levels were 27.14±6.8, 22.02±2.80, 11.56±3.95 and 14.99±4.20 mg/dL, respectively, at admission time, before exchange transfusion, after exchange transfusion (immediately), and 6 hours after exchange transfusion, respectively. The average PAB values were 19.06±11.91, 29.40±17.70 and 40.82±18.79 HK before, after and 6 hours after the exchange transfusion, respectively.
The results of the bilirubin levels and PAB before, after and 6 hours after the exchange transfusion in 22 jaundiced newborns with high bilirubin (over 17 mg/dL) showed that the average bilirubin decreased after the exchange transfusion. Six hours after, the blood exchange rose again slightly. The average PAB was increased after the exchange transfusion and unlike the short increase in bilirubin, there was still a persistent increase in PAB even 6 hours after the exchange transfusion ( Figure 1 ).
Comparison of mean serum bilirubin changes before blood transfusion after 6 hours after blood transfusion
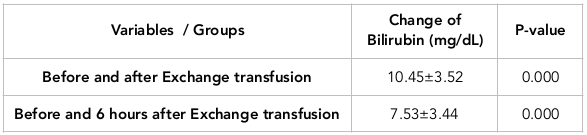
Paired T test results showed that serum bilirubin level before and after the exchange transfusions had a significant difference (P = 0.000). Thus, serum bilirubin level was decreased along with the blood exchange transfusion. Also, the amount of serum bilirubin, after the exchange transfusion was significantly lower than the time before the exchange transfusion (P = 0.000) ( Table 1 ).
Comparison of the mean changes in PAB before the exchange of blood after the exchange of blood and 6 hours after the exchange of blood
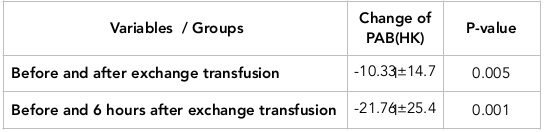
In addition, the amount of PAB after the exchange transfusion significantly increased in comparison to before the exchange transfusion (P = 0.005). The amount of PAB 6 hours after exchange transfusion, compared to before, was significantly different (P=0.001), but the increase of PAB in 6 hours after, more than after the exchange transfusion ( Table 2 ).
Discussion
The results of the study show that Prooxidant-Antioxidant Balance change in favor of Prooxidants after exchange transfusion and even intensifies at six hours after the exchange transfusion. To our knowledge, this is the first study to evaluate the relationship between PAB and the exchange transfusion, especially out to six hours after the exchange transfusion. Based on the results of our study, the exchange transfusion reduces serum bilirubin levels by close to 50%; but 6 hours later due to inter bilirubin from tissues to vasculature, the serum bilirubin level was increased again.
The gold standard after phototherapy for effective treatment of neonatal hyperbilirubinemia is exchange transfusion. Begum et al. (2012) showed that the average serum bilirubin levels before and after exchange were 21.37 and 8.46 mg/dL, respectively. It can be concluded that the exchange transfusion can reduce serum bilirubin by nearly 40% Begum et al., 2012. Based on the results of the study by Ibekwe et al. (2012), serum bilirubin concentrations before and after exchange transfusion were 28.30 and 13.88 mg/dL, respectively Ibekwe et al., 2012.
Bilirubin is a potential physiological antioxidant Ross, 1999 which can prevent the lipoprotein oxidation with low density Stocker et al., 1987. Due to the antioxidant capacity of bilirubin and its ability to potentially associate with peroxyl radicals, any mild increase in blood bilirubin can have a physiological role for protection against some diseases associated with the formation of oxygen and peroxyl radicals Mayer, 2000. The results from a study by Wiedemann et al. showed that total antioxidants have a direct correlation with bilirubin concentrations in term and preterm infants. The study showed the exchange transfusion occurred as reduction of serum bilirubin concentrations reduced plasma antioxidant capacity Wiedemann et al., 2003. Belanger et al. showed the relationship between the reduction of plasma antioxidant capacity (after exchange transfusion) and reduction of serum total bilirubin. Reduction of the antioxidant capacity of the plasma (in addition to reduction of bilirubin) was due to the high blood volume and, therefore, high iron content after the exchange of blood (Belanger et al., 1997).
Based on the results of our study, by reducing 50% of the amount of bilirubin, 50% of the PAB amount increased but at 6 hours later. When increasing bilirubin by 30%, PAB also increased (by 50% again). Increase of PAB after an exchange transfusion seems reasonable but increase of PAB at 6 hours after the exchange was not expected, in spite of the increase in bilirubin. There may be more antioxidant stores in the blood that are removed by exchange transfusion, but there are also oxidant stores in the tissues that quickly return to the blood after replacement, which, even with increasing bilirubin, cannot be corrected. Therefore, it seems that some schemes should be considered for this problem.
The increase of oxidative stress and reduction of antioxidant enzyme activities may lead to cell damage in newborns with hyperbilirubinemia Davutoglu et al., 2008. There is a critical balance between the formation of free radicals and antioxidant defenses in cells and regenerative systems. This means that there is a created balance between antioxidants and peroxides in physiological conditions and that free radicals are neutralized by the antioxidant system. Stressful conditions stimulate the production of free radicals by reducing pairing of oxidation and phosphorylation in the mitochondria, which result in increasing electron leakage and overproduction of superoxide radicals.
When the production of free radicals exceeds the capacity of the antioxidant system for neutralization, lipid peroxidation leads to damaging unsaturated lipids in the cell membrane, amino acids in proteins, and nucleotides in DNA. As a result, the integrity of the cell membrane is disrupted. This situation is intensified by reduction in the efficiency of the immune system, as well as adverse changes in the cardiovascular system, brain, nervous system, and muscle (by increasing lipid oxidation). Therefore, many signs and symptoms may occur to disrupt PAB Boskabadi et al., 2014Boskabadi et al., 2016Georgeson et al., 2002Surai, 2006.
The main limitation of our study was the lack of PAB in the blood given to the infants.
Conclusion
Based on the results of this study, the Prooxidant-Antioxidant Balance is changed in favor of prooxidants in the exchange transfusion and even also intensified at six hours after the transfusion, which may be a sign of the crisis status of oxidants (especially a few hours after the transfusion). In light of these observations, it is deemed advisable that jaundiced infants not be exposed to oxidants after the exchange transfusion; additionally, antioxidant substances may be used.
Abbreviations
G6PD: Glucose 6 Phosphate Deficiency
GSH-Px: glutathione peroxidase
PAB: Prooxidant-Antioxidant Balance
SOD: Superoxide dismutase
STB: Serum total bilirubin level,
TMB: Tetra methyl benzidine
TSH: Thyroid Stimulating Hormone
Author Contribution
Hassan Boskabadi: Dr. Boskabadi conceptualized and designed the study, drafted the initial manuscript, and approved the final manuscript as submitted. Maryam Kalate Mollaei: Kalate Mollaei carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. Maryam Zakerihamidi: Dr Maryam Zakerihamidi designed the data collection instruments, and coordinated and supervised data collection at two of the four sites, critically reviewed the manuscript, and approved the final manuscript as submitted. Majid Ghayour Mobarhan: Dr Ghayour Mobarhan designed the study and carried out the initial analyses, reviewed and revised the manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
References
-
D. H.
Alamdari,
K.
Paletas,
T.
Pegiou,
M.
Sarigianni,
C.
Befani,
G.
Koliakos.
A novel assay for the evaluation of the prooxidant-antioxidant balance, before and after antioxidant vitamin administration in type II diabetes patients. Clinical Biochemistry.
2007;
40(3-4)
:
248-254
.
View Article PubMed Google Scholar -
S.
Begum,
M. A.
Baki,
G.
Kundu,
I.
Islam,
M. K.
Talukdar,
K.
Fatema.
Exchange Transfusion: Indication and Adverse Effect. Bangladesh Journal of Child Health.
2012;
36(1)
:
16-19
.
View Article Google Scholar -
S.
Bélanger,
J.-C.
Lavoie,
P.
Chessex.
Influence of bilirubin on the antioxidant capacity of plasma in newborn infants. Neonatology.
1997;
71(4)
:
233-238
.
View Article PubMed Google Scholar -
V. K.
Bhutani,
A.
Zipursky,
H.
Blencowe,
R.
Khanna,
M.
Sgro,
F.
Ebbesen,
J. E.
Lawn.
Neonatal hyperbilirubinemia and Rhesus disease of the newborn: Incidence and impairment estimates for 2010 at regional and global levels. Pediatric Research.
2013;
74(S1
:
Suppl 1)
.
View Article PubMed Google Scholar -
H.
Boskabadi,
A.
Navaee Boroujeni,
H.
Mostafavi-Toroghi,
G.
Hosseini,
M.
Ghayour-Mobarhan,
D.
Hamidi Alamdari,
G. A.
Ferns.
Prooxidant-antioxidant balance in perinatal asphyxia. Indian Journal of Pediatrics.
2014;
81(3)
:
248-253
.
View Article PubMed Google Scholar -
H.
Boskabadi,
G.
Maamouri,
F.R.
Omran,
S.
Mafinejad,
F.
Tara,
M.P.
Rayman,
M.
Ghayour-Mobarhan,
A.
Sahebkar,
S.
Tavallaie,
M.T.
Shakeri,
M.
Mohammadi.
Effect of prenatal selenium supplementation on cord blood selenium and lipid profile. Pediatrics & Neonatology.
2012;
53(6)
:
334-339
.
-
H.
Boskabadi,
G.
Maamouri,
S.
Mafinejad.
The Effect of Traditional Remedies (Camel’s Thorn, Flixweed and Sugar Water) on Idiopathic Neonatal Jaundice. Iranian Journal of Pediatrics.
2011;
21(3)
:
325-330
.
PubMed Google Scholar -
H.
Boskabadi,
M.
Zakerihamidi,
M.
Heidarzadeh,
A.
Avan,
M.
Ghayour-Mobarhan,
G. A.
Ferns.
The value of serum pro-oxidant/antioxidant balance in the assessment of asphyxia in term neonates. The Journal of Maternal-Fetal & Neonatal Medicine.
2016;
:
1-17
.
PubMed Google Scholar -
C.
Dani,
M. F.
Reali,
G.
Bertini,
E.
Martelli,
M.
Pezzati,
F. F.
Rubaltelli.
The role of blood transfusions and iron intake on retinopathy of prematurity. Early Human Development.
2001;
62(1)
:
57-63
.
View Article PubMed Google Scholar -
M.
Davutoglu,
E.
Guler,
S.
Olgar,
E. B.
Kurutas,
H.
Karabiber,
M.
Garipardic,
H. C.
Ekerbicer.
Oxidative stress and antioxidant status in neonatal hyperbilirubinemia. Saudi Medical Journal.
2008;
29(12)
:
1743-1748
.
PubMed Google Scholar -
G. D.
Georgeson,
B. J.
Szőny,
K.
Streitman,
I. S.
Varga,
A.
Kovács,
L.
Kovács,
A.
László.
Antioxidant enzyme activities are decreased in preterm infants and in neonates born via caesarean section. European Journal of Obstetrics.
2002;
Gynecology
:
and Reproductive Biology
.
View Article PubMed Google Scholar -
O.
Golubnitschaja,
K.
Yeghiazaryan,
M.
Cebioglu,
M.
Morelli,
M.
Herrera-Marschitz.
Birth asphyxia as the major complication in newborns: Moving towards improved individual outcomes by prediction, targeted prevention and tailored medical care. The EPMA Journal.
2011;
2(2)
:
197-210
.
View Article PubMed Google Scholar -
V.
Gopinathan,
N. J.
Miller,
A. D.
Milner,
C. A.
Rice-Evans.
Bilirubin and ascorbate antioxidant activity in neonatal plasma. FEBS Letters.
1994;
349(2)
:
197-200
.
View Article PubMed Google Scholar -
J. M.
Gutteridge,
J.
Stocks.
Caeruloplasmin: Physiological and pathological perspectives. CRC Critical Reviews in Clinical Laboratory Sciences.
1981;
14(4)
:
257-329
.
View Article PubMed Google Scholar -
K.
Hirano,
T.
Morinobu,
H.
Kim,
M.
Hiroi,
R.
Ban,
S.
Ogawa,
T.
Ogihara.
Blood transfusion increases radical promoting non-transferrin bound iron in preterm infants. Archives of Disease in Childhood. Fetal and Neonatal Edition.
2001;
84(3)
:
F188-F193
.
-
R. C.
Ibekwe,
M. U.
Ibekwe,
V. U.
Muoneke.
Outcome of exchange blood transfusions done for neonatal jaundice in abakaliki, South eastern Nigeria. Journal of Clinical Neonatology.
2012;
1(1)
:
34-37
.
View Article PubMed Google Scholar -
J. H.
Lindeman,
E. G.
Lentjes,
E.
Houdkamp,
D.
van Zoeren-Grobben,
J.
Schrijver,
H. M.
Berger.
Effect of an exchange transfusion on plasma antioxidants in the newborn. Pediatrics.
1992;
90(2 Pt 1)
:
200-203
.
PubMed Google Scholar -
M.
Mayer.
Association of serum bilirubin concentration with risk of coronary artery disease. Clinical Chemistry.
2000;
46(11)
:
1723-1727
.
PubMed Google Scholar -
S.
Perrone,
M. L.
Tataranno,
G.
Stazzoni,
G.
Buonocore.
Biomarkers of oxidative stress in fetal and neonatal diseases. The Journal of Maternal-Fetal & Neonatal Medicine.
2012;
25(12)
:
2575-2578
.
View Article PubMed Google Scholar -
R.
Ross.
Atherosclerosis—An inflammatory disease. The New England Journal of Medicine.
1999;
340(2)
:
115-126
.
View Article PubMed Google Scholar -
R.
Stocker,
Y.
Yamamoto,
A. F.
McDonagh,
A. N.
Glazer,
B. N.
Ames.
Bilirubin is an antioxidant of possible physiological importance. Science.
1987;
235(4792)
:
1043-1046
.
View Article PubMed Google Scholar -
P.F.
Surai.
Natural antioxidants in poultry nutrition: new developments. Paper presented at: 16th European Symposium on Poultry Nutrition.
2006
.
-
M.
Turgut,
O.
Başaran,
M.
Cekmen,
F.
Karataş,
A.
Kurt,
A. D.
Aygün.
Oxidant and antioxidant levels in preterm newborns with idiopathic hyperbilirubinaemia. Journal of Paediatrics and Child Health.
2004;
40(11)
:
633-637
.
View Article PubMed Google Scholar -
M.
Wiedemann,
A.
Kontush,
B.
Finckh,
H.-H.
Hellwege,
A.
Kohlschütter.
Neonatal blood plasma is less susceptible to oxidation than adult plasma owing to its higher content of bilirubin and lower content of oxidizable Fatty acids. Pediatric Research.
2003;
53(5)
:
843-849
.
View Article PubMed Google Scholar
Comments

Downloads
Article Details
Volume & Issue : Vol 5 No 3 (2018)
Page No.: 2119-2129
Published on: 2018-03-30
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 7015 times
- Download PDF downloaded - 2037 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress