Abstract
Hyalinizing Trabecular Tumour (HTT) is rare among follicular cell neoplasm and contributes less than 1% of all primary thyroid gland tumours. It is commonly seen in middle age with female prepondenrance. HTT is a benign to malignant potential tumour. The tumour has definite histomorphological features. However cytological diagnosis is challenging. The definite cytological diagnosis of HTT is important to plan the surgical treatment. Here we present two case reports; one in 72 years male and other in 22 years female highlighting the pitfalls in the cytological diagnosis of HTT.
Introduction
Hyalinizing Trabecular Tumour (HTT) is rare among follicular cell neoplasm and contributes less than 1% of all primary thyroid gland tumours Gupta et al., 2010Li et al., 2012Thompson, 2011. It is considered as a unique entity. However some consider it as a variant of papillary thyroid carcinoma (PTC). It coexist with PTC and also seen with a variety of thyroid lesion Li et al., 2012Ninan et al., 2011. Majority are benign. A few cases with metastatic deposits in lymph node / lung are reported.
Hence it is considered as tumour of uncertain malignant potential and termed as HTT which is adopted by many Pathologists and WHO Howard et al., 2013Li et al., 2012. The tumour has definite histomorphological features. However cytological diagnosis of this unusual tumour is difficult Santosh et al., 2011. Here we present two case reports; one in 72 years male and other in 22 years female highlighting the pitfalls in the cytological diagnosis HTT.
Case Report 1
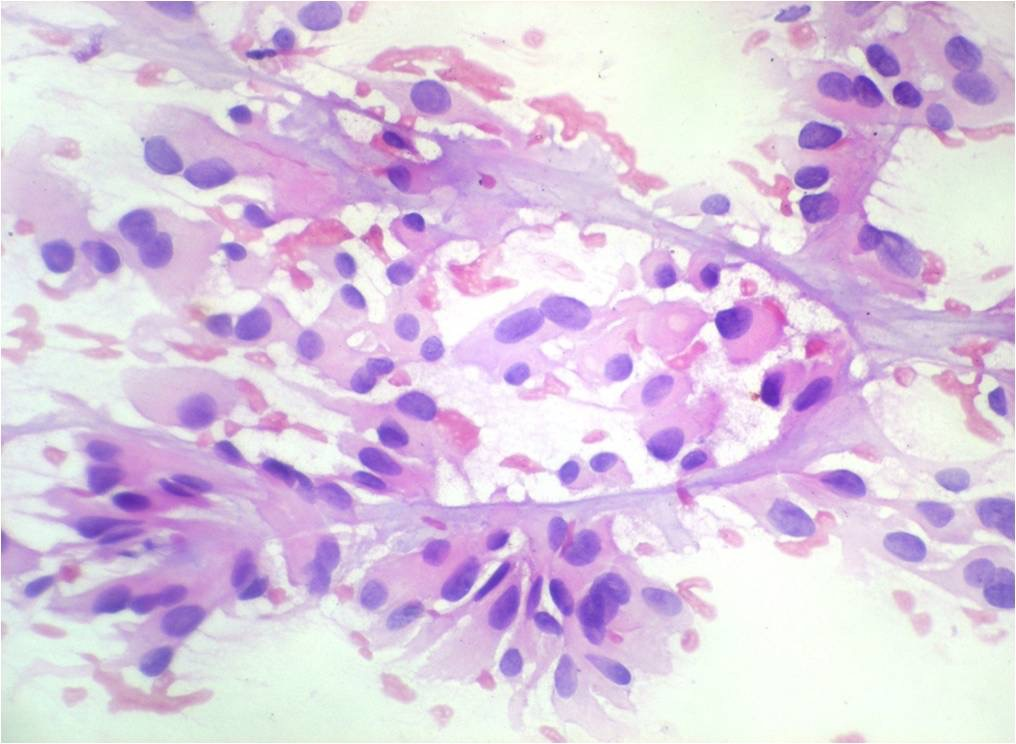
72 year male presented with swelling in the midline of neck, gradually increasing in size since 5 years. No history of pain in swelling or difficulty in swallowing. Patient gives history of Diabetes mellitus and is on treatment since 2 years. Local examination showed a solitary nodule on left lobe of thyroid measuring 8x8 cms. A provisional clinical diagnosis of solitary thyroid nodule was given. Laboratory haematological investigations were within normal limits. Thyroid profile showed; T3 – 1.2 ng/ml, T4 – 7.8 mcg/dl, TSH – 1.76 mcIU/ml and anti- TPO- 10.2 IU/ml. Ultrasound showed a well-defined hypoechoic lesion on left lobe of thyroid measuring 2.5x3.6x4.5 cms with increased vascularity. Right lobe showed 3 hypoechoic well-defined nodules, largest measuring 8x8 cms. A radiological diagnosis of multinodular goitre was offered. Fine needle aspiration cytology (FNAC) of the left lobe of thyroid showed highly cellular smear with follicular cells in sheets and clusters having marked Hurthle cell change. Focal area showed follicular cells in radiating/pallisading pattern around thick hyalinized fibrocollagenous tissue Figure 1 . The background showed erythrocytes and scanty colloid. A cytological diagnosis of Hurthle cell neoplasm was considered.
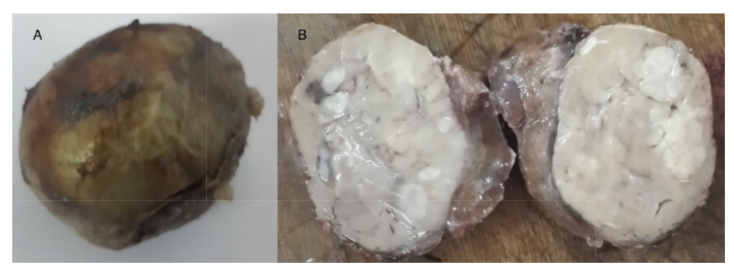
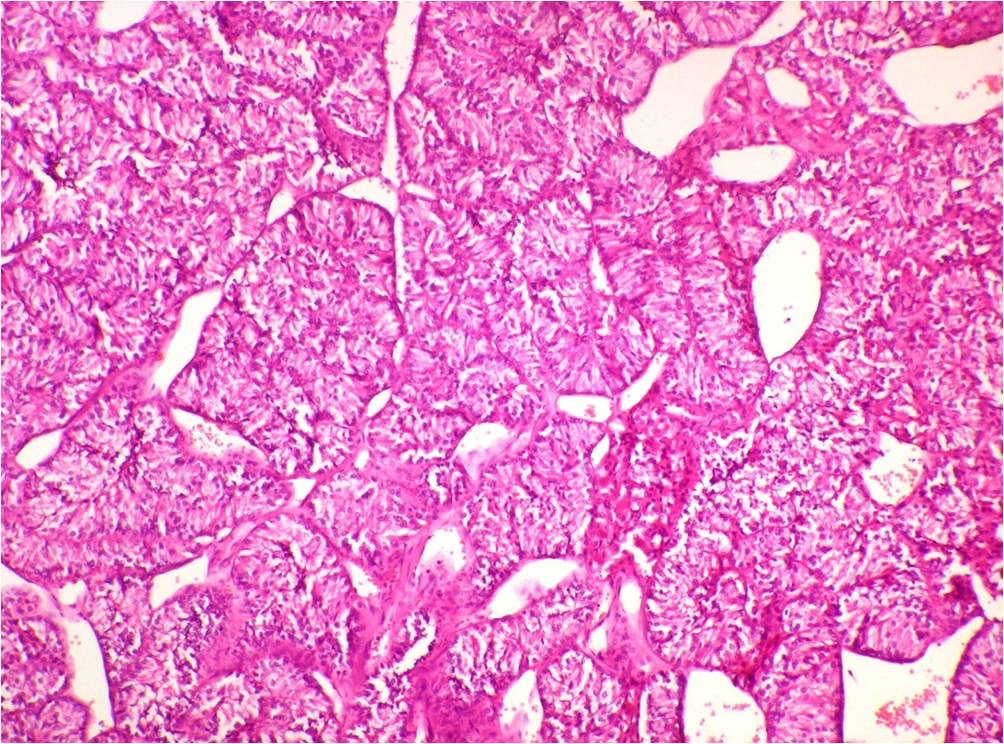
Patient underwent left hemithyroidectomy and specimen was subjected to histopathological examination. Grossly specimen measured 6x5.5x3cm. Cut section showed encapsulated gray white nodular lesion measuring 5x3.5cm with normal thyroid tissue only at one pole Figure 2 . Microscopy showed an encapsulated neoplasm composed of tumour cells arranged in cords/ trabecular pattern and in follicular pattern separated by fibrocollagenous tissue. The nuclei showed longitudinally placed nuclear grooves and occasionally intranuclear inclusions. Cytoplasm was moderate and eosinophilic. The tumour cells showed minimal capsular invasion. However tumour cells had not breached the capsule.
No vascular invasion was noted. The diagnosis of HTT, with uncertain malignant potential was given Figure 3 . Patient was followed for one year and was uneventful.
Case Report 2
22 years female presented with swelling in neck since 4 years with difficulty in breathing. Local examination showed single well defined swelling predominantly in left lobe of thyroid measuring 6x6cm, freely mobile and firm in consistency. A provisional clinical diagnosis of nodular goitre was given.
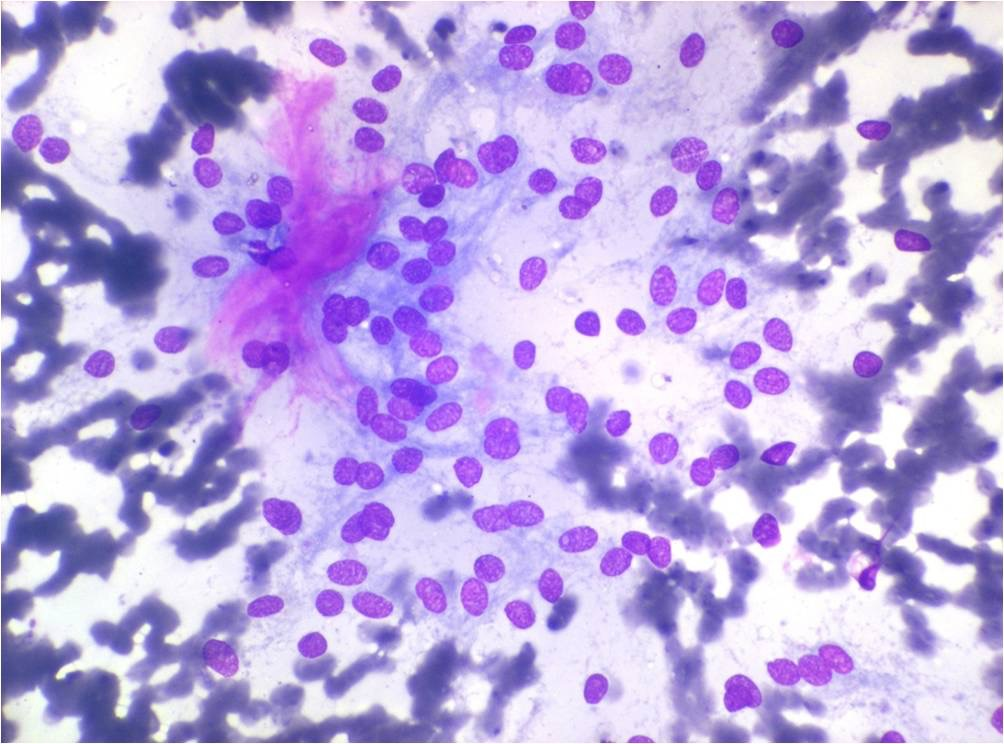
Laboratory investigations were within normal limits. Ultrasound showed unilateral left thyroidomegaly with features of multinodular goitre. FNAC showed satisfactory cell yield consisting of follicular cells having isonucleosis and scanty cytoplasm. Some of the follicular cells showed Hurthle cell change. Background showed colloid and erythrocytes Figure 4
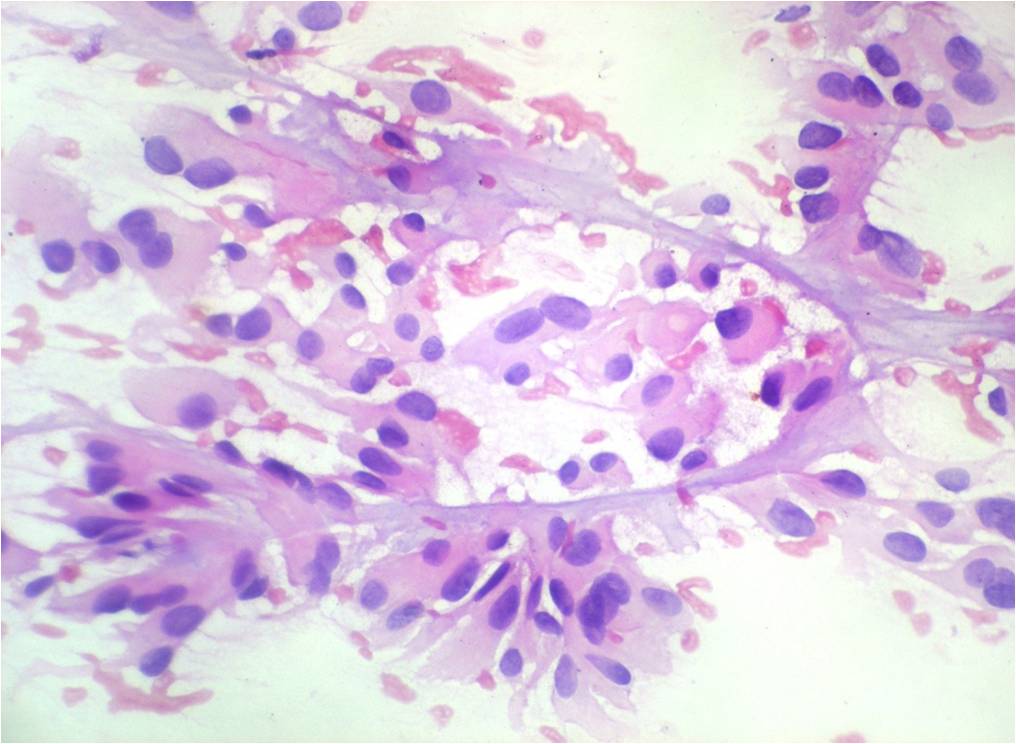
FNAC diagnosis of nodular goitre with Hurthle cell change was given. Patient underwent left hemithyroidectomy and specimen grossly showed single lobe of thyroid measuring 8.5x 5.3x4 cms. External surface showed intact capsule. Cut section was gray white with one area showed cystic degeneration Figure 5 . Microscopy showed an encapsulated tumour consisting of round to oval to spindly cells having fine, granular chromatin, longitudinal nuclear grooves, intranuclear inclusions with moderate to abundant eosinophilic cytoplasm. The cells were predominantly arranged in trabecular pattern with intra and intertrabecular hyaline material. The cells in trabeculae were arranged parallel to each other Figure 6 . A focal area of cystic degeneration was seen. The adjacent thyroid tissue was within normal limits. The tumour did not show capsular/ vascular invasion. A diagnosis of HTT was given. Patient was followed up for 8 months which was uneventful.
Discussion
HTT was originally reported in 1905 Howard et al., 2013. Later it was described in detail about the trabecular growth pattern and marked intratrabecular hyalinizing stroma in 1987 by Carney Casey et al., 2004Gupta et al., 2010Howard et al., 2013Jang et al., 2016Li et al., 2012 McCarthy et al.Ninan et al., 2011Santosh et al., 2011. Various etiological factors are put forth as; radiation exposure, arising in a background of chronic lymphocytic thyroiditis and multinodular goitre (MNG). HTT and lymphocytic thyroiditis are proved to have similar molecular genetics, age and gender distribution.
It can present as solitary/prominent nodule in MNG. There are evidence of possible association with PTC and sometimes considered as variant of PTC due to similar nuclear cytology, immunoprofile and RET oncogene Gupta et al., 2010Li et al., 2012Ninan et al., 2011Thompson, 2011.
HTT are commonly seen in middle age i.e. in 4th and 5th decade of age and are common in females with female:male ratio of 6:1. The tumour presents as asymptomatic/incidental onset or as an incidental finding in a thyroidectomy specimen Gupta et al., 2010Li et al., 2012Ninan et al., 2011Thompson, 2011. In the present case reports, one case is 72 years male and other is 22 years female both presenting as incidental finding.
Cytological diagnosis is challenging. The smears are usually hypercellular with polygonal or elongated spindle cells. Nucleus is hyperchromatic with longitudinally placed grooves, pseudoinclusions (cytoplasmic inclusions), perinuclear halo, perinuclear yellow bodies (represent lysososmes) and fine chromatin without optically clear chromatin.
Cells have low nuclear to cytoplasmic ratio. Cytoplasm is abundant. Cell border is ill defined. Sometimes psammoma bodies are seen. These cells will be arranged in a radial pattern around the hyaline material with vague curved nuclear pallisading. The cells will also arranged in sheets along with hyaline material with lack of papillary pattern and in bloody background Casey et al., 2004Gupta et al., 2010Howard et al., 2013Li et al., 2012 McCarthy et al.Ninan et al., 2011Santosh et al., 2011. The cytological differential diagnoses are PTC and medullary thyroid carcinoma (MTC). HTT is mistaken for PTC because of nuclear features and presence of psammoma bodies. It is mistaken for MTC for the elongated/ spindle cells and the hyaline material. However the hyaline material in HTT is solid/homogenous and well defined than amyloid and not contain the streaked nuclear material as in amyloid. Cells in HTT do not have cytoplasmic granules Gupta et al., 2010Howard et al., 2013Jang et al., 2016 McCarthy et al.. In the present case reports, in the first case the cells showed cytoplasmic features as mentioned above, however the nuclear features were absent and hence the cells were considered as Hurthle cells. The cells were arranged in pallisading pattern around thick hyaline fibrocollagenous tissue which was not accounted. The diagnosis of Hurthle cell neoplasm was given. In the second case a few follicular cells showed Hurthle cell change along with erythrocytes and colloid in background. The arrangement of cells did not show any definite pattern. The diagnosis of nodular goitre with Hurthle cell change was given. In both cases the cells did not show cytoplasmic granules.
The tumor grossly presents as solitary/multiple nodules with average size of 2.5cm. Cut section is well circumscribed/encapsulated usually solitary, solid, yellow tan, lobulated and well defined with foci of calcification. Capsule is thin irregular and uneven Gupta et al., 2010Howard et al., 2013Thompson, 2011.
In the present two cases, both presented as solitary nodule in left lobe of thyroid of more than 2.5 cms size, well defined, encapsulated and gray white on cut surface. Histomorphologically the cells will be polygonal with oval to elongated nuclei (as in cytological feature) with intracellular and extracellular hyaline material. These cells arranged in trabecular, alveolar and in insular pattern. In trabecular pattern, the cells will be seen as straight/pallisading pattern with nuclear grooves perpendicular to the long axis of the trabeculae. Fibrovascular stroma will be seen in intra and intertrabecular areas with marked hyalinization. The hyalinization shows greater deposition at the periphery of the trabeculae. Mitoses are rare. Psammoma bodies may be seen. Usually no vascular/capsular invasion seen Gupta et al., 2010Howard et al., 2013Ninan et al., 2011Thompson, 2011. In the present two cases all the mentioned histomorphological classical features were present. However this shows the poor cyto-histo correlation in the present cases considering cytological diagnosis of HTT. One study has shown the poor performance of even ultrasound guided FNAC in cytological diagnosis of HTT Jang et al., 2016.
The definite diagnosis of HTT is important as it determines the treatment. The treatment of choice for HTT is lobectomy. Misdiagnosis gives rise to mistreatment and total thyroidectomy which is reported in 44-71% of cases.
Cytopathologists should know the cytomorphological features of HTT for precise cytological diagnosis which helps to plan the surgery and avoid surgical overtreatment, postoperative levothyroxine supplementation / radiodine ablation therapy or follow-up with serial thyroglobulin antibody levels. Hence expertise of cytopathologist is very important. Clinicians should be aware that HTT is a benign entity, however it can behave as a potentially malignant tumour Howard et al., 2013Li et al., 2012 McCarthy et al.Thompson, 2011. The prognosis depends on careful screening of tissue sections for vascular, capsular and parenchymal invasion to eliminate the possibility of malignancy Gupta et al., 2010Howard et al., 2013Li et al., 2012.
Conclusion
Even though HTT is a rare entity, one should be aware of this tumour, its presentation and cytomorphological features by which definite cytological diagnosis can be offered and surgery can be planned appropriately.
List of Abbreviations
FNAC: Fine Needle Aspiration Cytology; MNG: Multinodular Goitre; MTC Medullary Thyroid Carcinoma; HTT: Hyalinizing Trabecular Tumour; PTC: Papillary Thyroid Carcinoma; TPO: Thryoid Peroxidase; TSH: Thyroid Stimulating Hormone; WHO: World Health Organization
Author Contribution
Kalyani. R.: Data collection, literature search, concept, manuscript writing, editing and review; Sweta Sinha: Data collection, typing of manuscript.
References
-
M.B.
Casey,
T.J.
Sebo,
J.A.
Carney.
Hyalinizing trabecular adenoma of the thyroid gland identification through MIB-1 staining of fine-needle aspiration biopsy smears. Am J Clin Pathol.
2004;
122
:
506-510
.
-
S.
Gupta,
S.
Modi,
V.
Gupta,
N.
Marwah.
Hyalinizing trabecular tumor of the thyroid gland. Journal of Cytology.
2010;
27
:
63
.
-
B.E.
Howard,
S.H.
Gnagi,
I.T.
Ocal,
M.L.
Hinni.
Hyalinizing trabecular tumor masquerading as papillary thyroid carcinoma on fine-needle aspiration. ORL.
2013;
75
:
309-313
.
-
H.
Jang,
C.K.
Park,
E.J.
Son,
E.K.
Kim,
J.Y.
Kwak,
H.J.
Moon,
J.H.
Yoon.
Hyalinizing trabecular tumor of the thyroid: diagnosis of a rare tumor using ultrasonography, cytology, and intraoperative frozen sections. Ultrasonography.
2016;
35
:
131-139
.
-
J.
Li,
G.-Z.
Yang,
L.-X.
Gao,
W.-X.
Yan,
H.
Jin,
L.
Li.
Hyalinizing trabecular tumor of the thyroid: Case report and review of the literature. Experimental and therapeutic medicine.
2012;
3
:
1015-1017
.
-
S.W.U.
McCarthy,
M.
Koops,
M.L.
Policarpio-Nicolas,
A.A.
Santillan,
S. Hyalinizing
Ahmadi.
Trabecular Tumor: A Diagnostic Challenge in Pathology. In Thyroid Cancer.
;
:
SAT022
.
-
S.
Ninan,
R.
Idris,
P.U.
Telisinghe.
Hyalinising trabecular adenoma of the thyroid. Brunei International Medical Journal.
2011;
7
:
346-349
.
-
K.V.
Santosh,
S.
Raychaudhuri,
H.
Subramanya,
B.J.
Naveen Kumar.
Cytology of hyalinising trabecular adenoma-like variant of medullary thyroid carcinoma. J Cancer Res Ther.
2011;
7
:
189-191
.
-
L.D.
Thompson.
Hyalinizing trabecular adenoma of the thyroid gland. Ear Nose Throat J.
2011;
90
:
416-417
.
Comments
Downloads
Article Details
Volume & Issue : Vol 3 No 11 (2016)
Page No.: 942-950
Published on: 2016-11-12
Citations
Copyrights & License

This work is licensed under a Creative Commons Attribution 4.0 International License.
Search Panel
- HTML viewed - 9772 times
- Download PDF downloaded - 2237 times
- View Article downloaded - 66 times
 Biomedpress
Biomedpress