Abstract
Introduction: The use of fresh human amniotic membrane as an accelerating factor for injury repair has been considered for improvement of various injuries, particularly burns, and has shown significant effects. Perianal surgeries, however, have a high recurrence rate due to the anatomy of the area. Thus, finding an effective method in postoperative care may play an important role in improving the quality of surgical procedures in this area. Considering the high recurrent rate of injury in the perianal region and the need for more effective post-surgical care, this study was aimed at evaluating the effects of using amniotic membrane for wound improvement following perianal surgery in a rabbit model.
Methods: Twenty-four New Zealand white male rabbits were divided into two groups. After the rabbits received anesthesia and perianal surgery, group A rabbits received fresh human amniotic membranes (measuring 1x1 cm) to potentially repair the surgical wounds, while group B rabbits did not receive the membranes. The data were analyzed using t-tests and in order to confirm the normal distribution of data, Kolmogorov-Simonov test was used (P=0.03).
Results: In this study, the Abramov surgical wound scoring system was used to determine the wound improvement rate in all specimens. According to the results, this rate was significantly higher in the group administered with amniotic membrane (group A; P=0.0001).
Conclusion: The use of fresh human amniotic membrane plays an important role in the improvement of perianal surgical wounds in rabbits. Thus, this method may be more effective than other methods without membrane anesthetic surgeries.
Introduction
Nowadays, there is a widespread tendency to use human amniotic membrane as an accelerated wound dressing for wound improvement. The antimicrobial properties, low immune stimulation, high separation power, and ease of access of human amniotic membranes have led many surgeons to use it in research applications Beck et al., 2011Beck et al., 2014Drake et al., 2014Mahajan et al., 2007Mohammadi et al., 2015Smink, 2015. During wound development and subsequent repair of tissue injury, a multitude of events occur to improve healing and accelerate the process of skin and tissue recovery. Repair begins quickly after the emergence of an injury and continues for several weeks. Different conditions or environments can affect injury improvement with respect to speed and quality of the repair.
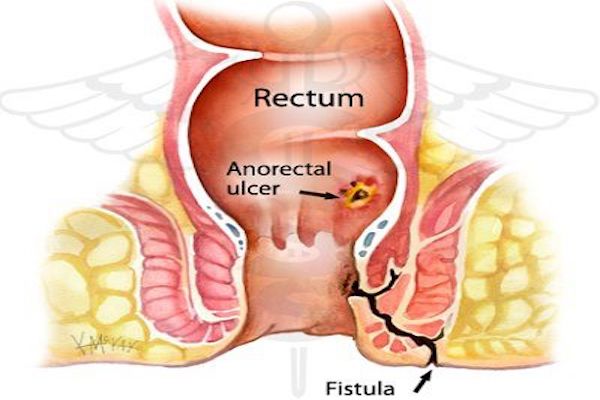
Healing after surgery of the perianal area has always been challenging due to the anatomy of the area; thus, it is important to have an effective method to accelerate healing which not only increases the success rate of the surgery but also patient satisfaction Mahajan et al., 2007Smink, 2015.
This study was designed to determine the effectiveness of using fresh human amniotic membrane, versus the conventional method, to improve the wound in the perianal region of rabbits following perianal surgery.
Materials - Methods
In this study, 24 New Zealand white rabbits (males), with weight ranging from 1500 to 2500 grams, were used. They were approved and housed in the animal laboratory center in Zahedan University of Medical Sciences, Zahedan, Iran in Feb 20116. All animals were initially evaluated by screening tests for any underlying diseases. Each animal was individually kept in a cage and cared for based on the guidelines for animal use at the Institute of Pasteur Institute in Iran.
The study was also approved by the Research Committee of Zahedan University of Medical Sciences and its Animal Maintenance Center. The fresh human amniotic membranes used in this study were prepared from the burn center of Tehran University of Medical Sciences, and preserved in glutaraldehyde solution and then frozen at -20oC for shipping. The operation site of the rabbits was washed after shaving using iodine and alcohol, and rinsed with betadine to reduce probable contamination. For aesthetics of rabbits, diazepam (5 mg/kg) and ketamine (30 mg/kg) were administered via intramuscular injection.
Following anesthesia, the rabbits were randomly divided into two groups of 12. For animals in group A, the surgical wound was closed after perianal surgery by inserting an amniotic membrane (1x1 cm). After cutting the perianal area (length of 1 cm and depth of 1 cm), the amniotic membrane was placed there and the cutting area was then sutured by a wicker thread 3-0. For group B, the same process was performed but without insertion of an amniotic membrane at the cutting area.
The extent of amniotic membrane isolation was carefully controlled; membranes were washed several times with normal saline and 0.05% sodium hypochlorite. On the other hand, the fresh human amniotic membrane was stored after delivery and before use in normal saline serum for 2-10 minutes at a temperature of 24ºC to prevent possible dehydration.
The treatment process was conducted the same way for 14 days for animals in both groups. During this time, each rabbit was kept in a separate cage and had a standard and free diet without any differences. The rabbits were attended to by an experienced animal technician who was blinded to the study groups. Also, during this time, the area was examined for dehiscence, infection and abscess formation, and other daily and possible complications. Finally, after 14 days, all animals were euthanized and several cross-sections were taken from the surgical area. Sections were stained with hematoxylin-eosin and sent as blinded to pathologists to evaluate based on the Abramov scoring system (Marie-Chenôve); this system is based on the incidence of tissue necrosis.
For statistical analysis of data in this study, SPSS version 18 and t-tests were used, with a significance level of the test set at p<0.05. Furthermore, the Kolmogorov-Smirnov test was used to compare the two groups and normal distribution of data (P = 0.03).
Results
All animals in this study survived for 14 days. An emergence of infection occurred in one member of group B, which was resolved after 2 washings with normal saline, and opening and re-suturing the area. Other members of the groups have had no complications during this period.
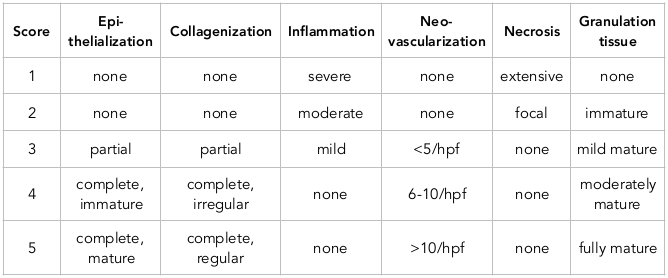
Microscopic assessment and scoring for improvement of the pre-determined surgical wounds were done. The degree of improvement in all specimens was determined based on the amount of epithelialization, collagenization, inflammation, neo-vascularization, necrosis and granulation tissue, according Abramov scoring system Abramov et al., 2007Roshanravan et al., 2014 are summarized in Table 1 .
Analysis of data based on t-test showed that there was a significant histological difference between the mean score of using (17.57±0.787) and without using (14.29±0.488) the fresh human amniotic membrane to improve surgical wounds in the perianal region of the two rabbit groups (P = 0.0001).
Discussion
Nowadays, diverse and scalable care programs are beings studied by physicians around the world for patients undergoing surgery, and their pre- and post-op care. Not only will such programs be effective to accelerate wound healing, they can minimize unwanted complications that surgical patients often face. Standardizing these programs is difficult and a single option may not be adequate Grocott and Pearse, 2012Haller et al., 2011Phipps et al., 2008.
Underlying diseases in the perianal area can lead to surgery. In that anatomical area, due to diseases such as pilonidal cysts and other types of sinuses, the importance of surgery and post-op care is mandatory. However, there is no effective post-surgical care for this area. The most important factor in the postoperative care is the experience of the surgeon. Thus, it is important to determine an effective way to increase the quality of the surgery and reduce the incidences of recurrent injury after operation.
In this regard, this study evaluated the effect of using fresh human amniotic membranes on the extent of wound improvement in rabbits following perianal surgery. The results of this study showed that the use of fresh human amniotic membrane can improve the histology of the wound tissue after perianal surgery.
The exact mechanism of human amniotic membrane in healing is still unclear. However some researchers have suggested that the membrane-associated growth factors may motivate fibroblastic growth and neo-vascularization in that anastomotic site Abramov et al., 2007Roshanravan et al., 2014.
Moreover, the amniotic membrane seems to be an immune-privileged tissue which contains some immunoregulatory factors, such as HLA-G and Fas ligand Kubo et al., 2001. Thus, the rabbit immune system does not reject the amniotic membrane.
In a similar study by Uludag et al., the effect of using an amniotic membrane on colon anastomosis in rats was evaluated. The results showed that use of amniotic membrane could reduce postoperative complications, such as leakage from anastomosis area, intra-abdominal abscesses, intestinal obstruction, and adhesion genesis Uludag et al., 2009. As a result, the authors found that the use of amniotic membrane could also reduce inflammation and lead to improved colon anastomosis histology Uludag et al., 2009Yetkin et al., 2009.
A study by Barlas M et al. determined the effect of using an amniotic membrane on neo-mucosal growth in rabbit ilium terminal; the results showed that using amniotic membrane increasing puberty and reduced irregularities in the intestinal vesicles Barlas et al., 1992. The study of Najipour et al. also determined the effect of using an amniotic membrane in colon astacolosis in dogs. The results of their study showed that the use of amniotic membrane has an effective role in improving the dog colon anastomosis and induced better histological results than the general method Najibpour et al., 2013. Also, in the study by Roshanravan et al, the use of amniotic membrane was evaluated in the recovery of dog rectovaginal fistula; the use of amniotic membrane significantly increased histologic improvement Roshanravan et al., 2014.
Moreover, many studies have focused on determining the effect of amniotic membrane on burn wounds. In these studies, amniotic membrane was shown to play an effective role in the improvement of burn wounds Mohammadi and Johari, 2010Schimidt et al., 2010.
In our present study, there were no prepared microscopic pictures to show histologic improvement, which can be considered as a limitation of the study.
Conclusion
According to the results of the study, fresh human amniotic membrane can play an important role as effective accelerators of healing of perianal wounds. However, more histologic outcomes and studies with larger sample sizes are recommended for further evaluation.
Abbreviations
Hpf: high power field
Author Contribution
Alireza Khazaei: Design of study, proposal of study writing, final content of study. Abdolreza Sotoodeh Jahromi: proposal of study writing, interpretation, final content of study. Hadi okati, Fahimeh Shibak: proposal of study writing, enrolled data, manuscript writing. Masoum Khoshfetrat: Design of study, proposal of study writing, analysis, interpretation, manuscript writing, final content of study. All authors approved the final manuscript.
References
-
Y.
Abramov,
B.
Golden,
M.
Sullivan,
S. M.
Botros,
J. J. R.
Miller,
A.
Alshahrour,
P. K.
Sand.
Histologic characterization of vaginal vs. abdominal surgical wound healing in a rabbit model. Wound Repair and Regeneration.
2007;
15(1)
:
80-86
.
View Article PubMed Google Scholar -
M.
Barlas,
H.
Gökçora,
S.
Erekul,
H.
Dindar,
S.
Yücesan.
Human amniotic membrane as an intestinal patch for neomucosal growth in the rabbit model. Journal of Pediatric Surgery.
1992;
27(5)
:
597-601
.
View Article PubMed Google Scholar -
D. E.
Beck,
P. L.
Roberts,
T. J.
Saclarides,
A. J.
Senagore,
M. J.
Stamos,
Y.
Nasseri.
The ASCRS textbook of colon and rectal surgery. Springer Science & Business Media.
2011
.
-
D. E.
Beck,
S. D.
Wexner,
T. L.
Hull,
P. L.
Roberts,
T. J.
Saclarides,
A. J.
Senagore,
S. R.
Steele.
The ASCRS manual of colon and rectal surgery. Springer Science & Business Media.
2014
.
-
R.
Drake,
A. W.
Vogl,
A. W.
Mitchell,
R.
Tibbitts,
P.
Richardson.
Gray’s Atlas of Anatomy E-Book. Elsevier Health Sciences.
2014
.
-
M.
Grocott,
R.
Pearse.
Perioperative medicine: the future of anaesthesia?. Oxford University Press.
2012
.
-
G.
Haller,
T.
Laroche,
F.
Clergue.
Morbidity in anaesthesia: Today and tomorrow. Best Practice & Research. Clinical Anaesthesiology.
2011;
25(2)
:
123-132
.
View Article PubMed Google Scholar -
M.
Kubo,
Y.
Sonoda,
R.
Muramatsu,
M.
Usui.
Immunogenicity of human amniotic membrane in experimental xenotransplantation. Investigative Ophthalmology & Visual Science.
2001;
42(7)
:
1539-1546
.
PubMed Google Scholar -
M. K.
Mahajan,
V.
Gupta,
S.
Anand.
Evalution of fustulectomy and primary skin grafting in low fistula in Ano. JK science.
2007;
9
:
68-71
.
-
A.A.
Mohammadi,
H.G.
Johari.
Anchoring sutures: Useful adjuncts for amniotic membrane for skin graft fixation in extensive burns and near the joints. Burns.
2010;
36
:
1134
.
-
A. A.
Mohammadi,
B.
Sabet,
H.
Riazi,
A. R.
Tavakko-lian,
M. K.
Mohammadi,
S.
Iranpak.
Human amniotic membrane dressing: An excellent method for outpatient management of burn wounds. Iranian Journal of Medical Sciences.
2015;
34
:
61-64
.
-
N.
Najibpour,
M. B.
Jahantab,
M.
Hosseinzadeh,
R.
Roshanravan,
S.
Moslemi,
S.
Rahimikazerooni,
S. V.
Hosseini.
The effects of human amniotic membrane on healing of colonic anastomosis in dogs. Annals of Colorectal Research.
2013;
1(3)
:
97-100
.
View Article Google Scholar -
D.
Phipps,
G. H.
Meakin,
P. C.
Beatty,
C.
Nsoedo,
D.
Parker.
Human factors in anaesthetic practice: Insights from a task analysis. British Journal of Anaesthesia.
2008;
100(3)
:
333-343
.
View Article PubMed Google Scholar -
R.
Roshanravan,
L.
Ghahramani,
M.
Hosseinzadeh,
M.
Mohammadipour,
S.
Moslemi,
A.
Rezaianzadeh,
S. V.
Hosseini.
A new method to repair recto-vaginal fistula: Use of human amniotic membrane in an animal model. Advanced Biomedical Research.
2014;
3(1)
:
114
.
View Article PubMed Google Scholar -
L. R.
Schimidt,
E. J.
Cardoso,
R. R.
Schimidt,
L. A.
Back,
M. B.
Schiazawa,
A. J.
d’Acampora,
M. V.
Sousa.
The use of amniotic membrane in the repair of duodenal wounds in Wistar rats. Acta Cirurgica Brasileira.
2010;
25(1)
:
18-23
.
View Article PubMed Google Scholar -
D. S.
Smink.
Schwartz’s Principles of Surgery. Annals of Surgery.
2015;
261
:
1026
.
View Article Google Scholar -
M.
Uludag,
B.
Citgez,
O.
Ozkaya,
G.
Yetkin,
O.
Ozcan,
N.
Polat,
A.
Isgor.
Effects of amniotic membrane on the healing of primary colonic anastomoses in the cecal ligation and puncture model of secondary peritonitis in rats. International Journal of Colorectal Disease.
2009;
24(5)
:
559-567
.
View Article PubMed Google Scholar -
G.
Yetkin,
M.
Uludag,
B.
Citgez,
S.
Karakoc,
N.
Polat,
F.
Kabukcuoglu.
Prevention of peritoneal adhesions by intraperitoneal administration of vitamin E and human amniotic membrane. International Journal of Surgery.
2009;
7(6)
:
561-565
.
View Article PubMed Google Scholar
Comments
Downloads
Article Details
Volume & Issue : Vol 4 No 12 (2017)
Page No.: 1867-1873
Published on: 2017-12-26
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Google Scholar
Pubmed
Search for this article in:
Google Scholar
Researchgate
- HTML viewed - 6732 times
- Download PDF downloaded - 2018 times
- View Article downloaded - 0 times
 Biomedpress
Biomedpress