Right iliofemoral deep venous thrombosis associated with adenomyosis: A case report
- Department of Medicine, Faculty of Medicine, Nguyen Tat Thanh University, 300A Nguyen Tat Thanh Street, Xom Chieu Ward, Ho Chi Minh City, Viet Nam
- Intensive Care Unit, Thong Nhat Hospital, 1 Ly Thuong Kiet Street, Tan Son Nhat Ward, Ho Chi Minh City, Viet Nam
- Vietnamese German Faculty of Medicine, Pham Ngoc Thach University of Medicine, 2 Duong Quang Trung Street, Hoa Hung Ward, Ho Chi Minh City, Viet Nam
- Department of Geriatrics, Faculty of Medicine, Pham Ngoc Thach University of Medicine, 2 Duong Quang Trung Street, Hoa Hung Ward, Ho Chi Minh City, Viet Nam
- Department of Respiratory, Thong Nhat Hospital, 1 Ly Thuong Kiet Street, Tan Son Nhat Ward, Ho Chi Minh City, Viet Nam
Abstract
Introduction: Adenomyosis is typically considered a benign gynecological disorder; however, accumulating evidence suggests an association with thromboembolic complications. This case report highlights the potential development of deep-vein thrombosis (DVT) in patients with adenomyosis, particularly when concurrent estrogen therapy is used, and emphasizes the diagnostic and therapeutic challenges posed by this scenario.
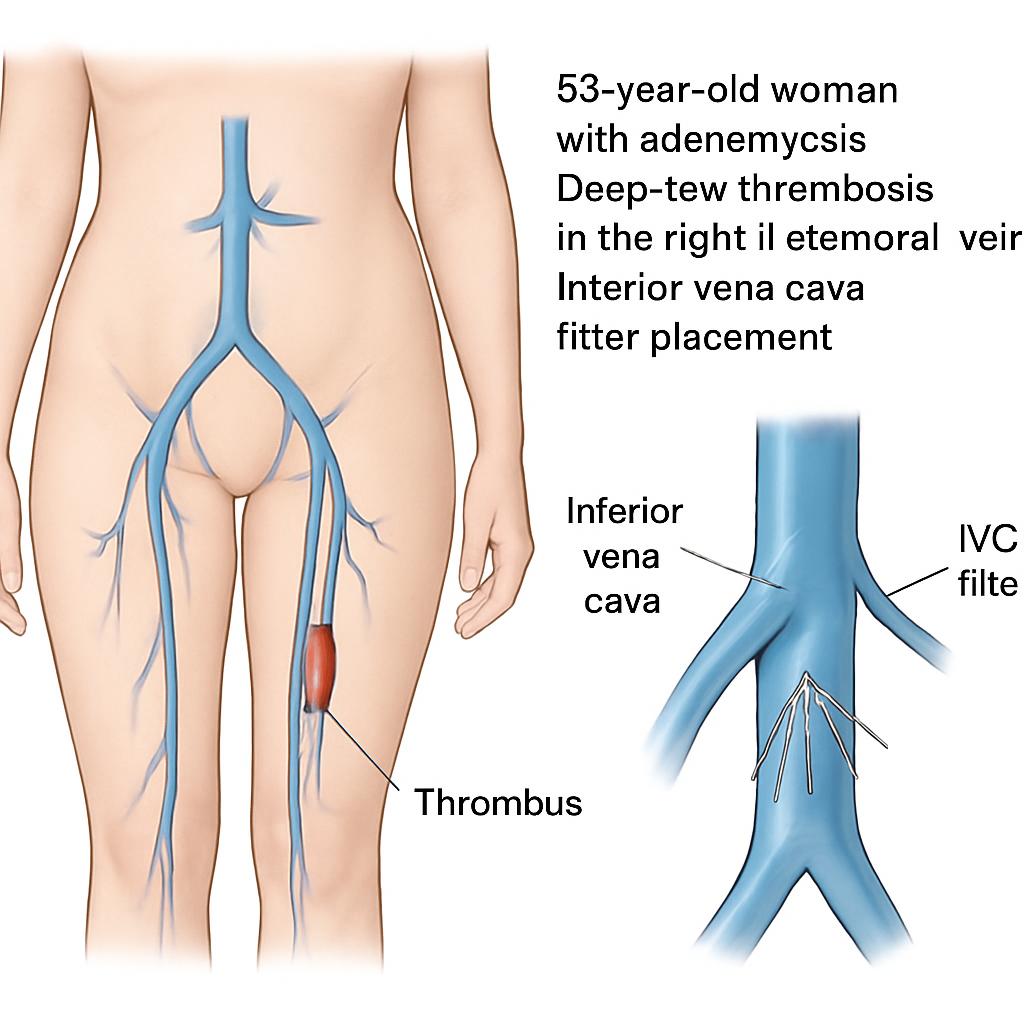
Case Presentation: A 53-year-old woman with histologically proven adenomyosis and chronic menorrhagia presented with right lower-limb pain after prolonged travel. She had recently started estrogen-progestin therapy. On examination, oedema and tenderness were noted in the right calf and groin. Doppler ultrasound confirmed iliofemoral DVT; laboratory findings showed an elevated D-dimer (6.36 µg/mL) and markedly elevated CA-125 (2539.1 U/mL; normal < 35 U/mL). Rivaroxaban was initiated but precipitated heavy vaginal bleeding, necessitating hospital admission, blood transfusion, and temporary discontinuation of anticoagulation. An inferior vena cava (IVC) filter was placed, and she subsequently underwent total hysterectomy with bilateral salpingo-oophorectomy. Post-operative recovery was uneventful, and rivaroxaban was re-introduced.
Conclusions: Adenomyosis is a benign uterine condition that predominantly affects middle-aged, multiparous women. Nevertheless, lower-limb DVT represents a serious complication, especially in patients with adenomyosis and menorrhagia receiving estrogen therapy. Management may require individualized anticoagulation strategies in conjunction with surgical intervention. A multidisciplinary approach is essential for accurate diagnosis, risk stratification, and effective management.
Background
Deep vein thrombosis (DVT) refers to the intravascular formation of a thrombus within the deep veins of the lower extremities, typically precipitated by immobility, vascular injury, or hypercoagulability; if left untreated, it can progress to pulmonary embolism (PE) 1. Adenomyosis is characterized by ectopic endometrial tissue within the myometrium, predominantly affecting middle-aged women and manifesting as menstrual irregularities, menorrhagia, dysmenorrhea, and chronic pelvic pain 2,3. A U.S. population-based study conducted between 2006 and 2015 estimated the annual incidence of adenomyosis at approximately 1.03 % 4. Although histologically benign, adenomyosis has increasingly been associated with venous thromboembolism (VTE), including lower-limb DVT, PE, cerebral venous thrombosis, and multisite thrombosis 5,6,7,8. We describe a 53-year-old woman with adenomyosis who developed right iliofemoral DVT temporally related to estrogen-containing therapy; management included temporary inferior vena cava (IVC) filter placement followed by total hysterectomy. We further discuss potential pathophysiologic mechanisms, therapeutic challenges, and follow-up considerations in this clinical context.
Case presentation
Patient Information
A 53-year-old multiparous Vietnamese woman (gravida 2, para 2; G2P2) was referred for evaluation of acute right lower-extremity pain that began one week after completing a long-distance journey. The pain progressively worsened, radiating along the medial thigh into the right groin. She self-administered acetaminophen and diclofenac without relief. The patient had been diagnosed with adenomyosis in January 2024 and had been receiving combined oral hormonal therapy consisting of ethinylestradiol 0.03 mg plus drospirenone 3 mg daily since June 2024. She also reported chronic menorrhagia and anemia. No relevant family history or previous thrombotic events was documented.
She initially presented to a private clinic, where Doppler ultrasonography of the lower extremities confirmed a right iliofemoral vein thrombosis. Rivaroxaban 15 mg twice daily was prescribed as an induction dose. Two hours after the first dose, the patient developed profuse vaginal bleeding accompanied by dizziness, necessitating admission to Thong Nhat Hospital, a tertiary-care teaching hospital in Viet Nam.
Clinical Findings
Upon presentation, the patient’s vital signs were as follows: blood pressure 120/70 mmHg, heart rate 110 beats per minute (bpm), respiratory rate 20 breaths per minute, and temperature 37.0 °C. Physical examination demonstrated swelling of the right lower extremity with calf and inguinal tenderness. There was no evidence of respiratory distress or neurologic deficits.
Timeline
Clinical timeline of the reported case
| Date | Clinical Event |
|---|---|
| Jan, 2024 | Diagnosis of adenomyosis |
| Jun, 2024 | Initiation of estrogen-progestin therapy |
| Oct 10th, 2024 | Onset of right leg pain post-travel |
| Oct 16th, 2024 |
DVT confirmed by Doppler; CA-125 >2500 U/mL Rivaroxaban initiated → Severe vaginal bleeding → Hospital admission |
| Oct 18th, 2024 | blood transfusion, IVC filter placement |
| Oct 20th, 2024 | Total hysterectomy with bilateral salpingo-oophorectomy |
|
Oct 21st, 2024 Jan, 2025 |
Enoxaparin restarted → Rivaroxaban maintenance CA-125 < 35 U/ml; no residual thrombus on Doppler ultrasonography |
Diagnostic Assessment
Initial laboratory investigations at a private clinic demonstrated a hemoglobin (Hb) concentration of 8.6 g/dL, an elevated D-dimer level of 6.36 μg/mL (reference interval 0.27–1.09 μg/mL), and a markedly raised cancer antigen-125 (CA-125) concentration of 2,539.1 U/mL (reference ≤ 35 U/mL); CA 19-9 remained within the normal range. Doppler ultrasonography performed with a Siemens ACUSON SC2000 PRIME system (Siemens Medical Solutions USA, Inc.) identified thrombosis of the right iliofemoral vein. Subsequent testing at Thong Nhat Hospital recorded a hemoglobin level of 7.0 g/dL and a D-dimer level of 3,180 ng/mL, with otherwise normal coagulation profiles as well as hepatic and renal function tests. A comprehensive evaluation for inherited or acquired thrombophilia (factor V Leiden, prothrombin G20210A, antithrombin, protein C/S, and antiphospholipid antibodies) was not performed during the index admission because of limited test availability. Electrocardiography showed no S1Q3T3 pattern, and transthoracic echocardiography demonstrated no evidence of right ventricular dysfunction.
Therapeutic Intervention
Initial anticoagulation with rivaroxaban 15 mg twice daily resulted in profuse vaginal hemorrhage. The patient required transfusion of four units of packed red blood cells. Because systemic anticoagulation was temporarily contraindicated, an optional inferior vena cava (IVC) filter (ALN, ALN Implants Chirurgicaux, France) was inserted. Definitive surgical management comprised a total hysterectomy with bilateral salpingo-oophorectomy performed at Hung Vuong Obstetrics and Gynecology Hospital. Postoperatively, anticoagulation was reinitiated with enoxaparin 6,000 IU subcutaneously every 12 h for three days, after which therapy was transitioned to rivaroxaban 15 mg once daily for maintenance.
Follow-up and Outcomes
The patient was discharged in a stable condition and scheduled for outpatient follow-up. She subsequently reported a complete resolution of symptoms. At three months post-operatively, the CA-125 concentration had fallen to < 35 U/mL (baseline 2,539.1 U/mL), and Doppler ultrasonography confirmed full resolution of the right iliofemoral deep-vein thrombosis without residual thrombus. Retrieval of an inferior vena cava (IVC) filter is typically recommended within 1–3 months. Owing to the temporary unavailability of retrieval equipment at our institution, the patient will be reassessed for filter removal at the earliest feasible opportunity.
Discussion
We conducted a targeted literature search of PubMed/MEDLINE, Embase, Scopus, and Web of Science from database inception to 31 August 2025, employing the search strategy: “adenomyosis” AND (“deep vein thrombosis” OR “venous thromboembolism” OR “pulmonary embolism” OR “cerebral venous thrombosis”). We also manually reviewed the reference lists of all pertinent publications. Following title-, abstract-, and full-text screening, we identified only case reports and small case series; no randomized controlled trials or large observational cohort studies were retrieved. These observations underscore the rarity of adenomyosis-associated VTE, corroborating previous estimates of fewer than 40 documented cases. A concise summary of reported DVT cases is presented in
Reported cases regarding deep vein thrombosis
| Reported Cases | Ordinal number | Age | Diagnosis and site of DVT | CA 125 (U/ml) | Treatment for VTE | Treatment for adenomyosis | Outcomes |
|---|---|---|---|---|---|---|---|
| Frank Nawroth, et al | 1 | 37 | Left femoral vein thrombosis | - | Oral Vitamin K antagonist | Hysterectomy | Thrombus recurrence after 10 years |
| Akira S, et al | 2 | 34 | Left lower extremity thrombosis | - | - | GnRHa | - |
| Mitsuyoshi Tamura, et al | 3 | 46 | Multiple cerebral infarctions in the left middle cerebral artery territory and deep vein thrombosis in right lower extremity | 1477 | Heparin | Hysterectomy |
No thrombus recurrence during the 16-month follow-up period |
| Xiaolong Zong, et al | 4 | 50 | Distal vein of the right lower extremity thrombosis | 687 | Heparin anticoagulation therapy in 7 days. Rivaroxaban 20mg once daily for two months | Hysterectomy |
No thrombus recurrence during the 6-month follow-up period |
Our case report describes a 53-year-old woman with a history of adenomyosis who had received estrogen–progesterone hormone replacement therapy for two months. She was admitted with pain in the right calf, thigh, and groin after a long-distance trip. Duplex ultrasonography confirmed right iliofemoral deep-vein thrombosis (DVT). Thrombogenesis results from an imbalance between pro-thrombotic and anti-thrombotic pathways, classically summarized in Virchow’s triad of hypercoagulability, venous stasis, and endothelial injury 11. In this patient, the main predisposing factors were estrogen exposure and prolonged travel-related immobility. According to the 2019 European Society of Cardiology (ESC) Guidelines for the Diagnosis and Management of Acute Pulmonary Embolism, oral contraceptives or hormone replacement therapy constitute a moderate-risk factor (odds ratio 2–9), whereas prolonged sitting or travel is considered a weak-risk factor (odds ratio <2) for venous thromboembolism 12. She had no history of trauma, surgery, heart failure, atrial fibrillation, or recent myocardial infarction. Could these two risk factors alone have precipitated thrombosis in this case? A cross-sectional study conducted between July and September 2020 in a Shanghai hospital demonstrated that patients with adenomyosis and menorrhagia exhibited a higher degree of hypercoagulability than those without menorrhagia 13. Moreover, previous studies have documented VTE complications in adenomyosis, including lower-limb DVT, pulmonary embolism, cerebral venous thrombosis, and multisite thrombosis 5,6,7,8.
In our patient, venous stasis may have constituted an additional pathogenic factor, because she presented with diffuse adenomyosis and a uterus enlarged to approximately a 16-week gestational size. A markedly large uterus can compress the right common iliac vein, impeding venous return and facilitating thrombus formation. Recent European Society of Cardiology guidelines have identified adenomyosis as a risk factor for future cardiovascular disease, including stroke and acute myocardial infarction 14. Previous case reports have documented cerebral venous thrombosis, ischemic stroke, pulmonary embolism (PE), and multisite thrombosis involving the brain, kidney, and spleen in patients with adenomyosis 5. Xiaolong Zong et al. demonstrated that patients with CA-125 levels greater than 1000 U/mL have a higher risk of PE, venous thrombo-embolism (VTE), and multisite thrombosis; moreover, those with CA-125 exceeding 1000 U/mL were significantly more likely to experience recurrent thrombosis than patients with CA-125 below 1000 U/mL 5. Our patient presented with a completely occlusive deep-vein thrombosis (DVT) in the right lower extremity and an initial CA-125 level of 2539.1 U/mL, substantially higher than the threshold reported by Xiaolong Zong et al. This finding implies a more severe thrombotic burden than that described in Xiaolong Zong’s report, where the thrombus was limited to the distal veins of the right leg and the CA-125 level was 687 U/mL 6. Nevertheless, she reported no chest pain, dyspnea, headache, visual disturbances, or abdominal pain, and supplementary investigations—including electrocardiography (ECG), transthoracic echocardiography, and abdominal ultrasonography—revealed no evidence of thrombosis at other sites.
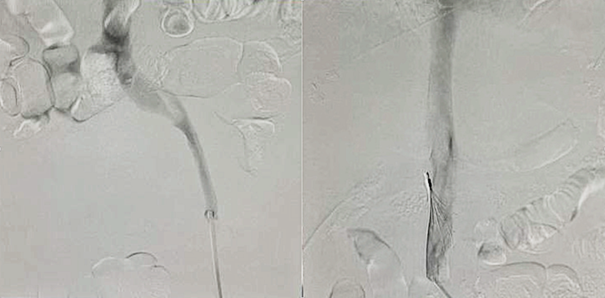
The left photo demonstrates a complete occlusion of the right iliofemoral vein during the intervention. The right photo shows the placement of an inferior vena cava filter.
Therapeutic approaches for adenomyosis-associated VTE or PE are primarily derived from individual case reports. In most descriptions, initial therapy consists of intravenous unfractionated heparin, subsequently replaced by a novel oral anticoagulant (NOAC) or aspirin as maintenance therapy 15,16. Control of adenomyosis itself involves surgical intervention—typically total hysterectomy—or medical management with non-steroidal anti-inflammatory drugs (NSAIDs), hormone replacement with estrogen plus progesterone, or gonadotropin-releasing hormone (GnRH) agonists 17. Because individuals with concurrent adenomyosis and thrombosis generally respond poorly to NSAIDs and must avoid exogenous estrogen owing to the heightened thrombotic risk, most published cases have been treated with either GnRH agonists or definitive hysterectomy after the VTE event.
Our patient could not receive systemic anticoagulation secondary to profound vaginal hemorrhage; therefore, an inferior vena cava (IVC) filter was placed to mitigate the risk of PE. Given the unavailability of GnRH agonists and their delayed onset of action, a total hysterectomy was performed at Hung Vuong Hospital. Anticoagulation was re-initiated on postoperative day 1 with enoxaparin 6,000 IU subcutaneously every 12 h for three days, after which the regimen was switched to rivaroxaban 15 mg/day at discharge. Expert opinion supports extended anticoagulation in patients with CA-125 concentrations > 1,000 U/mL or those with a history of recurrent VTE 5. Although no consensus exists regarding the optimum timing or dosage of anticoagulation following surgery for iliofemoral DVT secondary to adenomyosis, the literature documents heterogeneous strategies ranging from antiplatelet agents to vitamin K antagonists and NOACs. In light of the absence of evidence-based guidelines and the patient’s high bleeding risk, we elected to resume rivaroxaban at the reduced dose of 15 mg once daily, aiming to balance hemorrhagic and thrombotic hazards. The intended duration of therapy was ≥ 3 months, after which Doppler ultrasonography would be performed to evaluate thrombus resolution. If the CA-125 level fell below 1,000 U/mL and no residual thrombosis was detected, discontinuation of anticoagulation would be considered. Retrieval of the IVC filter is generally advocated within three months of placement.
Conclusion
Adenomyosis is a benign uterine disorder that predominantly affects multiparous women in mid-life. Although generally non-life-threatening, it can be complicated by lower-extremity deep-vein thrombosis (DVT), particularly in patients with adenomyosis and menorrhagia who are receiving estrogen therapy. Management may require patient-specific anticoagulation strategies and may also involve definitive surgical intervention. Consequently, a multidisciplinary approach is crucial for accurate diagnosis, risk stratification, and effective evidence-based management.
Abbreviations
bpm: beats per minute; CA 19-9: cancer antigen 19-9; CA-125: cancer antigen 125; D-dimer: cross-linked fibrin degradation product; DVT: deep-vein thrombosis; ECG: electrocardiography; ESC: European Society of Cardiology; G2P2: gravida 2, para 2; GnRH: gonadotropin-releasing hormone; GnRHa: gonadotropin-releasing hormone agonist; Hb: hemoglobin; IU: international unit; IVC: inferior vena cava; NOAC: novel oral anticoagulant; NSAIDs: non-steroidal anti-inflammatory drugs; PE: pulmonary embolism; S1Q3T3: electrocardiographic pattern (S wave in lead I, Q wave and inverted T wave in lead III); VTE: venous thromboembolism
Acknowledgments
None.
Author’s contributions
Conceptualization, H.V.Q. and D.S.H.; methodology, H.V.Q.; software, H.V.Q. and H.V.L.; validation, D.S.H.; investigation, H.V.Q., V.A.D., H.V.L., L.P.N. and D.S.H.; data curation, D.S.H. and L.P.N.; writing—original draft preparation, H.V.Q., V.A.D., H.V.L., L.P.N. and D.S.H.; writing—review and editing, L.P.N. and D.S.H.; visualization, H.V.Q., H.V.L. and V.A.D.; supervision, D.S.H.; project administration, H.V.Q.; All authors have read and agreed to the published version of the manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Declaration of generative AI and AI-assisted technologies in the writing process
The authors declare that they have not used generative AI (a type of artificial intelligence technology that can produce various types of content including text, imagery, audio and synthetic data. Examples include ChatGPT, NovelAI, Jasper AI, Rytr AI, DALL-E, etc) and AI-assisted technologies in the writing process before submission.
Competing interests
The authors declare that they have no competing interests.

