Abstract
Background: Electroconvulsive therapy (ECT) is a method commonly used in the treatment of psychiatric disorders. As ocular side effects from OCT are less studied and discussed, the aim of this study was to evaluate the profile of the peripapillary retinal nerve fiber layer thickness in patients receiving ECT.
Method: This study was performed on 30 patients who had indication for ECT. After recording demographic data, retinal nerve fiber layer thickness was measured by using spectral domain optical coherence tomography (Heidelberg Engineering, Heidelberg, Germany) of optic nerve head and peripapillary retinal nerve fiber layer.
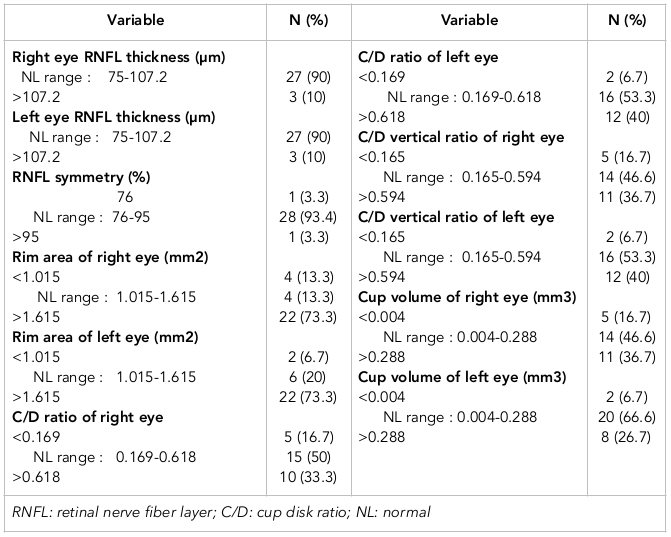
Results: Our results showed that for most of the studied variables, the normal range was observed in less than 85% of patients receiving ECT. Variables which were outside the normal range were: cup disk (C/D) ratio (right and left eyes were 50% and 46.7%, respectively), vertical C/D ratio (right and left eyes were 53.3% and 46.7%, respectively), and cup volume (right and left eyes were 53.3% and 33.3%, respectively).
Conclusion: This study showed that a high percentage of patients receiving ECT had changes in the optic nerve head while intra-ocular pressure in these patients was normal. It is warranted for examiners to pay attention to diagnosis of normal tension glaucoma in patients receiving ECT.
Introduction
Electro-convulsive therapy (ECT) is an electrical current to the brain from the patient for one tenth of a second which produces a major seizure. In other words, the electroshock from two electrodes on the head releases an electrical current to the brain that can lead to a change in brain size Pompili et al., 2014Read and Bentall, 2010. ECT is one of the most effective treatments in psychiatry Mowla et al., 2013. It is an effective short-term treatment for major depression and is probably more effective than drug therapy Group, 2003Khalid et al., 2008. ECT is also an effective psychiatric treatment for mania, catatonic states, and, to a lesser degree, some schizophrenias O'CONNELL, 1982. It generates an epileptic seizure by means of a brief pulse of electrical current under general anesthesia. As noted, it has been used to treat psychiatric disorders Dols and Stek, 2009.
Recently, reports suggest that patients with glaucoma have higher prevalence of depression in contrast to the control group Mabuchi et al., 2008Yochim et al., 2012. Taking this into consideration, it is expected that more and more patients with glaucoma require treatment for their depression and some of these patients with severe depression may require ECT Aneja et al., 2013. For shock therapy, there is a general anesthetic to help prevent muscle contractions due to seizure and bone fractures, and to prevent other side effects such as increased intraocular pressure. Due to increased arterial blood pressure and reduced venous return during electrical shock therapy, it can be expected that intraocular pressure will also increase due to electrical shock therapy Boroojeny et al., 2012.
At present, optical coherence tomography (OCT) is widely used in the diagnosis of optic nerve diseases, especially retinal nerve fiber layer (RNFL). OCT is useful for early diagnosis and evaluation of glaucoma. The OCT device has made clear progress; the most important advancement has been in the Spectoral domain OCT technology. The thickness of RNFL measured with the OCT device is interpreted naturally (or abnormally) using data of RNFL thickness. These data are calculated on a normal basis for each age, and each device has its own data Asl et al., 2014Lashkari et al., 2014Shirzadi et al., 2015.
The aim of this study was to investigate the profile of the optic nerve head and the thickness of the nerve fibers of the peripapillary retina in patients receiving ECT. Additionally, the study aimed to evaluate the adverse effects of ECT on optic nerve head and RNFL pattern.
Materials - Methods
This study was approved by the Ethics Committee of Zahedan University of Medical Sciences in Zahedan, Iran. In this analytical-descriptive study, patients referred to the Baharan Psychiatric Hospital in 2016 and whom were undergoing electro-shock therapy were assessed; 30 patients were selected based on the criteria below.
Inclusion criteria
All patients with major depression, bipolar disorders, catatonia and other acute psychiatric disorders; patients must have undergone more than six courses of ECT for a minimum of three months.
Exclusion criteria
Patients were excluded if they had ocular surgical history, history of glaucoma (for the individual and for his/her family), and/or history or evidence of other eye diseases (e.g. diabetic retinopathy, retinal diseases, uveitis, visual acuity, etc.).
Patients included in the study, along with any caregivers of the patients, were advised by the specialist (physician) about the study and were provided explanations about the process; they were also informed that all clinical information relating to them would remain confidential. Three months after the end of electro-shock therapy, all of the patients were examined by an expert ophthalmologist and their demographic as well as clinical information were recorded. Following that, for all subjects, the optical fiber coherence of the retina was assessed in the peripapillary region using spectral domain OCT (Heidelberg Engineering, Heidelberg, Germany). Images were taken to examine the visual acuity features using the OCT machine. All information was recorded and the necessary analyses were performed.
Statistical analysis
All data were entered into the SPSS version 16.1 software and analyzed using descriptive statistical methods (e.g. statistical tables, determination of central indexes and dispersion) and inferential statistical methods (e.g. mean comparison test with a constant number). As per standard, P<0.05 was considered statistically significant with 95% confidence interval (95%CI).
Results
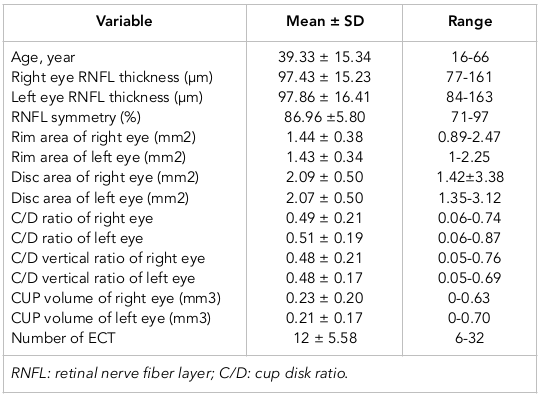
A total of 30 patients including 13 males (43.3%) and 17 females (56.7%) were selected for the study. The mean age of patients was 39.33 years (range, 16-66 years) ( Table 1 ). All patients had undergone ECT for a minimum three months and had received ECT for a total of six times; there was no significant change in the number nor frequency of changes in OCT. The cup/disk ratios of right and left eyes were 0.49±0.21 and 0.51±0.19, respectively; both were in the normal range.
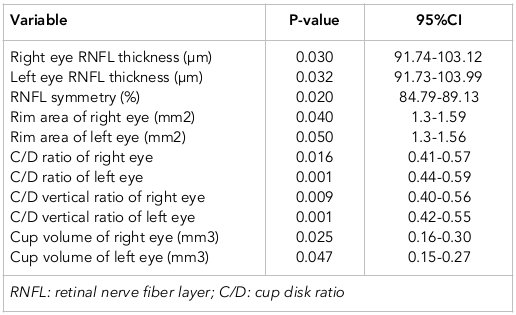
The confidence interval of the studied variables in the patients undergoing ECT is shown in Table 2 . RNFL symmetry (%) between the eyes was 86.96 ± 5.80 (p = 0.020).
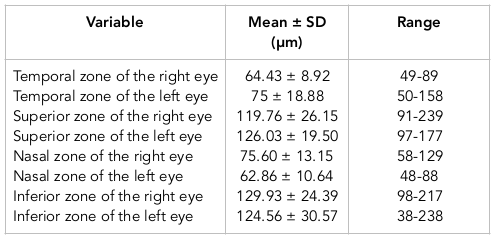
Table 3 shows the mean and range of retinal nerve fiber layer quadrants studied in the patients undergoing ECT. For the right eye, the retinal nerve fiber layer (RNFL) in the inferior zone (129.93 μm) was greater than that of the temporal (64.43 ± 8.92 μm) or superior zone (119.76 ± 26.15 μm). However, for the left eye, the RNFL in the superior zone (126.03 ± 19.50 μm) was greater compared to the other zones. The lowest values were seen in the temporal zone of the right eye (64.43 ± 8.92 μm) and nasal zone of the left eye (62.86 ± 10.64 μm).
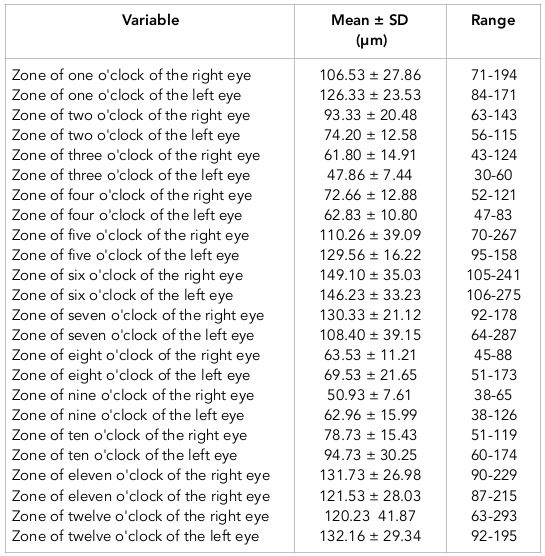
The mean and range of zones of retinal nerve fiber layer o'clock in patients undergoing ECT is shown in Table 4 . The maximum range of zones of retinal nerve fiber layer o'clock was six o'clock in both eyes (right and left eyes were 149.10 ± 35.03 and 146.23 ± 33.23, respectively).
Normal range and percent of patients undergoing ECT for the studied variables are shown in Table 5 . The data show that the frequency of right eye RNFL thickness, left eye RNFL thickness, RNFL symmetry, rim area of right eye, rim area of left eye, cup disk (C/D) ratio of right eye, C/D ratio of left eye, C/D vertical ratio of right eye, C/D vertical ratio of left eye, cup volume of right eye, and cup volume of left eye were 90%, 90%, 93.4%, 13.3%, 20%, 50%, 53.3%, 46.6%, 53.3%, and 46.6%, respectively. About 66.6% patients were in the normal range.
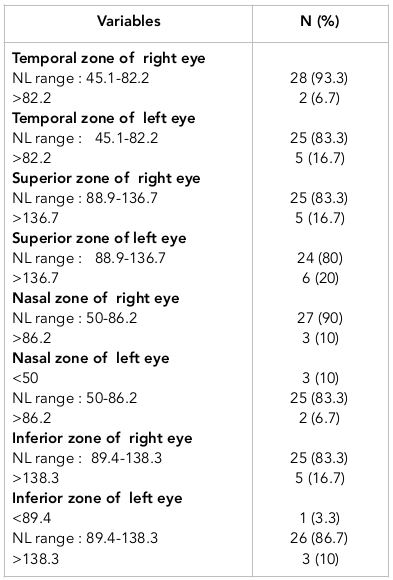
The normal range and percentage of the patients undergoing ECT for retinal nerve fiber layer quadrants are shown in Table 6 . The temporal zone of the right eye, temporal zone of the left eye, superior zone of the right eye, superior zone of the left eye, nasal zone of the right eye, nasal zone of the left eye, inferior zone of the right eye, and inferior zone of the left eye were 93.3%, 83.3%, 83.3%, 80%, 90%, 83.3%, and 83.3%, respectively; about 86.7% patients were normal.
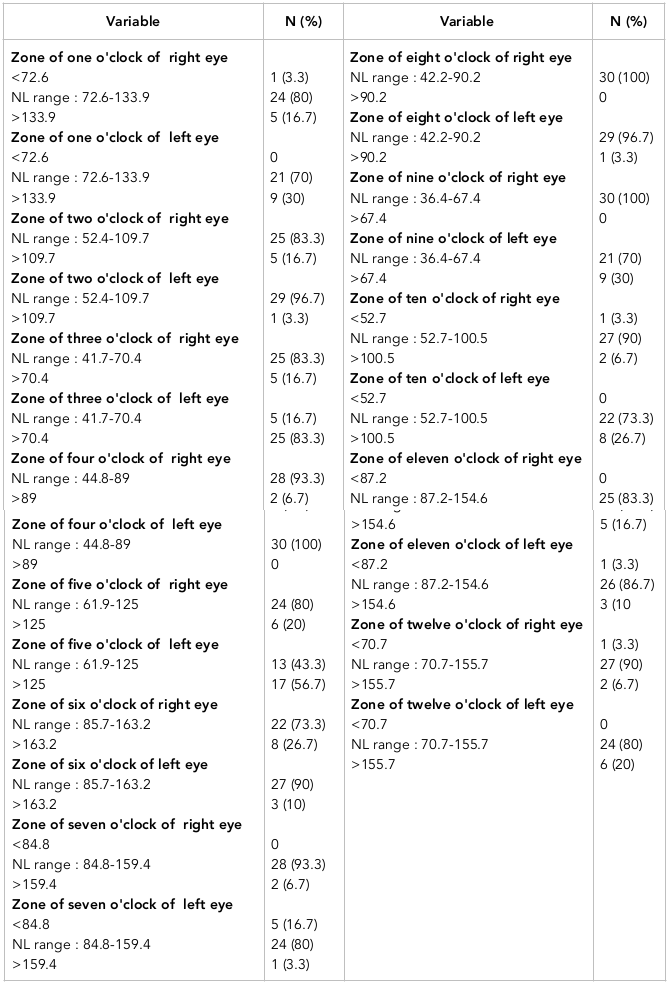
The normal range and percentage of patients undergoing ECT for zones of retinal nerve fiber layer o'clock are shown in Table 7 . As noted, the following were recorded: zone of one o'clock of the right eye, zone of one o'clock of the left eye, zone of two o'clock of the right eye, zone of two o'clock of the left eye, zone of three o'clock of the right eye, zone of four o'clock of the right eye, zone of four o'clock of the left eye, zone of five o'clock of the right eye, zone of five o'clock of the left eye, zone of six o'clock of the right eye, zone of six o'clock of the left eye, zone of seven o'clock of the right eye, zone of seven o'clock of the left eye, zone of eight o'clock of the right eye, zone of eight o'clock of the left eye, zone of nine o'clock of the right eye, zone of nine o'clock of the left eye, zone of ten o'clock of the right eye, zone of ten o'clock of the left eye, zone of eleven o'clock of the right eye, zone of eleven o'clock of the left eye, zone of twelve o'clock of the right eye, zone of twelve o'clock of the left eye were 80%, 70%, 83.3%, 96.7%, 83.3%, 16.7%, 93.3%, 100%, 80%, 43.3%, 73.3%, 90%, 93.3%, 80%, 100%, 96.7%, 100%, 70%, 90%, 73.3%, 83.3%, 86.7%, 90%, and 80% respectively. About 80% of the patients were in normal range.
Discussion
This study evaluated the characteristics of the optic nerve head and peripapillary thickness of the nerve fibers of the retina in patients undergoing ECT. It was found that for most of the variables studied (e.g. retinal nerve fiber layer quadrants, RNFL thickness and RNFL symmetry), the normal range was observed in less than 85% of the subjects. The variables most outside the normal range included the ratio of C/D (50% in the right eye and 53.3% in the left eye), vertical C/D ratio (46.6% in the right eye and 53.3% in the left eye), and cup volume (46.6% in the right eye and 66.6% in the left eye).
Yıldız et al. (2016) checked the efficacy of ECT on the thickness of the optic nerve in Turkey (19 patients had bipolar disorders and 18 were controls) Yıldız et al., 2016. The average RNFL thickness, superior RNFL thickness, and nasal RNFL thickness had significant differences ‘before ECT’ compared with ‘after ECT’. The ECT increased the mean of three variables (RNFL thickness, superior RNFL thickness, and nasal RNFL thickness) but did not have a significant effect on central macular thickness, inferior RNFL thickness, and temporal RNFL thickness. The average RNFL thickness, superior RNFL thickness, and nasal RNFL thickness before ECT compared with the control group showed significant differences; however, we did not have a comparison for ‘after ECT’ and the control group. At the end, the authors concluded that in the patients who underwent ECT, RNFL thickness was similar to the healthy controls. In this study, after intervention, patients undergoing ECT showed greater RNFL thickness than healthy controls.
Boroojeni et al. (2012) evaluated the efficacy of ECT combined to Propofol and Succinylcholine on intraocular pressure Boroojeny et al., 2012. Intracranial base pressure had a significant decrease in patients undergoing ECT plus Propofol, and a significant increase in patients undergoing ECT plus Succinylcholine. In all patients at the one and five minutes compared with before intervention (base pressure), the pressure significantly increased (18.32±3.49 mmHg versus 15.41±3.46 mmHg). However, in 10 minutes the pressure was close to the base pressure (14.68±3.57 mmHg). ECT can increase the intraocular pressure that is not in risk range and, therefore, ECT can be prescribed to patients regardless of their ocular complications.
However, in the present study, intraocular pressure was not measured in patients, but it was found that some indices affected by intraocular pressure increased in patients and it seems that ECT procedure increases the intraocular pressure. Aneja et al. (2013) examined a patient who was suffering from major depression accompanied by psychiatric symptoms, which did not improve with normal symptoms of depression thus requiring an ECT Aneja et al., 2013. On the other hand, it was found that the patient had open angle glaucoma. The patient was subjected to ECT and eventually, the symptoms of the patient improved and did not result in increased eye pressure or eye diseases.
Another study Edwards et al., 1990 showed that intraocular pressure increased significantly after ECT but returned to basic pressure in 90 seconds after ECT was ended. Therefore, the results showed that an increase in intraocular pressure, although not dangerous in the non-glaucomatous eye, can affect eye function and cause recurrent complications in patients with severe glaucoma. However, any increase in intraocular pressure was of a transient nature. Mabuchi et al. (2008) investigated the relationship between anxiety and depression with increasing intraocular pressure Mabuchi et al., 2008; the authors showed that the intraocular pressure in patients with depression and those with anxiety was significantly higher than that of the control group (13% and 1.5%, versus 5.2%, respectively). It was found that intraocular pressure was significantly higher in patients with depression and anxiety who underwent ECT.
One study reported that ECT is associated with a brief rise in intraocular pressure and probably does not cause a significant rise in intraocular pressure in patients with glaucoma Good et al., 2004. Another study described a case of 49-year-old woman treated with ECT for depression, 13 days after phacoemulsification and intraocular lens implantation Sienaert and Vanholst, 2013. That patient had 9 treatments until remission, without any complication. Saad et al. (2000) described two cases; one patient received ECT at 12 days post cataract surgery while the other patient received ECT one week post vitrectomy on one eye (a few years after that she received ECT 2.5 weeks post cataract surgery on the other eye) Saad et al., 2000. There were no complications or adverse events for either patient.
There are four recommendations including: 1) regular monitoring of ophthalmic sign and symptoms, clinical examination and para-clinical tests for rapid and timely identification of ocular side effects in patients before and after treatment with ECT; 2) conduct sessions and provide information to psychiatric practitioners to introduce undesirable effects of ECT on the patients' eyes, and refer patients to ophthalmologists before and after treatment with ECT for diagnosis and supplementary therapies if needed; 3) considering a small number of studies, similar studies are suggested with larger sample sizes; and 4) perform a similar prospective study with regard to the variables studied, before and after ECT intervention and compared with the control group.
Conclusion
The results of this study showed that for most of the variables studied, the normal range was observed in less than 85% of patients undergoing ECT. The variables outside the normal range included C/D ratio, vertical C/D ratio, cup volume in the right eye, cup volume in the left eye, and at 5 o'clock. It was also found that these changes were at the head of the optic nerve and that the intraocular pressure in the patients was normal. It is suggested that examiners should be careful to distinguish these patients from normal torsion glaucoma cases.
Abbreviations
C/D: cup disk
ECT: Electroconvulsive therapy
NL:Normal
OCT: Optical coherence tomography (OCT)
RNFL: Retinal nerve fiber layer
Author Contribution
Kourosh Shahraki & Alireza Khosravi designed the study and contributed to analysis, interpretation of data, and drafting of manuscript. Shiva Kaffashipour collected data. Kianoush Shahraki reviewed and edited the manuscript for intellectual content. Masoud Sadeghi contributed to analysis and interpretation of data and revised the manuscript. All authors gave final approval of the version to be published.
References
-
J.
Aneja,
S.
Grover,
M.
Agarwal,
S.
Kaushik.
Use of Electroconvulsive Therapy in the Presence of GLAUCOMA: A Case Report and Review of Literature. Indian Journal of Psychological Medicine.
2013;
35(1)
:
80-83
.
View Article PubMed Google Scholar -
A.N.
Asl,
A.
Khoshvaghti,
A.
Najafi,
K.
Shahraki,
S.
Molayi.
Evaluation of the intraocular pressure changes after flight with warplanes. Int J Curr res Aca Rev 2014.
2014;
2
:
222-225
.
-
S. B.
Boroojeny,
N. H.
Tabatabai,
B.
Babakhani,
S.
Babakhani,
Z.
Moody.
The effect of electroconvulsive therapy using propofol and succinylcholine on the intraocular pressure . Middle East Journal of Anaesthesiology.
2012;
21(5)
:
713-717
.
PubMed Google Scholar -
A.
Dols.
[Electroconvulsion therapy]. Nederlands Tijdschrift voor Geneeskunde.
2009;
153
:
A588
.
PubMed Google Scholar -
R. M.
Edwards,
A.
Stoudemire,
M. A.
Vela,
R.
Morris.
Intraocular Pressure Changes in Nonglaucomatous Patients Undergoing Electroconvulsive Therapy. Convulsive Therapy.
1990;
6(3)
:
209-213
.
PubMed Google Scholar -
M. S.
Good,
T. J.
Dolenc,
K. G.
Rasmussen.
Electroconvulsive therapy in a patient with glaucoma. The Journal of ECT.
2004;
20(1)
:
48-49
.
View Article PubMed Google Scholar -
M. H.
Lashkari,
K.
Shahraki,
A.
Najafi,
K.
Shirzadi,
S.
Molaei,
K.
Shahraki.
Evaluation of the optic nerve head and peripapillary retinal nerve fiber layer changes in warplanes pilots. Int J Curr Res Aca Rev.
2014;
2(8)
:
217-221
.
-
K.
Shirzadi,
A. R.
Amirdehi,
A.
Makateb,
K.
Shahraki,
K.
Khosravifard.
Studying the effect of tropicamide various concentrations on routine dilation of the pupil. Biomedical & Pharmacology Journal.
2015;
8(2)
:
885-889
.
View Article Google Scholar -
N.
Khalid,
M.
Atkins,
J.
Tredget,
M.
Giles,
K.
Champney-Smith,
G.
Kirov.
The effectiveness of electroconvulsive therapy in treatment-resistant depression: A naturalistic study. The Journal of ECT.
2008;
24(2)
:
141-145
.
View Article PubMed Google Scholar -
F.
Mabuchi,
K.
Yoshimura,
K.
Kashiwagi,
K.
Shioe,
Z.
Yamagata,
S.
Kanba,
S.
Tsukahara.
High prevalence of anxiety and depression in patients with primary open-angle glaucoma. Journal of Glaucoma.
2008;
17(7)
:
552-557
.
View Article PubMed Google Scholar -
A.
Mowla,
F.
Houshmand,
A.
Pani.
A Comparison of the practice of Electro convulsive therapy (ECT) for psychiatry patient in department of psychiatry ,Fatemeh Zahra hospital, Bushehr, Iran 2008-2009. Iran South Med J.
2013;
16(3)
:
260-267
.
-
R.A.
O'CONNELL.
A review of the use of electroconvulsive therapy. Psychiatric Services.
1982;
33
:
469-473
.
-
M.
Pompili,
G.
Dominici,
G.
Giordano,
L.
Longo,
G.
Serafini,
D.
Lester,
P.
Girardi.
Electroconvulsive treatment during pregnancy: A systematic review. Expert Review of Neurotherapeutics.
2014;
14(12)
:
1377-1390
.
View Article PubMed Google Scholar -
J.
Read,
R.
Bentall.
The effectiveness of electroconvulsive therapy: A literature review. Epidemiologia e Psichiatria Sociale.
2010;
19(4)
:
333-347
.
View Article PubMed Google Scholar -
D. A.
Saad,
J. L.
Black,
Krahn
III,
Rummans
L. E..
ECT post eye surgery: Two cases and a review of the literature. The Journal of ECT.
2000;
16(4)
:
409-414
.
View Article PubMed Google Scholar -
P. A.
Sienaert.
Electroconvulsive therapy after eye surgery. The Journal of ECT.
2013;
29(2)
:
139-141
.
View Article PubMed Google Scholar -
UK ECT Review Group..
Efficacy and safety of electroconvulsive therapy in depressive disorders: A systematic review and meta-analysis. Lancet.
2003;
361(9360)
:
799-808
.
View Article PubMed Google Scholar -
N.
Yıldız,
D.
Uçar,
M.
Hepokur,
F.
Baltu,
E.
Guliyev,
H.
Emül.
The alteration of retinal nerve fiber layer thickness after ECT sessions. European Neuropsychopharmacology.
2016;
26
:
S307
.
-
B. P.
Yochim,
A. E.
Mueller,
K. D.
Kane,
M. Y.
Kahook.
Prevalence of cognitive impairment, depression, and anxiety symptoms among older adults with glaucoma. Journal of Glaucoma.
2012;
21(4)
:
250-254
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 12 (2017)
Page No.: 1885-1897
Published on: 2017-12-27
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 5902 times
- Download PDF downloaded - 2116 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress